Abstract
Purpose
Laparoscopic fundoplication is considered the standard surgical treatment for gastroesophageal reflux disease (GERD) in Western countries. However, some patients experience poor surgical outcomes with this procedure. The study aimed to identify the predictive factors of the surgical outcomes of laparoscopic Nissen fundoplication for the treatment of Korean GERD patients.
Methods
Sixty-one patients with GERD were treated using laparoscopic Nissen fundoplication between November 2012 and February 2015. Symptom control rates were compared according to clinical and surgical factors to identify predictive factors of successful surgical outcomes.
Results
Thirty-five men and 26 women were enrolled. Preoperatively, typical symptoms were present in 60 patients (98%), while atypical symptoms were present in 40 patients (66%). Postoperatively, typical symptoms were controlled in 51 of 60 patients (85.0%), while atypical symptoms were controlled in 33 of 40 patients (82.5%). Overall, at 6 months postsurgery, 54 (88.5%) reported some resolution of GERD symptoms, with 48 (78.7%) achieving complete control. Patients who exhibited a good response to proton pump inhibitor therapy had a significantly greater rate of complete symptom control (P = 0.035).
Gastroesophageal reflux disease (GERD) is caused by chronic exposure of the esophagus to gastric contents, which reduces quality of life and results in various complications [1]. GERD is one of the most common benign diseases of the upper gastrointestinal tract in Western countries, with a prevalence ranging from 10% to 20%, while the prevalence is 4.3% to 15.7% in East Asian countries [2]. Laparoscopic fundoplication is advocated for the treatment of GERD and is regarded as an alternative treatment option in Western countries. Several randomized studies have documented a better or similar effect with laparoscopic fundoplication compared with long-term treatment using a proton pump inhibitor (PPI), with curative or significant improvement in symptoms reported in 85% to 90% of patients [34567].
However, while most patients have excellent outcomes with antireflux surgery, the outcomes of this procedure in some patients are unsatisfactory. Therefore, especially in Korea where antireflux surgery is not a common treatment modality for GERD and the therapeutic mainstay is still long-term treatment with PPI, many gastroenterologists and surgeons remain uncertain about the indications and efficacy of this procedure. In this study, we sought to identify predictive factors of the outcomes of antireflux surgery that could facilitate appropriate patient selection for the surgical treatment of GERD.
This study was approved of Institutional Review Board of Chung-Ang University Hospital (C2016113(1856)).
We identified 61 consecutive patients who underwent primary laparoscopic Nissen fundoplication for the treatment of GERD from November 2012 to February 2015 at Chung-Ang University Hospital, Korea. None of the patients had undergone prior gastric or esophageal operations. The medical records of the study patients were reviewed retrospectively. Patient information including demographic data, preoperative presentation of symptoms, preoperative evaluation, surgical procedure, surgery outcome, complications, and postoperative symptoms was recorded.
For symptomatic evaluation, patients were asked to report any GERD symptoms they had experienced, including frequency and severity of symptoms. Typical (heartburn and regurgitation) and atypical symptoms were reported separately. Information on duration of GERD symptoms and use of PPI therapy was also collected.
At 6 months after surgery, postoperative GERD symptom resolution was scored as poor, fair, good, or excellent for typical and atypical symptoms. The response “good” was regarded as partial symptom control, while “excellent” was regarded as complete symptom control. Symptom control for the individual patient was defined as complete control when all GERD symptoms including typical and atypical symptoms were improved and partial control when one of the 2 types of symptoms was not improved. Complete symptom control rates were compared to identify predictive factors of successful surgical outcomes according to clinical and surgical factors including age, sex, body mass index (BMI), presence of atypical symptoms, hiatal hernia status, esophagitis on endoscopy, results of pH monitoring and upper gastrointestinal barium studies, duration of symptoms, response to PPI therapy, and surgeon experience.
Adverse symptoms after antireflux surgery consisted of dysphagia, difficulty belching, gas bloating, and flatulence and were scored using a 5-point scale (no symptom, mild, moderate, severe, and very severe). The prevalence of adverse symptoms (no symptoms/any symptoms including mild grade) was evaluated at discharge and again at 6 months after surgery.
Indications for surgery included proven GERD with failed medical treatment, complications of GERD (esophageal stricture, esophageal ulcer, and/or Barrett esophagus), extraesophageal symptoms (laryngopharyngeal and/or respiratory symptoms), and a preference for surgical treatment in order to avoid the need for lifelong medical treatment.
Laparoscopy was initially employed in all patients. Patients were placed in the reverse Trendelenburg position with the legs abducted. The surgeon stood between the patients' legs. For most cases, a total of five trocars were used. The first trocar for the camera was inserted transumbilically using an open technique. Four additional ports, namely, left midclavicular (5 mm) for the surgeon's right hand, subxiphoid (5 mm) for the surgeon's left hand, right midclavicular (5 mm) for retraction of the left lobe of the liver, and left anterior axillary (5 mm) for retraction of the stomach by the assistant surgeon were inserted under direct vision.
The initial step of the procedure was the division of the gastrohepatic omentum overlying the caudate lobe of the liver. Beginning at the edge of the right crus, circumferential mobilization of the esophagus was performed with careful dissection using ultrasonic shears (Harmonic scalpel ACE, Ethicon Endosurgery, Cincinnati, OH, USA) to obtain a length of at least 4 cm of the esophagus in the abdomen. For large hiatal hernias, we performed a full dissection of the hiatal hernia sac from the mediastinum, with complete reduction of the sac contents into the abdomen. An umbilical tape was placed around the esophagogastric junction and used for retraction. Short gastric vessels were divided in all cases to clear the greater curvature of the fundus. An esophageal lengthening procedure was not used for any of the patients in this study. Hiatus defects were repaired with interrupted sutures using nonabsorbable thread (2–0 Ethybond, Ethicon, Somerville, NJ, USA). Sutures were placed posterior to the hiatus, and when necessary, supplemented with additional anterior sutures to achieve adequate closure. None of the cases involving a large hiatal hernia involved the use of prosthetic mesh. A tension-free, loose, 360° gastric fundic wrap (2 cm) was placed around the lower esophagus using 2 interrupted, full-thickness, nonabsorbable sutures. We did not use an esophageal dilator when performing hiatal repair or placing the wrap. The shoe-shine maneuver and drop test were performed to evaluate the tension of the wrap. To prevent migration of the wrap, 2 to 3 additional sutures were placed to fix it to the esophageal wall and diaphragm.
Symptom control rates between groups were compared using Fisher exact and chi-square tests to evaluate the univariate effects of each predictor variable on successful surgical outcomes. To identify independently significant predictive factors, stepwise logistic regression was performed. The McNemar test was used to compare side effects immediately after surgery with those of 6 months after surgery. Significance was set at P < 0.05 for all comparisons.
A total of 61 patients underwent primary laparoscopic fundoplication for the treatment of GERD. The mean patient age was 46.7 years (range, 19–83 years). The mean age of the 26 female patients (42.6%) was 56.9 years, while the mean age of the 35 male patients (57.4%) was 46.9 years. The difference in age between these 2 groups was statistically significant (P = 0.029).
Preoperatively, all patients described symptoms of GERD. Typical symptoms (heartburn, regurgitation) were present in 60 patients (98.4%), while atypical symptoms were present in 40 patients (65.6%). Thirty-nine patients (63.9%) had both typical and atypical symptoms. The mean duration of GERD symptoms was 78.8 months (range, 6–480 months). All patients were taking acid-reducing medication preoperatively. Thirty-seven patients (60.7%) reported a history of poor response to acid-suppression treatment with PPIs. The mean duration of PPI medication was 22.0 months (range, 0–120 months). Radiologic reflux on barium esophagography was observed in 29 patients (53.7%) and pathologic acid reflux finding on ambulatory pH monitoring study was reported in 17 of the evaluated patients (39.5%) (Table 1).
Intraoperatively, pleural tears developed in 2 patients during the dissection of the hiatal hernia sac. Subsequent postoperative chest X-ray showed significant pneumomediastinum, which was managed conservatively; none of the cases required the placement of a surgical drain. There were no other postoperative complications including bleeding or visceral injury, nor open conversion. The average duration of surgery was 117.8 ± 37.2 minutes (range, 75–270 minutes), and the average postoperative hospital stay was 2.69 days.
Among the 60 patients who had typical GERD symptoms, typical GERD symptoms were completely controlled in 47 patients (78.3%) and partially improved in 4 patients (6.7%). Typical GERD symptoms were not controlled in 9 patients (15.0%) after surgery. For the 40 patients who had atypical GERD symptoms, atypical symptoms were completely controlled in 25 patients (62.5%) and partially controlled in 8 patients (20.0%). Seven patients (17.5%) with atypical symptoms did not improve after fundoplication. A total of 48 patients (78.7%) were completely cured and symptom-free including typical and atypical symptoms, and 54 patients (88.5%) experienced complete or partial resolution of GERD symptoms (Table 2).
The side effects of surgery were evaluated on the day of discharge and 6 months after surgery. Twenty-one patients (34.5%) developed postoperative dysphagia of mild or moderate grade. The rate of occurrence of this side effect significantly reduced with time, being present in only 6 patients (9.8%) at 6 months after surgery (P = 0.001). Most cases of dysphagia were mild grade (5 patients), although 1 patient had moderate grade dysphagia due to the intrathoracic migration of the wrap. Surgical or interventional treatments were not necessary for these patients.
Difficult belching was also significantly improved 6 months after surgery (P = 0.013). On the other hand, gas bloating was consistent during the follow-up period (P = 0.077) and flatulence was more frequent at 6 months after surgery compared with the immediate postoperative period (P < 0.001) (Table 3).
Complete GERD symptom control rates were compared according to age, sex, BMI, presence of atypical symptoms, hiatal hernia status, esophagitis on endoscopy, results of pH monitoring and upper gastrointestinal barium studies, duration of symptoms, response to PPI therapy, and surgeon experience.
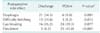
On univariate analysis, symptom control rates for patients who reported a good response to PPI therapy were significantly higher compared to patients who did not respond to PPI (P = 0.008). In addition, the rate of symptom control for patients with a hiatal hernia on preoperative endoscopy was better than that of patients without a hiatal hernia (P = 0.030). Age, sex, BMI, atypical symptoms, abnormal pH monitoring score, radiologic reflux on barium esophagography, esophagitis on endoscopy, long duration of symptoms, and surgeon experience did not significantly influence the surgical outcomes of GERD symptom control. Multivariate logistic regression analysis showed that preoperative PPI response was an independently significant predictor of outcome (P = 0.035) (Table 4).
GERD has recently been recognized as a common public health problem in Korea, where the use of acid-reducing medications is increasing [8]. Although the treatment of GERD is based on medical therapy, especially since the introduction of PPIs, the advent of minimally invasive surgery has led some physicians to consider laparoscopic antireflux surgery as a treatment option. Numerous randomized controlled trials have demonstrated similar or greater long-term improvement of GERD via antireflux surgery compared to treatment using drug-induced acid suppression with PPI [47]. Thus, antireflux surgery for GERD has become the standard in Western countries. Laparoscopic Nissen fundoplication is one of the most popular surgical procedures for the upper gastrointestinal tract in Western countries; however, many gastroenterologists and surgeons in Korea remain concerned about the uncertainties of this surgery, including its indications and efficacy. Thus, due to insufficient surgeon experience and the desire to avoid postoperative dysphagia, PPI therapy has remained the mainstay of GERD treatment. Indeed, there have been only 2-case series of antireflux surgery in Korea to date, which reported a complete or partial symptom control rate of 93% [910]. To the best of our knowledge, the present study is the largest reported series of antireflux surgery at a single institution in Korea to date.
The overall symptom improvement rate in our study was 88.5% and complete GERD symptom control was achieved in 78.7% of patients 6 months after surgery. This outcome was considered good based on the results of previous studies. Specifically, a majority of our patients had atypical symptoms, normal pH monitoring results, and were nonresponders to PPI therapy, and these have been reported as predictors of unsuccessful surgical outcomes.
Several studies have attempted to identify predictors of outcome after fundoplication [1112]. The majority of systematic reviews have confirmed that most demographic factors such as age, sex, and BMI do not predict outcome after fundoplication [12]. Patients with atypical symptoms of GERD, such as chest pain, asthma, hoarseness, chronic cough, and chronic bronchitis, are known to respond less well to fundoplication compared with patients with typical symptoms such as heartburn and regurgitation [1113]. However, in the present study, patients with atypical symptoms of GERD also showed good resolution of symptoms after fundoplication. Moreover, there was no difference in the rates of complete symptom control according to the presence of atypical symptoms. The results of this study also support the findings of Brown et al. [14], who described a good response to laparoscopic Nissen fundoplication in GERD patients with atypical symptoms after judicious evaluation and proper patient choice.
Symptomatic response to preoperative PPI treatment has been shown to be an excellent predictor of symptomatic response to fundoplication [15]. In the present study, PPI non-responders had a lower rate of symptom control compared with PPI responders. Indeed, response to PPI was the single most significant predictor of successful outcome according to multivariate regression analysis, which was consistent with the findings reported in previous studies [1115]. Although the clinical response to fundoplication for PPI nonresponders was significantly weaker than that for PPI responders, a substantial portion of PPI nonresponders had a good response to laparoscopic Nissen fundoplication. Therefore, PPI failure should not be considered a contraindication to antireflux surgery, but instead an indication for surgical treatment. On the other hand, a thorough evaluation is mandatory to confirm the diagnosis of GERD for these patients before making a decision regarding surgery because fundoplication is the last resort for PPI-refractory GERD patients. Likewise, the possibility of poor surgical outcomes must be discussed with patients before surgery.
In our patients, the presence of a hiatal hernia on preoperative endoscopy was related with the symptomatic success rate of surgery at the univariate level. Specifically, the symptomatic response for patients with hiatal hernias was excellent, with 95.0% of patients exhibiting complete symptom control. Anatomically, a hiatal hernia is a defect of the diaphragm which is one of the antireflux barriers of the lower esophagus. Thus, the surgical repair of this defect could have a clear effect by restoring normal antireflux mechanisms. Staehelin et al. [16] also reported that hiatal hernia is not associated with worse clinical outcome following laparoscopic fundoplication, with less heartburn and higher overall satisfaction. Although the effect of hiatal hernia on surgical outcome was not statistically significant at the multivariate level, GERD patients with hiatal hernia can be good candidates for antireflux surgery because better surgical outcomes could be expected for those patients. However, a previous study reported that larger hiatal hernias noted at the time of surgery are a predictor of subsequent failure because of increased risk of anatomical failure after surgery [17]. To determine the effect of preoperative hiatal hernia on the surgical outcome of antireflux surgery, the long-term follow-up of patients would be necessary.
Abnormal pH monitoring score was not related to success rate in this study, despite being the most objective measure of acid reflux and having been previously reported as a positive predictor of surgical outcome [17], Although, in this study, pH monitoring was not performed for some patients because of the confirmation of GERD using other examinations and the difficulty in stopping the PPI medication before the pH monitoring test, majority of patients had normal pH monitoring study results and showed equally good surgical outcomes compared with patients with abnormal pH monitoring results. Thus, a normal pH monitoring result should not be a contraindication for antireflux surgery but for symptomatic patients with normal pH monitoring results, who might have nonacid reflux, careful evaluation with other diagnostic modalities including barium esophagography or endoscopy is useful in selecting good surgical candidates.
In addition, barium esophagography is useful for defining the type and size of a hiatal hernia and gastroesophageal reflux. In our series, 53.7% of the patients examined had gastroesophageal reflux on barium esophagography. However, this positive finding was not related to success rate.
According to previous studies, operating time, hospitalization, early dysphagia, and complications are the most common parameters used to evaluate the learning curve of fundoplication and these significantly improve with surgeon experience. On the other hand, clinical outcomes of symptom resolution and patient satisfaction do not improve with experience [1819]. Consistently, we did not observe a difference in symptomatic outcomes according to surgeon experience. Operating time, hospitalization, and prevalence of postoperative dysphagia also did not differ according to surgeon experience, which was attributed to the surgeon's (JMP) previous experience with advanced laparoscopic gastric surgery and strict adherence to the principles of laparoscopic Nissen fundoplication, which were studied by the surgeon before beginning the procedure. Thus, the procedure was considered consistent for all of the patients in the study.
Dysphagia, difficulty belching, bloating, and flatulence are distinguishing postoperative adverse symptoms after fundoplication. According to previous reports from 628 Nissen fundoplication procedures, the prevalence of postoperative dysphagia was 34% at 0–3 months and 0.8% at 3–12 months after surgery. The vast majority of postoperative symptoms resolve within the first 4 weeks to 6 weeks after surgery [20]. We experienced a similar prevalence and resolution patterns of postoperative dysphagia. Furthermore, there were no cases of severe postoperative dysphagia requiring surgical or interventional therapy. Based on the results of the present study, dysphagia and difficulty belching developed immediately after surgery and resolved with time, whereas gas bloating and flatulence developed relatively later.
There were a few limitations in the present study. First, the follow-up period evaluated in this study was very short compared with other previous long-term studies. Second, follow-up examination for patients was based on symptomatic evaluation. We did not evaluate patients postoperatively using pH monitoring and manometry unless they reported recurrent symptoms. Thus, there was a lack of objective evidence of the improvement of reflux after fundoplication.
In conclusion, although laparoscopic Nissen fundoplication is not commonly performed in Korea, it is an efficacious method for controlling the symptoms of GERD based on our early experiences, which represent the most comprehensive report of laparoscopic antireflux surgery in Korea to date. Careful preoperative patient selection can identify patients at a high risk of surgical failure. PPI nonresponders have an increased risk of poor surgical outcome; thus, caution should be exercised in evaluation and treatment of such patients. Long-term evaluation of surgical results in a prospective study is needed to validate the outcomes of laparoscopic Nissen fundoplication.
Figures and Tables
References
1. Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006; 101:1900–1920.
2. Jung HK. Epidemiology of gastroesophageal reflux disease in Asia: a systematic review. J Neurogastroenterol Motil. 2011; 17:14–27.
3. Lundell L, Miettinen P, Myrvold HE, Hatlebakk JG, Wallin L, Malm A, et al. Seven-year follow-up of a randomized clinical trial comparing proton-pump inhibition with surgical therapy for reflux oesophagitis. Br J Surg. 2007; 94:198–203.
4. Mahon D, Rhodes M, Decadt B, Hindmarsh A, Lowndes R, Beckingham I, et al. Randomized clinical trial of laparoscopic Nissen fundoplication compared with proton-pump inhibitors for treatment of chronic gastro-oesophageal reflux. Br J Surg. 2005; 92:695–699.
5. Parrilla P, Martinez de Haro LF, Ortiz A, Munitiz V, Molina J, Bermejo J, et al. Long-term results of a randomized prospective study comparing medical and surgical treatment of Barrett's esophagus. Ann Surg. 2003; 237:291–298.
6. Spechler SJ, Lee E, Ahnen D, Goyal RK, Hirano I, Ramirez F, et al. Long-term outcome of medical and surgical therapies for gastroesophageal reflux disease: follow-up of a randomized controlled trial. JAMA. 2001; 285:2331–2338.
7. Galmiche JP, Hatlebakk J, Attwood S, Ell C, Fiocca R, Eklund S, et al. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. JAMA. 2011; 305:1969–1977.
8. Kim KM, Cho YK, Bae SJ, Kim DS, Shim KN, Kim JH, et al. Prevalence of gastroesophageal ref lux disease in Korea and associated health-care utilization: a national population-based study. J Gastroenterol Hepatol. 2012; 27:741–745.
9. Lee SB, Jeon KM, Kim BS, Kim KC, Jung HY, Choi YB. Early experiences of minimally invasive surgery to treat gastroesophageal reflux disease. J Korean Surg Soc. 2013; 84:330–337.
10. Lee SK, Kim EK. Laparoscopic Nissen fundoplication in Korean patients with gastroesophageal reflux disease. Yonsei Med J. 2009; 50:89–94.
11. Morgenthal CB, Lin E, Shane MD, Hunter JG, Smith CD. Who will fail laparoscopic Nissen fundoplication? Preoperative prediction of long-term outcomes. Surg Endosc. 2007; 21:1978–1984.
12. Ip S, Tatsioni A, Conant A, Karagozian R, Fu L, Chew P, et al. Predictors of clinical outcomes following fundoplication for gastroesophageal reflux disease remain insufficiently defined: a systematic review. Am J Gastroenterol. 2009; 104:752–758.
13. Ruigomez A, Rodriguez LA, Wallander MA, Johansson S, Thomas M, Price D. Gastroesophageal reflux disease and asthma: a longitudinal study in UK general practice. Chest. 2005; 128:85–93.
14. Brown SR, Gyawali CP, Melman L, Jenkins ED, Bader J, Frisella MM, et al. Clinical outcomes of atypical extra-esophageal reflux symptoms following laparoscopic antireflux surgery. Surg Endosc. 2011; 25:3852–3858.
15. Hamdy E, El Nakeeb A, Hamed H, El Hemaly M, ElHak NG. Outcome of laparoscopic Nissen fundoplication for gastroesophageal reflux disease in non-responders to proton pump inhibitors. J Gastrointest Surg. 2014; 18:1557–1562.
16. Staehelin A, Zingg U, Devitt PG, Esterman AJ, Smith L, Jamieson GG, et al. Preoperative factors predicting clinical outcome following laparoscopic fundoplication. World J Surg. 2014; 38:1431–1443.
17. Power C, Maguire D, McAnena O. Factors contributing to failure of laparoscopic Nissen fundoplication and the predictive value of preoperative assessment. Am J Surg. 2004; 187:457–463.
18. Broeders JA, Draaisma WA, Rijnhart-de Jong HG, Smout AJ, van Lanschot JJ, Broeders IA, et al. Impact of surgeon experience on 5-year outcome of laparoscopic Nissen fundoplication. Arch Surg. 2011; 146:340–346.
19. Tsuboi K, Gazallo J, Yano F, Filipi CJ, Mittal SK. Good training allows excellent results for laparoscopic Nissen fundoplication even early in the surgeon's experience. Surg Endosc. 2010; 24:2723–2729.
20. Frantzides CT, Carlson MA, Zografakis JG, Moore RE, Zeni T, Madan AK. Postoperative gastrointestinal complaints after laparoscopic Nissen fundoplication. JSLS. 2006; 10:39–42.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download