Abstract
Purpose
We aimed to develop an effective system for surgical site infection (SSI) surveillance and examine the current domestic state of SSIs for common abdominal surgeries in Korea.
Methods
The Korean Surgical Site Infection Surveillance (KOSSIS) program was developed as an SSI surveillance system. A prospective multicenter study in nine university-affiliated or general hospitals was conducted for patients who underwent gastrectomy, cholecystectomy, appendectomy, colectomy, or proctectomy between August 16 and September 30 in 2012. Patients were monitored for up to 30 days by combining direct observation and a postdischarge surgeon survey. Data on SSIs were prospectively collected with KOSSIS secretarial support according to a common protocol. Operation-specific SSI rates were stratified according to risk factors and compared with data from the Korean Nosocomial Infections Surveillance System (KONIS) and National Healthcare Safety Network. A focus group interview was conducted with participating hospitals for feedback.
Results
A total of 1,088 operations were monitored: 207 gastrectomies, 318 cholecystectomies, 270 appendectomies, 197 colectomies, and 96 proctectomies. Operation-specific SSI rates determined by the KOSSIS program were substantially higher than those found in KONIS (7.73% [95% confidence interval, 4.5%-12.3%] vs. 3.4% for gastrectomies, 10.15% [95% confidence interval, 6.1%-15.2%] vs. 4.0% for colectomy, and 13.5% [95% confidence interval, 7.4%-22.0%] vs. 4.2% for proctectomy).
Surgical site infections (SSIs) are the leading cause of nosocomial infection. The incidence of SSI ranged from 2.0% to 9.7% in Korea [1]. SSIs remain a major clinical problem leading to prolonged hospital stays, extra costs, and increased morbidity and mortality [2,3]. The Korean Nosocomial Infections Surveillance System (KONIS) was established in 2006 [4,5,6]. This surveillance system attracts voluntary participation from hospitals and uses the KONIS Web-based Report and Analysis Program to efficiently collect and share SSI data with participating hospitals in real-time. However, any surveillance system that uses computerized medical records could underestimate SSIs because superficial SSIs might not be reported [7]. National surveillance systems for nosocomial infection have already been developed and implemented successfully in the United States (US) and European countries [8,9]. Even though similar infection surveillance protocols are used, differences occur in the implementation, and comparisons between countries can be difficult [9]. Even data derived from national programs might not be comparable with data from high-quality surveillance trials of SSI interventions [10,11]. Concerns about the accuracy and validity of national surveillance data are therefore justified. Recently, KONIS demonstrated that the laborious and time-consuming task of dealing with the massive amount of data produced was a main obstacle to expanding the number of participating hospitals and target operation procedures (unpublished, 2013 internal report from KONIS). Thus, KONIS is moving to reduce investigation categories and shorten the duration of participation.
We developed the Korean Surgical Site Infection Surveillance (KOSSIS) program to focus on SSI among nosocomial infections by combining direct observation and a postdischarge surgeon survey. We conducted a prospective multicenter study using the KOSSIS program to establish an effective SSI surveillance system and evaluate SSI rates and risk factors in the Korean surgical setting.
Both regional distribution and the volume of hospitals in this study were balanced to include small and medium-sized hospitals, surgical specialty hospitals, colorectal specialty hospitals, and tertiary hospitals. Eventually, the KOSSIS secretariat selected nine hospitals where collaborative research was possible with corresponding surgeons performing operations under surveillance. In the nine participating hospitals, the prospective SSI survey was conducted during the short period from August 16 to September 30, 2012, for five common gastrointestinal surgeries: gastrectomy, cholecystectomy, appendectomy, colectomy, and proctectomy. Data on SSIs were prospectively collected with secretarial support according to a common protocol developed by KOSSIS. Surgeons, infection specialists with surveillance experience, and physicians in charge of infection control were trained by KOSSIS and then instructed to complete the SSI surveillance form. Patients aged 20 years or younger were excluded from the surveillance, except for appendectomies because of the operation's frequency among young people.
The definition from the US Centers for Disease Control was used to diagnose SSI [12]. The investigation methods were as follows: (1) The surgeon or surgical team was directed to examine the surgical site more than 3 times per week during the hospital stay for patients who underwent operations subject to surveillance. (2) The presence of SSI was determined through direct observation of the surgical site by the surgeon or surgical team, or adjunctively with indirect methods through a review of a patient's medical record, microorganism test, or radiological data. (3) The surgeon-report survey form was completed at the first outpatient follow-up appointment. (4) The surveillance period was set as 30 postoperative days. The presence of SSI was prospectively monitored until SSI developed or 30 days had passed after surgery. If surveillance for 30 days after surgery proved difficult or impossible, the surgeons recorded when and why the case was closed early. Patients were told to visit the outpatient department or emergency room if they experienced any kind of wound problems or fever.
Demographic data on the patients, hospital characteristics, and possible perioperative variables associated with the development of SSI were collected. Perioperative variables were as follows: gender, age, obesity (body mass index [BMI] ≥ 25 kg/m2), presence of diabetes mellitus, a history of smoking 1 month or less before the surgery, serum albumin level, a history of radiation therapy, use of any form of systemic steroid for 1 week or more before surgery, immune suppressive agent, laparoscopic versus open surgery, emergency status, trauma, simultaneous surgery at a different anatomical site through the same incision, whether reoperation was performed at the same site within the surveillance period, a history of previous operations, packed RBC (PRBC) transfusion within 24 hours before or after surgery, type of anesthesia, presence or absence of infection at other sites, wound contamination class [13], American Society of Anesthesiologists (ASA) physical status score [14], duration of surgery, and T-time. According to hospital size, hospitals with either more than 500 beds or fewer than 500 beds were compared.
The National Nosocomial Infection Surveillance (NNIS) System risk index was used to compare SSI rates [15]. When multiple operations were performed at a single incision site, the relationship of any infection with the corresponding operation was clarified in the record. When the relationship of a superficial SSI and a corresponding operation was not identifiable, the operation (among those listed above) with the higher SSI rate was recorded. The operation performed closest to the day of SSI onset was recorded as the onset cause of SSI unless there was evidence that the infection was associated with a different operation.
At the end of the survey, a focus group interview (FGI) was conducted at participating hospitals to establish an SSI surveillance system and suggest measures for improvement and postoperative infection prevention.
T-test and chi-square or Fisher exact test were performed to identify general characteristics by operation type. Univariate logistic regression analysis was performed to find risk factors for infection. Multivariate logistic regression analysis was carried out for variables with P-values of less than 0.2 in the univariate analysis. Statistical analysis was performed using SAS 9.2 (SAS Institute Inc., Cary, NC, USA), and P-values less than 0.05 were considered statistically significant.
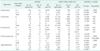
The general characteristics of the participating hospitals are shown in Table 1. They varied in terms of hospital size, facilities, and personnel resources. The total of analyzed operations was 1,088: 207 gastrectomies, 318 cholecystectomies, 197 colectomies, 96 rectal resections, and 270 appendectomies (Table 2). According to wound classification by operation, clean-contaminated wounds were the most common type. Table 3 shows the incidence of infection and infection rate by operation.
Univariate analysis was performed to identify factors affecting SSI in gastrectomy. Significant risk factors were age (odds ratio [OR], 1.05; 95% confidence interval [CI], 1.002-1.10, P = 0.04), laparoscopic operation (OR, 0.11; 95% CI, 0.02-0.48, P = 0.003), and transfusion (OR, 4.97; 95% CI, 1.71-14.4, P = 0.003). In the multivariate analysis, laparoscopic operation (OR, 0.06; 95% CI, 0.01-0.51; P = 0.01) and BMI index (OR, 5.26; 95% CI, 1.26-21.99, P = 0.02) were found to be significant factors. However, statistical estimation was unachievable for 9 among the 22 risk factors, probably because they did not occur or had minimal influence on infections.
According to the univariate analysis of colectomy, the significant risk factors affecting SSI were laparoscopic operation (OR, 0.23; 95% CI, 0.09-0.6; P = 0.003), T-time (OR, 4.33; 95% CI, 1.67-11.18; P = 0.003), stoma (OR, 6.07; 95% CI, 1.6-22.98; P = 0.008), and hospital size (OR, 0.19; 95% CI, 0.06-0.56; P = 0.003). When multivariate analysis was performed, laparoscopic operation (OR, 0.2; 95% CI, 0.06-0.73; P = 0.01) and a hospital with more than 500 beds (OR, 0.09; 95% CI, 0.02-0.39; P = 0.001) were found to be significant.
For rectal surgery, no significant factors for SSI were detected in the univariate or multivariate analyses.
For cholecystectomy, ASA class was found to be significant in the univariate analysis (OR, 6.53; 95% CI, 1.05-40.68; P = 0.04), but no significant factor was detected in the multivariate analysis.
For appendectomy, many variables were excluded from analysis due to insufficient infection frequency. However, according to univariate analysis, wound class was the only significant variable. When compared with clean-contaminated wounds, the infection rate was significantly higher in dirty wounds, with an odds ratio of 7.63 (P = 0.01). No significant factor was found in the multivariate analysis.
When compared with the mean infection rate found by National Healthcare Safety Network (NHSN) [16], the SSI rate reported using KOSSIS was significantly higher in gastrectomy, colectomy, proctectomy, and appendectomy (Table 4). When compared with the SSI rates reported using KONIS, the KOSSIS infection rate was significantly higher in gastrectomy, colectomy, and proctectomy (Table 5). SSI following cholecystectomy was high only in NNIS risk index category 0. The infection rate was in the 90th percentile range in gastrectomy, proctectomy, and cholecystectomy in the comparison with the KONIS data. Appendectomy was excluded from the comparison because it is not subject to surveillance in KONIS.
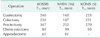
According to hospital size, hospitals with either more than 500 beds or fewer than 500 beds were compared. Only in colectomy, the infection rate (7.87%) in hospitals with more than 500 beds was significantly lower than that (31.58%) in hospitals with fewer than 500 beds (P = 0.01). The operation times found using KOSSIS were similar to those reported in KONIS, except for rectal surgery (Table 6).
The surveillance period and reasons for early closure of surveillance were surveyed. Only 193 patients (17.7%) met the requirements of the surveillance period for 30 days after surgery. When surveillance was not sustained until 30 days after surgery, the main reason (93.3%) was nonattendance after the first outpatient appointment (nonattendance at the outpatient department after surgery 6%, reoperation 0.8%, death 0.2%, and interhospital transfer 0.1% were the other reasons). Mean time to SSI diagnosis after surgery ranged between 6 and 10 days (Table 7).
This study reports significantly higher infection rates than were found with KONIS or NHSN. However, comparing these in a meaningful way may be problematic because this study was conducted among a small number of patients during a short-term period, and participating hospitals had different characteristics. However, concerns could be raised although KONIS has distinguished itself as a leader in surveillance for nosocomial infection in Korea. Recently, KONIS has begun moving to reduce investigation categories and shorten the duration of participation to reduce the burdens of surveillance (unpublished, 2013 internal report from KONIS). KONIS reported that because it was difficult to implement routine direct wound examination by trained professionals, chart review was the method of SSI surveillance applied in most participating hospitals (unpublished, 2012 internal report from KONIS). In this study, surgeons directly determined whether SSI was present and processed the surveillance. Moreover, the KONIS criteria for participating hospitals are more than 300 hospital beds with doctors and nurses specialized in infection control, but most hospitals actually joining KONIS are large. Only hospitals employing infection control personnel may participate in KONIS. Among the 60 hospitals that volunteered to participate in KONIS in 2012, only 11% were hospitals with fewer than 500 beds, whereas they represented 55.6% of the hospitals in the present study. The higher infection rate found by KOSSIS could also be attributable to under-reporting in KONIS's data.
At the end of the survey period, an FGI was conducted with participating hospitals to review the SSI surveillance system and plan improvement measures. According to the FGI, one reason SSI surveillance was carried out efficiently during the study period was that additional staff were allocated for the surveillance task. Also, participants answered that the development of standardized indices enabled the progress of this study. Participating hospitals have already requested government support to reduce SSIs. The FGI showed different requirements for SSI prevention between participating hospitals. Large hospitals need continued participation in surveillance programs, whereas small hospitals (fewer than 500 beds) need economic support for education and environmental improvement for SSI control. In the present study, hospitals with fewer than 500 beds showed much higher infection rate in colectomy (31.58% vs. 7.87%), which is a striking example that reflects the current situation and an issue to solve through sustained effort.
To continue operation of an SSI surveillance system, a specialized surveillance unit needs to be organized with the support of a national subsidy. Furthermore, a national surveillance system, computer system, and services need to be established, and the government must bear the burden of the expense. Hospitals in financial distress need physical resources. Although environment-management in operating rooms is recommended as an infection prevention activity, the current status of management conditions is inadequate in small and medium-sized hospitals, unlike in large hospitals. Therefore, the government needs to be more proactive in providing the money necessary for SSI prevention and facility maintenance.
This study had some limitations because it was preliminary research, and monitoring was carried out for only 45 days. In the analysis of the risk factors for SSI among such a small number of patients, statistical estimation was almost impossible in many cases due to nonoccurrence. Participating hospitals showed various levels of operating-room facilities as well as differences in experience and preventive activities for SSI control. Although small numbers of patients in hospitals of various sizes were involved, the 75th-percentile cutoff points for the operation times were similar to those found by KONIS, except for rectal surgery. Gastrectomy, colectomy, and rectal resection were most often performed in hospitals with 500 or more beds, whereas cholecystectomy and appendectomy were done even in hospitals with fewer than 500 beds. Despite using both inpatient and postdischarge SSI surveillance in this study, only a small percentage of patients (17.7%) met the requirements of the surveillance period for 30 days after surgery. However, the mean total diagnostic period of SSI ranged between 6 and 10 days, and the presence of infection was detected at the first outpatient visit in most patients. For actual SSI rates, a patient survey by telephone or mail should be implemented on the last day of surveillance when a patient does not visit the outpatient department as scheduled.
In conclusion, despite a short surveillance period, heterogenous group of hospitals, and small numbers of patients, our results suggest that KOSSIS could be a useful program for enhancing SSI surveillance in Korea. The domestic SSI rate is anticipated to decrease following the establishment of an SSI surveillance system nationwide based on this study. It is necessary to implement education and financial support for SSI prevention at the government level.
Figures and Tables
Acknowledgments
This work was supported by the Health Insurance Review & Assessment Service research project in Korea.
References
1. Lee KY, Coleman K, Paech D, Norris S, Tan JT. The epidemiology and cost of surgical site infections in Korea: a systematic review. J Korean Surg Soc. 2011; 81:295–307.
2. Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999; 20:725–730.
3. Leaper DJ, van Goor H, Reilly J, Petrosillo N, Geiss HK, Torres AJ, et al. Surgical site infection: a European perspective of incidence and economic burden. Int Wound J. 2004; 1:247–273.
4. Kim YK, Kim HY, Kim ES, Kim HB, Uh Y, Jung SY, et al. The Korean Surgical Site Infection Surveillance System Report, 2009. Korean J Nosocomial Infect Control. 2010; 15:1–13.
5. Kim YK, Kim HY, Kim ES, Kim HB, Jin HY, Lee JY, et al. Korean Surgical Site Infection Surveillance System Report: data summary from July 2010 through June 2011. Korean J Nosocomial Infect Control. 2012; 17:1–12.
6. Kwak YG, Lee SO, Kim HY, Kim YK, Park ES, Jin HY, et al. Risk factors for deviceassociated infection related to organisational characteristics of intensive care units: findings from the Korean Nosocomial Infections Surveillance System. J Hosp Infect. 2010; 75:195–199.
7. Kim ES, Kim HB, Song KH, Kim YK, Kim HH, Jin HY, et al. Prospective nationwide surveillance of surgical site infections after gastric surgery and risk factor analysis in the Korean Nosocomial Infections Surveillance System (KONIS). Infect Control Hosp Epidemiol. 2012; 33:572–580.
8. Centers for Disease Control and Prevention (CDC). Monitoring hospital-acquired infections to promote patient safety: United States, 1990-1999. MMWR Morb Mortal Wkly Rep. 2000; 49:149–153.
9. Coello R, Gastmeier P, de Boer AS. Surveillance of hospital-acquired infection in England, Germany, and The Netherlands: will international comparison of rates be possible? Infect Control Hosp Epidemiol. 2001; 22:393–397.
10. Wick EC, Gibbs L, Indorf LA, Varma MG, Garcia-Aguilar J. Implementation of quality measures to reduce surgical site infection in colorectal patients. Dis Colon Rectum. 2008; 51:1004–1009.
11. Tanner J, Padley W, Kiernan M, Leaper D, Norrie P, Baggott R. A benchmark too far: findings from a national survey of surgical site infection surveillance. J Hosp Infect. 2013; 83:87–91.
12. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008; 36:309–332.
13. Garner JS. CDC guideline for prevention of surgical wound infections, 1985. Supersedes guideline for prevention of surgical wound infections published in 1982. (Originally published in November 1985). Revised. Infect Control. 1986; 7:193–200.
14. Owens WD, Felts JA, Spitznagel EL Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978; 49:239–243.
15. The Society for Hospital Epidemiology of America. The Association for Practitioners in Infection Control. The Centers for Disease Control. The Surgical Infection Society. Consensus paper on the surveillance of surgical wound infections. Infect Control Hosp Epidemiol. 1992; 13:599–605.
16. Edwards JR, Peterson KD, Mu Y, Banerjee S, Allen-Bridson K, Morrell G, et al. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009; 37:783–805.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download