Abstract
Purpose
The safety and the feasibility of performing laparoscopic surgery for rectal cancer after preoperative chemoradiotherapy (CRT) have not yet been established. Thus, the aim of this study was to evaluate the efficacy and the safety of laparoscopic rectal cancer surgery performed after preoperative CRT.
Methods
We enrolled 124 consecutive patients who underwent laparoscopic surgery for rectal cancer. Of these patients, 56 received preoperative CRT (CRT group), whereas 68 did not (non-CRT group). The patients who were found to have distant metastasis and open conversion during surgery were excluded. The clinicopathologic parameters were evaluated and the short-term outcomes were compared between the CRT and non-CRT groups.
Results
The mean operation time was longer in the CRT group (294 minutes; range, 140 to 485 minutes; P = 0.004). In the non-CRT group, the tumor sizes were larger (mean, 4.0 cm; range, 1.2 to 8.0 cm; P < 0.001) and more lymph nodes were harvested (mean, 12.9; range, 0 to 35; P < 0.001). However, there was no significant difference between the two groups in time to first bowel movement, tolerance of a soft diet, length of hospital stay, and postoperative complication rate.
Laparoscopic colon cancer surgery has been accepted worldwide after its oncologic safety was established [1]. Surgeons and patients prefer laparoscopic surgery because of its clinical benefits, such as fast recovery from surgical insult, cosmetic superiority, and short hospital stay [1]. However, laparoscopic rectal cancer surgery is not used by many surgeons despite several prospective studies reporting that laparoscopic surgery is similar to conventional open surgery in terms of oncologic safety [2-5]. The multicenter, prospective randomized trial of the United Kingdom Medical Research Council Conventional versus Laparoscopic-Assisted Surgery in Colorectal Cancer (UK MRC CLASICC) revealed no difference in oncologic outcomes between open and laparoscopic surgery for rectal cancer [5]. Laparoscopic rectal cancer surgery is not as popular as laparoscopic colon cancer surgery because more technical difficulties are associated with it. Thus, laparoscopic rectal cancer surgery requires advanced laparoscopic surgical skills [6]. It is evident that performing laparoscopic surgery in patients with locally advanced rectal cancer is more challenging. So, performing open surgery in some patients with locally advanced rectal cancer is still inevitable despite the clinical benefits of laparoscopic surgery.
Locally advanced rectal cancer has been considered an indication for preoperative chemoradiotherapy (CRT). Preoperative CRT for rectal cancer has been demonstrated to increase the probability of tumor resectability, improve the sphincter preservation rate, decrease the rate of local recurrence, and enhance disease-free and overall survivals [7-10]. However, some surgeons consider performing laparoscopic rectal cancer surgery after preoperative CRT to be neither safe nor feasible because of the technical difficulty of laparoscopic surgery performed with a limited surgical field within the narrow pelvis and tissue fibrosis associated with radiation. Several studies have demonstrated that operating time, blood loss, and postoperative complication rate are increased in rectal cancer surgery after preoperative CRT [11-13]. A recently published, prospective, randomized trial, the Comparison of Open versus laparoscopic surgery for mid and low Rectal cancer After Neoadjuvant chemoradiotherapy (COREAN trial), reported short-term outcomes between open and laparoscopic surgeries for mid or low rectal cancer following preoperative CRT. The trial demonstrated that operation time was longer and blood loss was slightly lower in the laparoscopic group than in the open group. The perioperative complication rates were similar between the two groups (23.5% vs. 21.2%) [14]. However, the trial did not recommend the routine use of laparoscopic rectal resection for mid or low rectal cancer. The safety and feasibility of laparoscopic rectal surgery remain controversial.
In our institute, laparoscopic surgery has been performed for patients with rectal cancer, unless the rectal tumor invaded the perirectal structure. We retrospectively reviewed the clinical data of these patients to assess the short-term outcomes. The aim of this study was to evaluate the efficacy and the safety of performing laparoscopic rectal cancer surgery after preoperative CRT.
From July 2005 to June 2008, 124 consecutive patients underwent laparoscopic surgery for low rectal cancer regardless of preoperative CRT. Of these patients, 56 received preoperative CRT (CRT group), whereas 68 underwent only laparoscopic surgery (non-CRT group). The patients who were found to have distant metastasis at the time of operation and open conversion during operation were excluded. Pretreatment clinical staging was performed using a combination of physical examination, computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography/CT. The indications for CRT were as follows: 1) histologically proven adenocarcinoma of the rectum located within 12 cm of the anal verge, 2) full-thickness rectal cancer (T3 or T4) or node positivity staged by MRI, 3) no evidence of distant metastases, 4) no history of prior radiation therapy to the pelvis, and 5) willingness of the patients to receive CRT.
A standard pathologic examination was performed for all the resected specimens. Each specimen was evaluated for tumor differentiation, depth of tumor penetration, and lymph node metastases. The clinical data were retrospectively collected for age, sex, body mass index, diverting ileostomy, operation time, American Society of Anesthesiologists score, length of hospital stay, and postoperative course.
We clarified the definition of postoperative complications; Wound infection is infection that involves only skin and subcutaneous tissue of this incision; Ileus is temporary delay in gastrointestinal motility after surgery; Anastomotic leakage is characterized by peritonitis (localized or generalized), fecal drainage from wound or drain with presence of abscess or fever; Bleeding is condition for transfusion; Pelvic abscess is characterized by bacterial isolation from the site of infection or purulent material detection; Obstruction is the partial or complete mechanical or nonmechanical blockage of the small or large intestine occurring within the first 30 days after surgery; Bladder dysfunction is the inability to void in the presence of a full bladder; Thromboembolism is deep venous thrombosis and pulmonary embolism after surgery.
The CRT group received a 5-fluorouracil-based chemotherapy regimen preoperatively. Pelvic irradiation in 28 fractions of 180 cGy/day was delivered to the primary tumor for 6 weeks. The radiation field included the gross tumor, the mesorectum, and the internal iliac, presacral, and distal common iliac lymphatics. The upper margin was above the sacral promontory (L5/S1 level), and the lower margin was below 3 cm from the caudal to the gross tumor. Oral capecitabine was given at a dosage of 825 mg/m2 twice daily during the radiotherapy without weekend breaks. Curative surgery was performed 6 to 8 weeks after the completion of the preoperative CRT.
Each patient was placed in a modified lithotomy position with the head and the right side down. An initial 12 mm port was inserted into the abdominal cavity using the open technique, and then pneumoperitoneum was accomplished with carbon dioxide. A standard 10 mm laparoscope was inserted through the 12 mm trocar. Afterward, two 5 mm ports were inserted in the upper right and left abdominal quadrants, and 2 additional 12 mm ports were placed in the lower right and left abdominal quadrants under laparoscopic guidance.
Mobilization of the left side of the colon was performed in the medial-to-lateral direction, until the left ureter was identified. Dissection of the mesocolon was performed at the level of the bifurcation of the aorta. Then, a window was made between the mesocolon and the superior hypogastric nerve plexus. After the dissection of the mesocolon, the inferior mesenteric vessels were divided using endoscopic clips. Total mesorectal excision was performed for the rectal cancers. The rectal transection was performed intracorporeally. An endoscopic linear stapler (Endo Gia Universal Auto Suture, United States Surgical, Norwalk, CT, USA, a subsidiary of Tyco International, Princeton, NJ, USA) was loaded with a 60 mm green cartridge containing 3.5 mm staples, and transection of the rectum was done through the 12 mm trocar in the right lower quadrant. The specimen was extracted through a small incision in the left lower quadrant port, and the wound was covered with a protector. After extracorporeal transection of the proximal bowel, the anvil head of the circular stapler was inserted into the proximal colon and secured with a purse-string suture. The proximal colon was positioned in the abdomen, and the incision site was closed. An end-to-end anastomosis was performed intracorporeally using a circular stapler. Complete anastomosis was confirmed by the air-leak test. A diverting ileostomy was performed in the patients with positive air-leak test. A Jackson-Pratt drain was placed in the pelvis for drainage.
Open conversion cases were excluded, but there were 3 conversions to open (2.36%). Two conversions were in the non-CRT group due to severe adhesion after previous operation (duodenal ulcer perforation, perforated appendicitis), 1 conversion was in the CRT group due to bleeding.
The statistical analysis was performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Two-tailed t-test for continuous variables and the chi-square test for categorical variables were used for statistical comparison of the clinical characteristics. P < 0.05 was considered statistically significant. Qualitative data (2 by 3 data) was analyzed by Fisher's exact test.
The patient characteristics are summarized in Table 1. The CRT group had more male (P < 0.001) and younger patients (P = 0.009) than the non-CRT group. However, there were no significant differences in body mass index, operative type, tumor location, complication rate, diverting ileostomy, histology, pathologic stage and distal resection margin between the two groups. The mean operation time was longer in the CRT group than in the non-CRT group (P = 0.004). In the non-CRT group, the tumors were larger (P < 0.001) and more lymph nodes were harvested (P < 0.001) than in the CRT group.
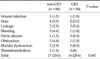
However, there were no significant differences between the two groups in terms of short-term outcomes. The mean time to first day of gas passage was 2.3 days in the non-CRT group and 2.2 days in the CRT group. The mean time to first day of consuming a soft diet was 4.9 days in the non-CRT group and 5.1 days in the CRT group. There were more R0 resections in the non-CRT group than in the CRT group, but this difference was not statistically significant either (97.1% vs. 94.6%, P = 0.87). The total complication rates were not significantly different between the two groups (25.0% vs. 28.6%, P = 0.687) (Table 2). Anastomotic leakage was noted in 2 patients in the non-CRT group and in 3 patients in the CRT group. Bladder dysfunction was more frequent in the CRT group (8.9%) than in the non-CRT group (2.9%).
Preoperative CRT has been accepted as the standard treatment of locally advanced rectal cancer [7-10], as several studies have demonstrated improved local control and reduced toxicity in patients who underwent rectal cancer surgery after preoperative CRT [15,16]. Currently, most tertiary referral hospitals have applied this treatment strategy in patients with locally advanced rectal cancer. However, some of these institutes do not use laparoscopic surgery for locally advanced rectal cancer because of technical difficulties [17], whereas laparoscopic colon cancer surgery has been considered feasible and safe based on the short-term and long-term outcomes [1-4]. Laparoscopic rectal cancer surgery has not been performed worldwide. According to the UK MRC CLASICC trial, high conversion rates to open surgery (34%) and high perioperative morbidity (59%) occurred after laparoscopic rectal cancer surgery [6]. However, several investigators have demonstrated that laparoscopic rectal cancer surgery does not compromise oncologic outcomes when compared with open rectal cancer surgery [18-21], but these studies did not have sufficient sample sizes or include patients who received preoperative CRT. It is evident that performing laparoscopic surgery after preoperative CRT in patients with locally advanced rectal cancer is challenging. Inevitably, open surgery is still performed in some patients with locally advanced rectal cancer who received preoperative CRT despite the short-term outcome benefits of laparoscopic surgery.
Few randomized studies have demonstrated the safety and feasibility of performing laparoscopic surgery after preoperative CRT for locally advanced rectal cancer. The recently conducted COREAN multicenter, prospective, randomized trial demonstrated the safety and the feasibility of performing laparoscopic rectal cancer surgery after preoperative CRT [14]. They reported excellent short-term outcomes in the laparoscopic surgery group when compared with the open surgery group. The times required to pass the first flatus, to resume normal diet, and to pass the first stool were significantly shorter after laparoscopic surgery than after open surgery. In addition, the perioperative complication rates between the two groups were similar (21.2% vs. 23.5%). In our study, all the patients underwent laparoscopic surgery, and short-term outcomes were acceptable. The mean time to first day of flatus was 2.3 days, and the mean time to first day of consuming a soft diet was 5.0 days. Moreover, the overall complication rate was also acceptable. Anastomotic leakage, which is the most serious complication after rectal cancer surgery, was noted in 5 patients (4.0%). One case of anastomotic leakage recovered with conservative management and the others required reoperation with a laparoscopic approach. There was no significant difference in terms of anastomotic leakage between the CRT and non-CRT groups. Previous studies reported much higher anastomotic leakage rates (13.5 to 17%) after laparoscopic rectal cancer surgery than those reported here [22-24]. We did not perform diverting ileostomy routinely, but only did when the air leak test was positive, although re-inforcement sutures were used. Moreover, a single experienced surgeon (JYK) performed all the operations. This may explain the low incidence of anastomotic leakage.
In the current study, each group had different characteristics, including sex, age, operation time, tumor size, and number of harvested lymph nodes. The CRT group had more male and younger patients than the non-CRT group. This result might be attributable to the selection bias because the patients in the non-CRT group were selected according to the patients' refusal to undergo radiotherapy. We find it interesting that the CRT group had a longer operation time, smaller tumor sizes, and fewer numbers of harvested lymph nodes. This may be explained as the effect of the radiation. The radiation tissue sterilization probably influenced fibrosis, shrank the tumor size, and decreased the number of lymph nodes. Furthermore, the pathologic stages did not differ between the two groups. In the CRT group, 55.4% of the patients were classified in pathologic stage 0 and I, although this group did not include the patients in clinical stage I. This finding was explained by the radiation down-staging effect.
We compared the short-term outcomes between the two groups. The postoperative hospital courses were not different between the two groups. Our data suggest that the preoperative CRT did not compromise the short-term outcomes in the patients who underwent laparoscopic rectal cancer surgery. The postoperative complications were also not different between the two groups, and there was no postoperative mortality. In a similar study conducted by Akiyoshi et al. [25], it was documented that postoperative complications were not significantly different between the CRT and non-CRT groups (20.0% vs. 11.4%) (P = 0.432). Our data were consistent with those of Akiyoshi et al. [25]. However, reoperation was required in 4 patients with anastomostic leakage, and most complications were treated in a conservative manner. In our data, the incidence of bladder dysfunction was higher in the CRT group than in the non-CRT group. We postulated that radiation might have adverse effects on the autonomic nerves and consequently result in bladder dysfunction. However, Garlipp et al. [26] demonstrated that preoperative CRT was not a risk factor for bladder dysfunction after undergoing a sphincter preserving rectal resection. The relationship between preoperative CRT and bladder dysfunction has not been established.
Several limitations of the present study have to be mentioned. First, this was a retrospective study, and thus, the study group was not randomized. Long-term follow-up is required to evaluate the oncologic safety of laparoscopic surgery after preoperative CRT. Second, all the operations were conducted by a single experienced surgeon. Therefore, a multicenter trial is needed to assess the safety and the feasibility of laparoscopic surgery for rectal cancer after preoperative CRT based on short-term outcomes. Third, as previously mentioned, selection bias might have existed because the sex ratios and the ages were significantly different between the two groups. This is a weakness of retrospective studies. However, we believe that laparoscopic surgery following preoperative CRT is safe and feasible in terms of the short-term outcomes, if performed by well experienced laparoscopic surgeon.
References
1. Laparoscopically assisted colectomy is as safe and effective as open colectomy in people with colon cancer Abstracted from: Nelson H, Sargent D, Wieand HS, et al; for the Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004; 350:2050-2059. Cancer Treat Rev. 2004. 30:707–709.
2. Colon Cancer Laparoscopic or Open Resection Study Group. Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009. 10:44–52.
3. Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taura P, Pique JM, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002. 359:2224–2229.
4. Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS, et al. Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet. 2004. 363:1187–1192.
5. Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, et al. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007. 25:3061–3068.
6. Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005. 365:1718–1726.
7. Han N, Galandiuk S. Induction chemoradiation for rectal cancer. Arch Surg. 2006. 141:1246–1252.
8. Kuo LJ, Liu MC, Jian JJ, Horng CF, Cheng TI, Chen CM, et al. Is final TNM staging a predictor for survival in locally advanced rectal cancer after preoperative chemoradiation therapy? Ann Surg Oncol. 2007. 14:2766–2772.
9. Sauer R, Becker H, Hohenberger W, Rodel C, Wittekind C, Fietkau R, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004. 351:1731–1740.
10. Shivnani AT, Small W Jr, Stryker SJ, Kiel KD, Lim S, Halverson AL, et al. Preoperative chemoradiation for rectal cancer: results of multimodality management and analysis of prognostic factors. Am J Surg. 2007. 193:389–393.
11. Enker WE, Merchant N, Cohen AM, Lanouette NM, Swallow C, Guillem J, et al. Safety and efficacy of low anterior resection for rectal cancer: 681 consecutive cases from a specialty service. Ann Surg. 1999. 230:544–552.
12. Konishi T, Watanabe T, Kishimoto J, Nagawa H. Elective colon and rectal surgery differ in risk factors for wound infection: results of prospective surveillance. Ann Surg. 2006. 244:758–763.
13. Marijnen CA, Kapiteijn E, van de Velde CJ, Martijn H, Steup WH, Wiggers T, et al. Acute side effects and complications after short-term preoperative radiotherapy combined with total mesorectal excision in primary rectal cancer: report of a multicenter randomized trial. J Clin Oncol. 2002. 20:817–825.
14. Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol. 2010. 11:637–645.
15. Swedish Rectal Cancer Trial. Improved survival with preoperative radiotherapy in resectable rectal cancer. N Engl J Med. 1997. 336:980–987.
16. Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 2001. 345:638–646.
17. Yamamoto S, Fujita S, Akasu T, Moriya Y. Safety of laparoscopic intracorporeal rectal transection with double-stapling technique anastomosis. Surg Laparosc Endosc Percutan Tech. 2005. 15:70–74.
18. Gouvas N, Tsiaoussis J, Pechlivanides G, Tzortzinis A, Dervenis C, Avgerinos C, et al. Quality of surgery for rectal carcinoma: comparison between open and laparoscopic approaches. Am J Surg. 2009. 198:702–708.
19. Lujan J, Valero G, Hernandez Q, Sanchez A, Frutos MD, Parrilla P. Randomized clinical trial comparing laparoscopic and open surgery in patients with rectal cancer. Br J Surg. 2009. 96:982–989.
20. Sileri P, Sthory R, McVeigh E, Child T, Cunningham C, Mortensen NJ, et al. Adhesions are common and costly after open pouch surgery. J Gastrointest Surg. 2008. 12:1239–1245.
21. Zhou ZG, Hu M, Li Y, Lei WZ, Yu YY, Cheng Z, et al. Laparoscopic versus open total mesorectal excision with anal sphincter preservation for low rectal cancer. Surg Endosc. 2004. 18:1211–1215.
22. Barlehner E, Benhidjeb T, Anders S, Schicke B. Laparoscopic resection for rectal cancer: outcomes in 194 patients and review of the literature. Surg Endosc. 2005. 19:757–766.
23. Leroy J, Jamali F, Forbes L, Smith M, Rubino F, Mutter D, et al. Laparoscopic total mesorectal excision (TME) for rectal cancer surgery: long-term outcomes. Surg Endosc. 2004. 18:281–289.
24. Morino M, Parini U, Giraudo G, Salval M, Brachet Contul R, Garrone C. Laparoscopic total mesorectal excision: a consecutive series of 100 patients. Ann Surg. 2003. 237:335–342.
25. Akiyoshi T, Kuroyanagi H, Oya M, Konishi T, Fukuda M, Fujimoto Y, et al. Safety of laparoscopic total mesorectal excision for low rectal cancer with preoperative chemoradiation therapy. J Gastrointest Surg. 2009. 13:521–525.
26. Garlipp B, Ptok H, Schmidt U, Meyer F, Gastinger I, Lippert H. Neoadjuvant chemoradiotherapy for rectal carcinoma: effects on anastomotic leak rate and postoperative bladder dysfunction after non-emergency sphincter-preserving anterior rectal resection. Results of the Quality Assurance in Rectal Cancer Surgery multicenter observational trial. Langenbecks Arch Surg. 2010. 395:1031–1038.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download