Abstract
Purpose
It is unknown whether patients with advanced rectal cancer develop severe constipation. Therefore, the objective of this study was to assess whether constipation severity is associated with pathologic progression of rectal cancer.
Methods
We analyzed 472 patients with rectal cancer who underwent elective surgical resection between January 2005 and December 2010. Constipation severity was prospectively evaluated in 407 patients (86.2%) using the Cleveland Clinic Constipation Score System. Linear regression analysis was performed to identify clinicopathologic variables associated with constipation. Kaplan-Meier analysis and Cox proportional hazard models were used to evaluate the prognostic value of constipation severity on disease-free and overall survival.
Results
Multivariable analysis showed that sex (regression coefficient [B] = 1.55; 95% confidence interval [CI], 0.79 to 2.60; P < 0.001), body mass index (B = -0.95; 95% CI, -1.83 to -0.64; P = 0.036), tumor size (B = 1.04; 95% CI, 0.20 to 1.88; P = 0.016), T stage (B = 0.75; 95% CI, 0.23 to 1.27; P = 0.005), and distant metastasis (B = 1.16; 95% CI, 0.03 to 2.30; P = 0.045) were associated with constipation severity. Severe constipation (score ≥ 8) was independently associated with 3-year disease-free survival (vs. scores of 0-3; hazard ratio [HR], 2.39; 95% CI, 1.15 to 4.98; P = 0.020) and 5-year overall survival (HR, 2.30; 95% CI, 1.23 to 4.30; P = 0.009) in multivariable analysis.
Although the majority of cases of rectal cancer are not diagnosed until they reach an advanced pathologic stage, the referral of symptomatic patients for clinical investigations is important for the early detection of rectal cancer [1,2] because about three-quarters of rectal cancers present with rectal bleeding, constipation, or changes in bowel habits [3,4]. However, the clinical relevance of constipation in rectal cancer is unknown, and recent clinical guidelines do not include constipation as a high-risk symptom [5], even though it is a common symptom in patients with rectal cancer [6].
Obstructive symptoms were reported as a marker for tumor progression in right colon cancer [7]. Furthermore, a previous study showed that preoperative obstruction predicted worse long-term prognosis of stage III colorectal cancer, and could help to identify patients with high-risk colorectal cancer [8], although this is a controversial issue [9]. Symptoms of colorectal cancer were reported to help identify the cancer site, and constipation was more prominent in left-sided cancer [10]. However, until recently, it was unknown whether patients with advanced rectal cancer develop severe constipation.
In studies assessing the oncologic relevance of constipation in rectal cancer, potential systemic error can be reduced by using a reliable scale for assessing constipation severity, homogeneity of tumor location, and controlled preoperative chemoradiotherapy. Since January 2005, we have routinely assessed constipation severity in patients with rectal cancer using the Cleveland Clinic Constipation Scoring System (CCSS). This system is compatible with objective physiologic findings, provides standardized assessment of constipation [11], and has been validated in clinical practice [12-15]. The objective of this study was to assess whether constipation severity is associated with pathologic progression in patients with rectal cancer who did not receive preoperative chemoradiotherapy.
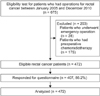
This prospective single-center, cohort study was designed to evaluate the clinical relevance of constipation severity in terms of the pathologic stage and prognosis of rectal cancer. We first screened 675 consecutive patients with rectal cancer who underwent resection between January 2005 and December 2010. All of the tumors were histologically classified as adenocarcinoma and were located ≤15 cm from the anal verge. We excluded patients who underwent emergency surgery for suspected bowel obstruction or perforation, and who could not complete the questionnaire. We also excluded patients who received prior chemoradiotherapy to avoid potential bias caused by down-staging of the primary tumor. The study was approved and overseen by the Institutional Review Board at Seoul National University Bundang Hospital.
The following factors were analyzed in this study: patient demographic factors, including age, sex, body mass index (BMI), and carcinoembryonic antigen (CEA); pathologic features, including tumor size and TNM classification; and oncologic data, including long-term survival and disease recurrence. The pathology reports were prepared according to the Guidelines of the College of American Pathologists [16]. Tumor staging was based on the American Joint Committee on Cancer guidelines [17].
Constipation score was self-reported by patients and the completed forms were collected by dedicated research nurses blinded to the study. We measured preoperative constipation severity using the Korean version of the CCSS. The CCSS, developed by Agachan et al. [11] consists of eight items: frequency of bowel movements, painful evacuation, incomplete evacuation, abdominal pain, length of time per attempt, assistance for evacuation, number of unsuccessful attempts of evacuation per 24 hours, and duration of constipation. Scores range from 0 to 30, and higher scores indicate more severe symptoms.
All patients were followed-up in accordance with a prespecified protocol. Follow-up visits were scheduled at 1 and 4 months after surgery, then every 3 months for the first 2 years, every 6 months for the next 3 years, and then every 12 months thereafter for 5 years. CEA serum levels were measured every 3 months, abdominal computed tomography and chest X-rays were performed every 6 months, and total colonoscopy was performed annually. All recurrences were diagnosed based on imaging and biopsy was performed if necessary. Recurrence was classified as local (i.e., around the anastomosis or within the region of the primary operation), systemic, or combined.
Our approach to managing missing data was to include only individuals with complete data for all variables included in multivariable analysis of constipation score and survival. Student t test, χ2 analysis/Fisher exact test, one-way analysis of variance, and multiple linear regression analysis were used to evaluate clinicopathological variables of relevance to the constipation score. Variables showing a significant correlation or a tendency toward an association (P < 0.20) were entered into the regression models using the forward selection method. Continuous variables were grouped using conventional cutoff values, such as age of 65 years old, BMI of 25 kg/m2, CEA of 5 ng/mL, and tumor size of 5 cm.
Survival data were obtained from the cancer registry, and the study population was classified into three groups according to tertiles of constipation score. The 3-year disease-free survival and 5-year overall survival curves were estimated using the Kaplan-Meier method, and differences in survival curves were compared using the log-rank test. Multivariable analysis were performed using the Cox proportional hazard model. All statistical tests were two-sided and were performed using the IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA). Values of P < 0.05 were considered to indicate statistical significance.
A total of 472 patients with rectal cancer underwent elective surgical resection without preoperative chemoradiotherapy and were eligible for analysis (Fig. 1). The response rate to the constipation questionnaire was 86.2%. The mean ± standard deviation constipation score was 5.29 ± 4.02, the median score was 4 (interquartile range [IQR], 2 to 8), and the distribution was skewed leftwards (Fig. 2).
Constipation scores were higher in the following groups of patients: females (P < 0.001), BMI < 25 kg/m2 (P = 0.031), larger tumor ≥5 cm (P < 0.001), advanced T stage (P < 0.001), lymph node positive (P = 0.001), and distant metastasis (P < 0.001) (Table 1). In multiple linear regression analysis, constipation severity was significantly associated with sex (regression coefficient [B] = 1.55; 95% confidence interval [CI], 0.79 to 2.60; P < 0.001), BMI (B = -0.95; 95% CI, -1.83 to -0.64; P = 0.036), tumor size (B = 1.04; 95% CI, 0.20 to 1.88; P = 0.016), T stage (B = 0.75; 95% CI, 0.23 to 1.27; P = 0.005), and distant metastasis (B = 1.16; 95% CI, 0.03 to 2.30; P = 0.045). The distribution of T stage was significantly different among tertiles of constipation score (P < 0.001) (Table 2).
After a median follow-up of 36 months (IQR, 23 to 59 months) of patients with stage I-III disease (n = 397), 52 (13.1%) showed disease recurrence. The recurrence rate was greater in patients with severe constipation (constipation score 0-3, 12.0%; score 4-7, 11.1%; score ≥8, 22.7%; P = 0.049) (Table 3). The 3-year disease-free survival rate was also significantly lower in patients with severe constipation than in patients with less severe constipation (constipation score 0-3, 87.6%; score 4-7, 88.9%; score ≥8, 77.9%; P = 0.047) (Table 4, Fig 3). Severe constipation (score ≥8 vs. score 0-3; hazard ratio [HR], 2.39; 95% CI, 1.15 to 4.98; P = 0.020) and TNM stage were independent prognostic factors for 3-year disease-free survival in multivariable analysis, after excluding T stage to reduce multicollinearity.
The median follow-up for stage I-IV patients (n = 472) was 44 months (IQR, 31 to 69 months). In univariable analysis, constipation score, age, CEA, tumor size, and TNM stage were associated with the 5-year overall survival rate (Table 5, Fig. 4). In multivariable analysis, severe constipation severity was an independent prognostic factor for 5-year overall survival rate (score ≥8; HR, 2.30; 95% CI, 1.23 to 4.30; P = 0.009), as were age and TNM stage.
This large-scale prospective cohort study showed that preoperative constipation severity is associated with the pathologic status of rectal cancer, including larger tumor size, locally advanced T stage, and distant metastasis. To our knowledge, this is the first study to show that constipation severity may be an independent prognostic factor in patients with rectal cancer.
In the present study, we investigated the association between oncologic outcomes of rectal cancer and preoperative constipation severity, which was measured using a quantitative scoring system (CCSS) because constipation may represent a combination of heterogeneous symptoms. We had a high response rate of 86.2% to CCSS [18]. This scoring system, which includes several well-designed questions, could reduce systemic error compared with previous studies that relied on the patient's subjective recall of symptoms [19]. The CCSS does not have a cutoff value for the diagnosis of constipation, although the mean score in a general population was reported to be 3.4 [11]. In this study, 22.3% of patients had a constipation score of ≥8, similar to the prevalence of constipation among patients with colorectal cancer in an earlier study [6].
We showed that constipation score was independently associated with recurrence-free or overall survival, while the association between TNM stage and mortality observed in this study is already well known. Our findings in patients with rectal cancer confirm those of a previous study, which suggested that obstruction may predict worse long-term prognosis in patients with colorectal cancer [7,8]. Our study also showed that age is a poor prognostic factor for overall survival but not for recurrence-free survival, as reported in a systematic review [20].
Several investigators showed that the duration of preoperative constipation was not associated with prognosis after colorectal cancer surgery [21]. That study assessed constipation in terms of its duration alone in a heterogeneous group of patients with colon and rectal cancer. They proposed that rectal bleeding, as a first symptom, was associated with lower mortality rates whereas mild anemia was associated with higher mortality rates.
We suggest that constipation may be an insidious symptom of rectal cancer to be developed to obstruction, and its effects differ from those of bleeding, which is complained at the early period of rectal cancer. We suggest that quantitative assessment of constipation severity provides more accurate information than its duration alone when assessing patients with rectal cancer, based on the results of oncologic analysis in this study.
The present study showed that tumor size, T stage, and distant metastasis were associated with constipation severity in rectal cancer, as well as female sex and lower BMI, as reported in previous studies [22,23]. Considering that larger tumors or advanced tumors in the rectum were associated with severe constipation, these results suggest that constipation in patients with rectal cancer may be caused by mass effect. In addition, we consider that advanced rectal cancer could affect for constipation severity by decreasing the compliance of rectum, which may be related to perineural invasion [24,25], lymphatic metastasis followed by obstruction [26,27], or inflammatory cytokines [28].
This study has some limitations. First, the Korean version of the CCSS has not been validated. However, the response rate was high, and the responses were considered to be reliable based on anonymous interviews that were conducted by independent nurses blinded to the study. Second, the etiology of constipation was not differentiated, and symptoms other than constipation were not evaluated, although rectal bleeding, weight loss, abdominal pain, and anemia was warranted for the diagnosis of colorectal cancer in a systematic review [29]. Nevertheless, the clinical relevance of constipation could be confirmed in a well-controlled study aimed at reducing selection bias, because constipation is common symptom in patients with rectal cancer [6]. Third, we excluded patients who had previously received chemoradiotherapy. Preoperative chemoradiotherapy is usually performed for rectal adenocarcinomas located ≤9 cm from the anal verge, which were clinically diagnosed as cT3, N0-2 lesions based on pelvic computed tomography, transanal ultrasonography, and magnetic resonance imaging in our previous study [30]. In this study, we excluded these patients to avoid possible systemic error because down-staging of tumor size as a result of chemoradiotherapy could affect constipation severity.
In conclusion, this study showed that preoperative constipation severity is associated with advanced pathologic stage and poor oncologic outcomes in patients with rectal cancer. To our knowledge, this is the first study that the oncologic relevance of constipation was revealed in the prospective cohort design using a quantitative measure. Based on these findings, severe constipation may be considered as a marker for high-risk group in rectal cancer.
Figures and Tables
Fig. 3
Kaplan-Meier analysis of 3-year disease-free survival in patients divided by tertiles of constipation score.
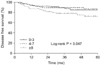
Fig. 4
Kaplan-Meier analysis of 5-year overall survival in patients divided by tertiles of constipation score.
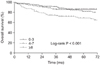
Table 1
Patients demographics and constipation-related factors (n = 472)

Values are presented as mean ± standard deviation or number (%).
B, regression coefficient; CI, confidence interval; CEA, carcinoembryonic antigen.
a)Multiple linear regression analysis. b)B indicates change of constipation score according to the incremental change of each variable. c)Student t-test. d)One-way analysis of variance.
References
1. John SK, George S, Primrose JN, Fozard JB. Symptoms and signs in patients with colorectal cancer. Colorectal Dis. 2011. 13:17–25.
2. Chen HM, Weng YR, Jiang B, Sheng JQ, Zheng P, Yu CG, et al. Epidemiological study of colorectal adenoma and cancer in symptomatic patients in China between 1990 and 2009. J Dig Dis. 2011. 12:371–378.
3. Barrett J, Jiwa M, Rose P, Hamilton W. Pathways to the diagnosis of colorectal cancer: an observational study in three UK cities. Fam Pract. 2006. 23:15–19.
4. Kim BP, Kwon KH, Min HS. A clinical study of colorectal cancer. J Korean Surg Soc. 1998. 54:374–382.
5. The National Collaborating Centre for Primary Care. Referral guidelines for suspected cancer. Issue date: June 2005 [Internet]. 2013. cited 2012 Jul 8. London: National Institute for Health and Clinical Excellence;Available from: http://www.nice.org.uk/nicemedia/pdf/cg027niceguideline.pdf.
6. Hamilton W, Round A, Sharp D, Peters TJ. Clinical features of colorectal cancer before diagnosis: a population-based case-control study. Br J Cancer. 2005. 93:399–405.
7. Wang HS, Lin JK, Mou CY, Lin TC, Chen WS, Jiang JK, et al. Long-term prognosis of patients with obstructing carcinoma of the right colon. Am J Surg. 2004. 187:497–500.
8. Katoh H, Yamashita K, Wang G, Sato T, Nakamura T, Watanabe M. Prognostic significance of preoperative bowel obstruction in stage III colorectal cancer. Ann Surg Oncol. 2011. 18:2432–2441.
9. Cho YB, Yun SH, Hong JS, Yun HR, Lee WS, Lee WY, et al. Carcinoma obstruction of the left colon and long-term prognosis. Hepatogastroenterology. 2008. 55:1288–1292.
10. Kent AJ, Woolf D, McCue J, Greenfield SM. The use of symptoms to predict colorectal cancer site. Can we reduce the pressure on our endoscopy services? Colorectal Dis. 2010. 12:114–118.
11. Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD. A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum. 1996. 39:681–685.
12. Boccasanta P, Venturi M, Salamina G, Cesana BM, Bernasconi F, Roviaro G. New trends in the surgical treatment of outlet obstruction: clinical and functional results of two novel transanal stapled techniques from a randomised controlled trial. Int J Colorectal Dis. 2004. 19:359–369.
13. Kenefick NJ, Nicholls RJ, Cohen RG, Kamm MA. Permanent sacral nerve stimulation for treatment of idiopathic constipation. Br J Surg. 2002. 89:882–888.
14. Altomare DF, Binda GA, Dodi G, La Torre F, Romano G, Rinaldi M, et al. Disappointing long-term results of the artificial anal sphincter for faecal incontinence. Br J Surg. 2004. 91:1352–1353.
15. Marchesi F, Sarli L, Percalli L, Sansebastiano GE, Veronesi L, Di Mauro D, et al. Subtotal colectomy with antiperistaltic cecorectal anastomosis in the treatment of slow-transit constipation: long-term impact on quality of life. World J Surg. 2007. 31:1658–1664.
16. Washington MK, Berlin J, Branton PA, Burgart LJ, Carter DK, Fitzgibbons PL, et al. Protocol for the examination of specimens from patients with primary carcinomas of the colon and rectum. Arch Pathol Lab Med. 2008. 132:1182–1193.
17. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual. 2010. 7th ed. New York: Springer.
18. Bove A, Pucciani F, Bellini M, Battaglia E, Bocchini R, Altomare DF, et al. Consensus statement AIGO/SICCR: diagnosis and treatment of chronic constipation and obstructed defecation (part I: diagnosis). World J Gastroenterol. 2012. 18:1555–1564.
19. Pamuk ON, Pamuk GE, Celik AF. Revalidation of description of constipation in terms of recall bias and visual scale analog questionnaire. J Gastroenterol Hepatol. 2003. 18:1417–1422.
20. Manceau G, Karoui M, Werner A, Mortensen NJ, Hannoun L. Comparative outcomes of rectal cancer surgery between elderly and non-elderly patients: a systematic review. Lancet Oncol. 2012. 13:e525–e536.
21. Stapley S, Peters TJ, Sharp D, Hamilton W. The mortality of colorectal cancer in relation to the initial symptom at presentation to primary care and to the duration of symptoms: a cohort study using medical records. Br J Cancer. 2006. 95:1321–1325.
22. Jeong JJ, Choi MG, Cho YS, Lee SG, Oh JH, Park JM, et al. Chronic gastrointestinal symptoms and quality of life in the Korean population. World J Gastroenterol. 2008. 14:6388–6394.
23. Jun DW, Park HY, Lee OY, Lee HL, Yoon BC, Choi HS, et al. A population-based study on bowel habits in a Korean community: prevalence of functional constipation and self-reported constipation. Dig Dis Sci. 2006. 51:1471–1477.
24. Kim HJ, Choi GS, Park JS, Park SY, Jun SH. Higher rate of perineural invasion in stent-laparoscopic approach in comparison to emergent open resection for obstructing left-sided colon cancer. Int J Colorectal Dis. 2013. 28:407–414.
25. Mulcahy HE, Skelly MM, Husain A, O'Donoghue DP. Long-term outcome following curative surgery for malignant large bowel obstruction. Br J Surg. 1996. 83:46–50.
26. Nickell DF, Dockerty MB. The 5 year survival rate in cases of completely obstructing annular carcinoma of the descending colon and sigmoid; a pathologic study. Surg Gynecol Obstet. 1948. 87:519–524.
27. Korenaga D, Ueo H, Mochida K, Kusumoto T, Baba H, Tamura S, et al. Prognostic factors in Japanese patients with colorectal cancer: the significance of large bowel obstruction--univariate and multivariate analyses. J Surg Oncol. 1991. 47:188–192.
28. Granger DN, Kvietys PR, Mortillaro NA, Taylor AE. Effect of luminal distension on intestinal transcapillary fluid exchange. Am J Physiol. 1980. 239:G516–G523.
29. Astin M, Griffin T, Neal RD, Rose P, Hamilton W. The diagnostic value of symptoms for colorectal cancer in primary care: a systematic review. Br J Gen Pract. 2011. 61:e231–e243.
30. Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol. 2010. 11:637–645.




 ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download