Abstract
Purpose
The aim of this study was to analyze oncologic outcomes after transanal local excision (LE) to ensure adequate surveillance of recurrence in order to treat with curative intent.
Methods
Between January 2000 and June 2009, 102 patients who underwent transanal LE for rectal adenocarcinoma were retrospectively reviewed.
Results
Of the 102 patients, 53 (52.0%) were male. The mean age was 57 ± 11 years. Postoperative pathologic examination revealed 93 cases (91.2%) of pathologic T stage (pT)1 and 9 cases (8.8%) of pT2. Forty-eight patients (47.1%) underwent adjuvant postoperative radiotherapy. The median follow-up interval was 60 months (range, 3 to 146 months). Seven (6.9%) out of 15 patients who suffered recurrence had locoregional recurrence, three (2.9%) had systemic recurrence and five (4.9%) had both systemic and locoregional recurrence. The latter five patients and two of the three patients with systemic recurrence died because of the disease recurrence. On the other hand, only one of the seven patients with locoregional recurrence died because of disease recurrence.
Radical en bloc excision of the rectum and mesorectum, either by abdominoperineal or low anterior resection, is the standard management for rectal cancer. However, in lower rectal cancer, radical resection may lead to permanent stoma, major perioperative morbidity and mortality, and distressing functional outcomes for the patient [1,2]. Therefore, local excision (LE) has been increasingly considered as an alternative to traditional transabdominal resection particularly in lower rectal cancer. Early lower rectal cancer has been treated by LE in a limited proportion of patients, despite the absence of definitive criteria for LE. The problem is that LE of rectal cancer is associated with less satisfactory oncologic outcomes after successful surgery than radical surgery [3]. Local recurrence rates after LE of pathologic T stage (pT)1 and pT2 tumors have been reported in the range of 6.6% to 18.0% and 4.8% to 47.0% (with or without adjuvant therapy), respectively [4-7].
One possible reason for the high local recurrence rate is lymph node involvement. Therefore, accurate assessment of the risk of lymph node metastasis is very important in potential LE candidates. Unfortunately, radiologic methods are inadequate for detecting metastatic lymph nodes. Magnetic resonance imaging (MRI), which is the current choice for preoperative staging in rectal cancer, detects lymph node metastasis with an accuracy of only 43% to 85% [8,9]. As accurate preoperative staging is very difficult with current examining tools, postoperative surveillance is important for detecting tumor recurrence at an early stge. However, few guidelines are available for safe follow-up in patients who undergo LE.
The aim of this study was to analyze the oncologic outcomes after LE to identify suitable methods of surveillance to detect recurrence early in order to with treat with curative intent.
Between January 2000 and June 2009, total 169 patients underwent transanal LE for rectal adenocarcinoma. Of these 169 patients, we excluded 14 with villotubular adenoma with high grade dysplasia, 47 with pTis cancer (intramucosal cancer), and one with pT3 cancer. Five of the remaining 107 patients were also excluded because of indeterminate T stage. However, 35 patients (34.3%) who underwent LE after endoscopic mucosal resection because of indeterminate resection margin or incomplete resection were included. The 102 patients that were left were analyzed retrospectively. We did not include patients who received preoperative chemoradiation therapy. The indication of transanal LE was as follows; a small (<3 cm), mobile, and well to moderately differentiated tumors that were palpated with an index fingertip on digital rectal examination and limited to less than 30% of the rectal circumference and for which there was no evidence of nodal involvement and within T1 stage on transrectal ultrasonography (TUS) and/or MRI.
Before surgery, all patients underwent digital rectal examination, colonofiberscopy, computed tomography (CT) scan, and chest radiography. Tumor location was recorded as the distance from the anal verge to the lower edge of the tumor. TUS was performed on most of the patients except those who underwent endoscopic mucosal resection to evaluate T stage and mesorectal lymph node involvement. Rectal MRI was performed on patients who underwent surgery after 2007.
Surgery was performed under either general or spinal anesthesia. A Foley catheter was inserted before the procedure, and bowel preparation was performed with 4 L of polyethylene glycol on the day before surgery. The procedure was performed in a prone jack-knife position. After identification, the tumor was excised full-thickness with a margin of at least 0.5 cm, and the rectal wall defects were repaired with absorbable sutures.
Patients who were having a tumor infiltrating depth≥ sm2 layer were recommended to receive salvage operation or postoperative adjuvant radiotherapy if they refused to receive radical surgery. Even in the case of sm1 tumors, if the patients had poor prognostic factors such as unfavorable histology (poorly differentiated or mucinous adenocarcinoma), lymphovascular invasion (LVI), and resection margin involvement, salvage operation or adjuvant radiotherapy was also recommended. Postoperative radiotherapy was delivered to the pelvis through three or four fields using 6 or 15 MV from a linear accelerator (Clinac 1800 instrument; Varian Medical Systems, Palo Alto, CA, USA), with all patients in the prone position. The total dose was 50 Gy, with a daily dose of 2 Gy administered on 5 days per week for 5 weeks. The dose of 50 Gy was administered to the whole pelvis. The lateral borders of the pelvic field were 1.5 to 2.0 cm on each side of the widest bony margin of the true pelvic wall. The superior border of the pelvic field was the bottom of L5, and the inferior border was 3 cm distal to the tumor. The anterior border was 3 cm anterior to the tumor, and the posterior border was 1 cm behind the posterior margin of the sacrum. The target volume included the primary tumor, perirectal fat tissue, and the internal iliac and presacral lymph nodes.
Patients received standardized postoperative follow-up, including clinical examinations, complete blood counts, blood chemistry tests, measurements of serum carcinoembryogenic antigen (CEA) concentration, and chest radiography, every 6 months for the first 2 years postoperatively and every 12 months thereafter. They also underwent abdominal and pelvic CT scanning and TUS every 12 months. Colonofiberoscopy or sigmoidofiberoscopy was performed every 6 months after the first postoperative year and then annually thereafter. Patients in whom recurrence was suspected underwent specific examinations (e.g., TUS, CT, MRI, and/or positron emission tomography). Recurrence was diagnosed pathologically by surgical resection or biopsy, and/or radiologically. Local recurrence was defined as recurrence at the LE site, and regional recurrence was defined as a recurrence in the rectal region and/or pelvic lymph nodes. Distant metastasis was defined as any recurrence outside the pelvic cavity.
Statistical analyses were performed using PASW ver. 18.0 (IBM Co., Armonk, NY, USA). Categorical variables were compared using the chi-squared test, and continuous variables were compared using independent sample t-tests. The Kaplan-Meier method was employed to compare disease-free survival rates. All statistical tests were two-sided, and P < 0.05 was considered to be statistically significant.
Of the 102 patients, 53 (52.0%) were male. The mean age was 57 ± 11 years. Postoperative pathologic examination revealed 93 cases (91.2%) of pT1 and 9 cases (8.8%) of pT2. A total of 48 patients (47.1%) underwent adjuvant postoperative radiotherapy. The median follow-up interval was 60 months (range, 3 to 146 months). The overall accuracy of TUS for T staging on these early rectal cancers was 57%; the accuracy was higher for T1 tumors than for T2 tumors (Table 1).
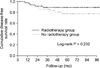
Patients who received postoperative radiotherapy were significantly more likely to have more aggressive T stages and positive resection margins than those who did not. Age, gender distribution, tumor location, serum CEA level, histologic type, and lymphovascular status did not differ significantly between the group receiving postoperative radiotherapy and the group that did not (Table 2). There was no difference in disease free survival between the two groups (Fig. 1).
Of the 102 patients, 15 (14.7%) suffered recurrence of cancer. There was no difference in clinicopathologic characteristics between the patients with and without recurrence except for gender: Females were more frequent among the patients with recurrence than among those without recurrence (12/15 [80.0%] vs. 37/87 [42.5%], P = 0.007). As a result of recurrence, death was more frequent among the patients with recurrence (8/15 [57.1%] vs. 6/87 [6.8%], P < 0.001) (Table 3). Clinicopathologic profiles of recurred patients are summarized in Table 4. Recurrence occurred between 8.4 and 53.4 months. Seven (6.9%) of 15 patients had locoregional recurrence, 3 (2.9%) had systemic recurrence and 5 (4.9%) had systemic and locoregional recurrence. The five latter patients and two of the three with systemic recurrence died from the disease recurrence. On the other hand, only one of the seven patients with locoregional recurrence died from the recurrence. Most of the recurrence was diagnosed by CT scan. However, four out of seven patients with locoregional recurrence were diagnosed by colonofiberscope alone and one patient was diagnosed by digital rectal examination and transrectal ultrasound (Table 4). Recurrence occurred in 12 (12.9%) of the pT1 cases, and in 3 (33.3%) of the pT2 cases (P = 0.098) (Table 5).
Although the oncologic result of LE is significantly inferior to radical surgery in early rectal cancer, LE is still an attractive treatment tool in terms of low-morbidity, good functional outcome, and sphincter-sparing [3,5,10].
Many studies have suggested that careful selection criteria are needed to achieve good oncologic results. The National Comprehensive Cancer Network guidelines recommend the following criteria for LE; <30% circumference of bowel, <3 cm in size, margin clear (>3 mm), mobile and nonfixed, within 8 cm of the anal verge, T1 only, endoscopically removed polyp with cancer or indeterminate pathology, no LVI or perineural invasion, well to moderately differentiated, no evidence of lymphadenopathy on pretreatment imaging. Furthermore, other studies have suggested that the risk factors for nodal involvement are LVI, poorly differentiated, and pT2 in patients with pT1-2 rectal cancer [2]. In the present study, female gender was risk factor for recurrence in univariate analysis. However, T2 stage was more frequently occurred in female than male (8 [16.3%] vs. 1 [1.9%], P = 0.010). In this study, it is likely that female patients did not want to sacrifice their anus as compared with male patients, therefore, to avoid stoma we could not perform radical surgery despite the presence of high risk factors.
Studies of LE with adjuvant radiotherapy have reported
recurrence rates ranging from 8% to 24% and overall survival rates from 77% to 100% [11-13]. Some workers have reported that LE with adjuvant therapy gave better disease-free survival than LE alone [14,15]. In another study overall recurrence and survival rates were similar in patients receiving radiotherapy and those not receiving it, but local recurrence was delayed in the former [16]. In this study, disease-free survival was similar in the LE only group and the LE with radiotherapy group. However, the LE with radiotherapy group were significantly more like to have more aggressive T-stages and positive resection margins. Radiotherapy may have a role as an adjuvant therapy.
Local and systemic recurrence rates vary in different studies, because most of these studies differ in terms of patient selection, tumor staging, surgical techniques, use of adjuvant treatment, and length of follow-up. In this study, eight of 15 patients (pT1, pT2) had systemic recurrence with or without locoregional recurrence and seven patients had locoregional recurrence. Seven of the former patients died because of recurrence whereas only one of the latter patients did so on. Our salvage operation rate was 75% for recurrence of pT1 and 33% for pT2 while in other studies 50% to 100% of the patients with recurrence of pT1 and/or pT2 underwent salvage operation and these studies employed a variety of diverse surveillance procedures (Table 6). Weiser et al. [17] reported that overall survival after salvage operation after long term follow-up was relatively low, considering the early stage of the patients' primary tumors. However, the patients who underwent salvage operation had a more favorable prognosis than those who did not. These results indicate that one aim of surveillance should be the early detection of locoregional recurrence before the development of systemic metastasis. A Guidelines for surveillance protocol after curative resection of colorectal cancer have been presented, and intensive surveillance was preferred to nonintensive surveillance [18]. Salinas et al. [19] also state that aggressive postoperative surveillance should be offered to patients after LE of rectal cancer. Since there are no preoperative tools for accurately predicting recurrence after LE, it is important to carry out aggressive postoperative surveillance to allow for earlier salvage treatments leading to better survival. Some studies have recommended TUS as an effective tool for detecting local recurrence after LE of rectal cancer [20,21]. Furthermore, one group has suggested that MRI should be added to the standard follow-up protocol [21]. We agree about the utility of MRI, provided the cost issue is resolved. In this study, we discovered recurrence mainly by using CT and colonofiberscopy. Therefore, we recommend that follow-up protocols using abdominopelvic CT, chest CT, sigmoidofiberscopy, digital rectal examination and TUS are needed at least every six months for the first five postoperative years. However, the detailed principles of surveillance after LE of rectal cancer remain to be determined.
In conclusion, LE of an early stage rectal adenocarcinoma is followed by a relatively higher recurrence rate. Furthermore, systemic recurrence after LE results in fatal consequences. Therefore, not only is it important to identify ideal candidates for LE, but intensive postoperative surveillance is important as well to identify curable recurrence as soon as possible.
Figures and Tables
Table 1
Comparison of ultrasound T stage (uT) and pathologic T stage (pT) in patients staged with preoperative transrectal ultrasound
Table 2
Clinicopathologic characteristics of patients receiving and not receiving adjuvant radiotherapy

Table 4
Clinicopathologic characteristics of 15 patients with recurrence

pT, pathologic T stage; LVi, lymphovascular invasion; AP, abdominopelvic; CT, computed tomography; S, systemic recurrence; CTx., chemotherapy; D, death; PD, poorly differentiate; CFS, colonofiberscope; Op., operation; WD, well differentiated; R, regional recurrence; CRTx., chemoradiotherapy; MD, moderately differentiated; L, local recurrence; A, alive; DRE, digital rectal examination; TUS, transrectal ultrasound.
ACKNOWLEDGEMENTS
The Asan Institute for Life Sciences (2011-069), the Korea Health 21 R&D Project (A062254), and the Center for Development and Commercialization of Anti-Cancer Therapeutics (A102059), Ministry of Health, Welfare, and Family Affairs, Republic of Korea.
References
1. Beral DL, Monson JR. Is local excision of T2/T3 rectal cancers adequate? Recent Results Cancer Res. 2005. 165:120–135.
2. Chang HC, Huang SC, Chen JS, Tang R, Changchien CR, Chiang JM, et al. Risk factors for lymph node metastasis in pT1 and pT2 rectal cancer: a single-institute experience in 943 patients and literature review. Ann Surg Oncol. 2012. 19:2477–2484.
3. You YN. Local excision: is it an adequate substitute for radical resection in T1/T2 patients? Semin Radiat Oncol. 2011. 21:178–184.
4. Endreseth BH, Myrvold HE, Romundstad P, Hestvik UE, Bjerkeset T, Wibe A, et al. Transanal excision vs. major surgery for T1 rectal cancer. Dis Colon Rectum. 2005. 48:1380–1388.
5. Bentrem DJ, Okabe S, Wong WD, Guillem JG, Weiser MR, Temple LK, et al. T1 adenocarcinoma of the rectum: transanal excision or radical surgery? Ann Surg. 2005. 242:472–477.
6. Garcia-Aguilar J, Mellgren A, Sirivongs P, Buie D, Madoff RD, Rothenberger DA. Local excision of rectal cancer without adjuvant therapy: a word of caution. Ann Surg. 2000. 231:345–351.
7. Sengupta S, Tjandra JJ. Local excision of rectal cancer: what is the evidence? Dis Colon Rectum. 2001. 44:1345–1361.
8. Brown G, Kirkham A, Williams GT, Bourne M, Radcliffe AG, Sayman J, et al. High-resolution MRI of the anatomy important in total mesorectal excision of the rectum. AJR Am J Roentgenol. 2004. 182:431–439.
9. Iafrate F, Laghi A, Paolantonio P, Rengo M, Mercantini P, Ferri M, et al. Preoperative staging of rectal cancer with MR Imaging: correlation with surgical and histopathologic findings. Radiographics. 2006. 26:701–714.
10. Nash GM, Weiser MR, Guillem JG, Temple LK, Shia J, Gonen M, et al. Long-term survival after transanal excision of T1 rectal cancer. Dis Colon Rectum. 2009. 52:577–582.
11. Bailey HR, Huval WV, Max E, Smith KW, Butts DR, Zamora LF. Local excision of carcinoma of the rectum for cure. Surgery. 1992. 111:555–561.
12. Minsky BD, Enker WE, Cohen AM, Lauwers G. Local excision and postoperative radiation therapy for rectal cancer. Am J Clin Oncol. 1994. 17:411–416.
13. Bleday R, Breen E, Jessup JM, Burgess A, Sentovich SM, Steele G Jr. Prospective evaluation of local excision for small rectal cancers. Dis Colon Rectum. 1997. 40:388–392.
14. Taylor RH, Hay JH, Larsson SN. Transanal local excision of selected low rectal cancers. Am J Surg. 1998. 175:360–363.
15. Min BS, Kim NK, Ko YT, Lee KY, Baek SH, Cho CH, et al. Long-term oncologic results of patients with distal rectal cancer treated by local excision with or without adjuvant treatment. Int J Colorectal Dis. 2007. 22:1325–1330.
16. Paty PB, Nash GM, Baron P, Zakowski M, Minsky BD, Blumberg D, et al. Long-term results of local excision for rectal cancer. Ann Surg. 2002. 236:522–529.
17. Weiser MR, Landmann RG, Wong WD, Shia J, Guillem JG, Temple LK, et al. Surgical salvage of recurrent rectal cancer after transanal excision. Dis Colon Rectum. 2005. 48:1169–1175.
18. Jeffery M, Hickey BE, Hider PN. Follow-up strategies for patients treated for non-metastatic colorectal cancer. Cochrane Database Syst Rev. 2007. (1):CD002200.
19. Salinas HM, Dursun A, Klos CL, Shellito P, Sylla P, Berger D, et al. Determining the need for radical surgery in patients with T1 rectal cancer. Arch Surg. 2011. 146:540–543.
20. de Anda EH, Lee SH, Finne CO, Rothenberger DA, Madoff RD, Garcia-Aguilar J. Endorectal ultrasound in the follow-up of rectal cancer patients treated by local excision or radical surgery. Dis Colon Rectum. 2004. 47:818–824.
21. Doornebosch PG, Ferenschild FT, de Wilt JH, Dawson I, Tetteroo GW, de Graaf EJ. Treatment of recurrence after transanal endoscopic microsurgery (TEM) for T1 rectal cancer. Dis Colon Rectum. 2010. 53:1234–1239.
22. Floyd ND, Saclarides TJ. Transanal endoscopic microsurgical resection of pT1 rectal tumors. Dis Colon Rectum. 2006. 49:164–168.
23. Madbouly KM, Remzi FH, Erkek BA, Senagore AJ, Baeslach CM, Khandwala F, et al. Recurrence after transanal excision of T1 rectal cancer: should we be concerned? Dis Colon Rectum. 2005. 48:711–719.
24. Huh JW, Park YA, Lee KY, Kim SA, Sohn SK. Recurrences after local excision for early rectal adenocarcinoma. Yonsei Med J. 2009. 50:704–708.
25. Ramirez JM, Aguilella V, Valencia J, Ortego J, Gracia JA, Escudero P, et al. Transanal endoscopic microsurgery for rectal cancer. Long-term oncologic results. Int J Colorectal Dis. 2011. 26:437–443.
26. Stipa F, Giaccaglia V, Burza A. Management and outcome of local recurrence following transanal endoscopic microsurgery for rectal cancer. Dis Colon Rectum. 2012. 55:262–269.




 ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download