Abstract
Purpose
The aim of this study was to confirm the factors that affect the mortality associated with the open surgical repair of ruptured abdominal aortic aneurysm (rAAA) and to analyze the long-term survival rates.
Methods
A retrospective review was performed on a prospectively collected database that included 455 consecutive patients who underwent open surgical repair for AAA between January 2001 and December 2012. We divided our analysis into in-hospital and postdischarge periods and analyzed the risk factors that affected the long-term survival of rAAA patients.
Results
Of the 455 patients who were initially screened, 103 were rAAA patients, and 352 were non-rAAA (nAAA) patients. In the rAAA group, 25 patients (24.2%) died in the hospital and 78 were discharged. Long-term survival was significantly better in the nAAA group (P = 0.001). The 2-, 5-, and 10-year survival rates of the rAAA patients were 87%, 73.4%, and 54.1%, respectively. Age (hazard ratio [HR], 1.05; 95% confidence interval [CI], 1.02–.08; P < 0.001) and aneurysm rupture (HR, 1.96; 95% CI, 1.12–.44; P = 0.01) significantly affected long-term survival.
The mortality rate associated with the elective treatment of non-ruptured abdominal aortic aneurysm (nAAA) has decreased in recent years. Nonetheless, 85% of patients with ruptured AAA (rAAA) die and 66% of these deaths occur before reaching the hospital or without undergoing an operation [1]. The mortality rate of the patients who undergo repair procedures is still 37%–74% [2]. There have been various studies of the perioperative mortality rate and its different risk factors in rAAA patients. Scarcello et al. [3] reported that the time before shock is the most important predictor of rAAA mortality, whereas Davies et al. [4] reported that postoperative renal replacement therapy is a risk factor for rAAA mortality. Antonopoulos et al. [5] reported that age, coronary artery disease, chronic renal failure, hemodynamic instability, and open surgical repair are risk factors that affect death from rAAA. There have also been reports of long-term survival outcomes after the surgical repair of a rAAA [67]. However, these studies were all conducted prior to 2000. To our knowledge, there has been no comparable study since then and surgical techniques, graft material, postoperative critical care, and anesthetic techniques have improved considerably in that time.
We therefore designed our present study to identify the factors that affect the mortality of patients who have undergone an open surgical rAAA repair since 2001 and analyzed the long-term survival rates in this population.
A retrospective medical data review was performed on a prospectively collected database of patients who underwent treatment for open repaired AAA at Asan Medical Center between January 2001 and December 2012. This study was performed with approval from Institutional Review Board of Asan Medical Center (approval number, 2015-0697) for the collection of patient medical data. A total of 455 consecutive patients were identified. rAAA was diagnosed in these cases on the basis of symptoms (e.g., acute abdominal or back pain) and CT findings. Rupture was defined as evidence of extravasated hematoma or blood. These findings were confirmed by a CT scan or operative findings. We investigated survival status and follow-up status in March 2015. Postoperative patient follow-up examinations included a physical examination, medical history review, and CT angiography at 6 months and 12 months; thereafter, annual follow-up examinations were conducted.
When the rAAA patients arrived at the hospital and resuscitation was required, they were initially resuscitated according to the patient's medical condition using fluids, packed RBCs, fresh frozen plasma, and platelet concentrates. Resuscitation was continued until the point of permissive hypotension. Permissive hypotension meant that when we resuscitated the rAAA patients, their systolic blood pressure was limited to a maximum of 100 mmHg in order to prevent excessive bleeding from the aneurysmal sac [8]. All patients were managed by 3 expert vascular surgeons with substantial experience in AAA management.
To better analyze long-term survival and the factors that affect rAAA patient mortality, in-hospital mortality patients were excluded from our analysis. This is because an aortic rupture is a severe event that causes a high perioperative mortality rate. We thus conducted a comparison of rAAA patients with nAAA patients who survived.
The risk factors that were identified in previous studies [91011] were considered as variables that could possibly affect the mortality of rAAA patients. Circulatory failure was defined as systolic blood pressure < 80 mmHg for >10 minutes upon hospitalization before a procedure, regardless of whether a vasopressor or volume replacement was used [2]. Abdominal compartment syndrome was diagnosed when the bladder pressure was >25 mmHg with abdominal distension and cardiovascular collapse [12]. Coronary artery disease was defined as a history of myocardial infarction or angina, percutaneous coronary intervention, coronary artery bypass grafting, and/or ischemic ST segment abnormalities on preoperative electrocardiography [13]. Patient with a serum creatinine level > 1.7 mg/dL were considered to have decreased renal function [14].
Continuous variables were expressed as the mean ± standard error. The chi-square test, Student t-test, and analysis of variance were used to compare the rAAA and nAAA groups. The effects of multiple factors were assessed using binary logistic regression. The Kaplan-Meier method was used to evaluate the postdischarge survival rate. We used Cox regression analysis to analyze the risk factors that affected the postdischarge survival rate. We considered P < 0.05 to indicate statistical significance. Statistical analyses were performed using IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA).
Of the 455 patients who underwent open surgical repair for AAA at Asan Medical Center during the study period, 103 were rAAA patients and 352 were nAAA patients. Of the 103 patients in the rAAA group, 25 patients (24.2%) died in the hospital and 78 (75.7%) were discharged. Of the 352 patients in the nAAA group, 7 patients (1.9%) died in the hospital and 345 (98%) were discharged. The age, rate of patients with decreased renal function, and rate of saccular AAA were higher in the rAAA group than in then AAA group. However, the rate of coronary artery disease patient was lower in the rAAA group than in then AAA group, despite high mortality. The demographic and clinical characteristics of all included patients are presented in Table 1. The most common cause of death for the 25 patients in the rAAA group who died during the hospital stay was hypovolemic shock (Table 2).
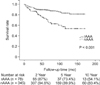
We evaluated the long-term survival rates of the rAAA and nAAA patients after excluding cases of in-hospital mortality. The mean follow-up period was 69.27 ± 46.90 months in the rAAA group and 73.61 ± 43.54 months in the nAAA group, and there was no statistical difference in follow-up period between the 2 groups (P = 0.33). The cumulative survival rate analysis showed that overall survival was significantly better in the nAAA group than in the rAAA group (P < 0.001). The 2-, 5-, and 10-year survival rates were 87%, 73.4%, and 54.1%, respectively, in the rAAA group and 94.6%, 89.9%, and 83.4%, respectively, in the nAAA group (Fig. 1).
Univariate Cox proportional-hazard analysis was used to analyze the factors that affected mortality, and factors with P < 0.1 were considered together in the multivariate analysis. Age (hazard ratio [HR], 1.05; 95% confidence interval [CI], 1.02–.08; P < 0.001) and aneurysm rupture (HR, 1.96; 95% CI, 1.12–.44; P = 0.01) were significant predictors of mortality in this analysis (Table 3).
Since 2000, there have been improvements in perioperative management and surgical devices. We can use aortic occlusion balloon in the distal thoracic aorta through the femoral artery to prevent excessive bleeding during anesthesia and resuscitation. Despite these recent advances however, mortality remains high in rAAA patients, as with our current cohort.
The in-hospital mortality rate was 24.2% in our study. The analysis of the causes of in-hospital deaths revealed that on-table deaths or immediate postoperative mortality due to hypovolemic shock caused by bleeding represented up to 32% of the in-hospital deaths. We hypothesized that avoiding preoperative circulatory failure may be important in reducing the in-hospital mortality rate. Some of our in-hospital mortality patients underwent preoperative circulatory failure as a result of permissive hypotension strategy. In real clinical situations, it is not easy to maintain the critical blood pressure range between that for hypotensive hemostasis and that for ‘avoiding preoperative circulatory failure.’ Our current study findings are also likely to have been strongly influenced by this process. The permissive hypotension strategy for rAAA patients has already been accepted by many centers. Even Crawford [15] have suggested that blood volume resuscitation should not be attempted until the time of surgery, and that the systolic blood pressure should be maintained at 50–70 mmHg using a small volume of whole blood or crystalloids until aortic clamping can be applied to prevent excessive blood loss. However, to our knowledge, there was no randomized controlled trial studies for hypotensive versus normotensive resuscitation strategies in patients with ruptured abdominal aortic aneurysms [16]. Our results cannot argue convincingly that there is no need to apply hypotensive resuscitation strategy. But, we have to avoid preoperative circulatory failure to reduce the in-hospital mortality.
In this study, the 2-, 5-, and 10-year survival rates of open-repaired rAAA patients were 87%, 73.4%, and 54.1%, respectively. And we confirmed a number of factors that affect the long-term survival rate in rAAA patients, namely age and AAA rupture. However, the presence of AAA rupture was used to divide our sample population into rAAA and nAAA groups. Therefore, age was the only factor affecting the mortality of AAA patients after excluding perioperative mortality cases. These data indicate that open surgical repair is not yet an outdated procedure for rAAA and studies of this treatment thus need to be continued. In the endovascular era, endovascular aneurysm repair (EVAR) has become the standard procedure for elective AAA repair. There have been many randomized trials, and cohort series have clearly demonstrated advantages including early survival. However, in the case of rAAA, EVAR cannot completely replace open surgical repair. Three randomized control trials comparing the EVAR and open surgical repair for rAAA have been conducted, and no superiority of either procedure was found in terms of survival [171819]. Some limitations have also been described for the emergent EVAR procedure. The anatomy of the aorta has to be examined for EVAR which necessitates the use of CT prior to surgery, regardless of the instability of the patient's hemodynamic status. Mehta et al. [20] reported better 5-year survival rates with EVAR than with open surgical repair. But, in this study, we speculated that the patient selection bias may have had an impact in this regard. Open repair is typically conducted on patients who are hemodynamically unstable or who have a more complex aortic anatomy that is not suitable for EVAR, such as a juxta renal type or supra renal type.
There are several limitations of this study. One notable limitation lies in the confirmation of the risk factors that affect the long-term survival rate in rAAA patients. We did not include any variables related to the characteristics of the aorta when comparing the long-term survival rates. Some studies have reported that organ failure is related to the mortality rate after AAA repair [2122], and postoperative renal impairment increases with increasing aortic clamp level [23]. Thus, the type, cause, and morphology of the AAA also should be analyzed as risk factors in future studies. The second limitation of this study is that the cause of deaths was not inspected during the long term survival rate analysis. For this reason, we could not explore the long-term complications. Third, this study was retrospective. The patient data were collected prospectively, but the analysis was conducted retrospectively. Therefore, there is a shortage of evidence for the results.
In conclusion, the prevention of preoperative circulatory failure is needed to reduce in-hospital mortality in rAAA patients. The long-term survival rate of rAAA patients is poorer than that of nAAA patients. Age is the only confirmed factor that affects this outcome.
Figures and Tables
Fig. 1
Comparison of the long-term survival rates of rAAA and nAAA patients analyzed in this study (not including the in-hospital mortality cases) using the Kaplan-Meier method. AAA, abdominal aortic aneurysm; rAAA, ruptured AAA; nAAA, non-rAAA.
References
1. Mastracci TM, Garrido-Olivares L, Cina CS, Clase CM. Endovascular repair of ruptured abdominal aortic aneurysms: a systematic review and meta-analysis. J Vasc Surg. 2008; 47:214–221.
2. Bonardelli S, Cervi E, Maffeis R, Nodari F, De Lucia M, Guadrini C, et al. Open surgery in endovascular aneurysm repair era: simplified classification in two risk groups owing to factors affecting mortality in 137 ruptured abdominal aortic aneurysms (RAAAs). Updates Surg. 2011; 63:39–44.
3. Scarcello E, Ferrari M, Rossi G, Berchiolli R, Adami D, Romagnani F, et al. A new preoperative predictor of outcome in ruptured abdominal aortic aneurysms: the time before shock (TBS). Ann Vasc Surg. 2010; 24:315–320.
4. Davies RS, Dawlatly S, Clarkson JR, Bradbury AW, Adam DJ. Outcome in patients requiring renal replacement therapy after open surgical repair for ruptured abdominal aortic aneurysm. Vasc Endovascular Surg. 2010; 44:170–173.
5. Antonopoulos CN, Kakisis JD, Andrikopoulos V, Dervisis K, Georgopoulos S, Giannoukas A, et al. Predictors affecting in-hospital mortality of ruptured abdominal aortic aneurysms: a Greek multicenter study. Ann Vasc Surg. 2014; 28:1384–1390.
6. Soisalon-Soininen S, Salo JA, Takkunen O, Mattila S. Comparison of long-term survival after repair of ruptured and non-ruptured abdominal aortic aneurysm. Vasa. 1995; 24:42–48.
7. Cho JS, Gloviczki P, Martelli E, Harmsen WS, Landis ME, Cherry KJ Jr, et al. Long-term survival and late complications after repair of ruptured abdominal aortic aneurysms. J Vasc Surg. 1998; 27:813–819.
8. Tsilimparis N, Saleptsis V, Rohlffs F, Wipper S, Debus ES, Kolbel T. New developments in the treatment of ruptured AAA. J Cardiovasc Surg (Torino). 2016; 57:233–241.
9. Laukontaus SJ, Aho PS, Pettilä V, Albäck A, Kantonen I, Railo M, et al. Decrease of mortality of ruptured abdominal aortic aneurysm after centralization and in-hospital quality improvement of vascular service. Ann Vasc Surg. 2007; 21:580–585.
10. Acosta S, Ogren M, Bengtsson H, Bergqvist D, Lindblad B, Zdanowski Z. Increasing incidence of ruptured abdominal aortic aneurysm: a population-based study. J Vasc Surg. 2006; 44:237–243.
11. Cho JS, Kim JY, Rhee RY, Gupta N, Marone LK, Dillavou ED, et al. Contemporary results of open repair of ruptured abdominal aortoiliac aneurysms: effect of surgeon volume on mortality. J Vasc Surg. 2008; 48:10–17.
12. Rubenstein C, Bietz G, Davenport DL, Winkler M, Endean ED. Abdominal compartment syndrome associated with endovascular and open repair of ruptured abdominal aortic aneurysms. J Vasc Surg. 2015; 61:648–654.
13. Han SR, Kim YW, Heo SH, Woo SY, Park YJ, Kim DI, et al. Frequency of concomitant ischemic heart disease and risk factor analysis for an early postoperative myocardial infarction after elective abdominal aortic aneurysm repair. Ann Surg Treat Res. 2016; 90:171–178.
14. Kwon H, Lee DY, Choi SJ, Park KH, Min SK, Chang JH, et al. Anatomical features and early outcomes of endovascular repair of abdominal aortic aneurysm. Vasc Specialist Int. 2015; 31:87–94.
15. Crawford ES. Ruptured abdominal aortic aneurysm. J Vasc Surg. 1991; 13:348–350.
16. Moreno DH, Cacione DG, Baptista-Silva JC. Controlled hypotension versus normotensive resuscitation strategy for people with ruptured abdominal aortic aneurysm. Cochrane Database Syst Rev. 2016; (5):CD011664.
17. Hinchliffe RJ, Bruijstens L, MacSweeney ST, Braithwaite BD. A randomised trial of endovascular and open surgery for ruptured abdominal aortic aneurysm - results of a pilot study and lessons learned for future studies. Eur J Vasc Endovasc Surg. 2006; 32:506–513.
18. Hoornweg LL, Wisselink W, Vahl A, Balm R. Amsterdam Acute Aneurysm Trial Collaborators. The Amsterdam Acute Aneurysm Trial: suitability and application rate for endovascular repair of ruptured abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2007; 33:679–683.
19. IMPROVE Trial Investigators. Endovascular strategy or open repair for ruptured abdominal aortic aneurysm: one-year outcomes from the IMPROVE randomized trial. Eur Heart J. 2015; 36:2061–2069.
20. Mehta M, Byrne J, Darling RC 3rd, Paty PS, Roddy SP, Kreienberg PB, et al. Endovascular repair of ruptured infrarenal abdominal aortic aneurysm is associated with lower 30-day mortality and better 5-year survival rates than open surgical repair. J Vasc Surg. 2013; 57:368–375.
21. Bown MJ, Nicholson ML, Bell PR, Sayers RD. The systemic inflammatory response syndrome, organ failure, and mortality after abdominal aortic aneurysm repair. J Vasc Surg. 2003; 37:600–606.
22. Maziak DE, Lindsay TF, Marshall JC, Walker PM. The impact of multiple organ dysfunction on mortality following ruptured abdominal aortic aneurysm repair. Ann Vasc Surg. 1998; 12:93–100.
23. Ambler GK, Coughlin PA, Hayes PD, Varty K, Gohel MS, Boyle JR. Incidence and outcomes of severe renal impairment following ruptured abdominal aortic aneurysm repair. Eur J Vasc Endovasc Surg. 2015; 50:443–449.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download