Abstract
Purpose
The genes p53 and B-cell lymphoma (bcl)-2 play an important role in regulating the mechanisms of apoptosis. In this paper, we retrospectively applied these factors to our series of triple negative breast cancer (TNBC) patients, in conjunction with an evaluation of the prognostic significance of these factors' influence on TNBC survival rate. Particular focus was placed on the role of bcl-2, p53, Ki-67.
Methods
The study subjects, 94 women with TNBC, were a subset of patients operated at Kosin University Gospel Hospital from January 2000 to December 2005. Chi-squared tests were used for statistical analysis.
Results
Positive staining for cytokeratin (CK)5/6 in 23 cases (24.5%), epidermal growth factor receptor in 15 cases (16.0%), bcl-2 in 26 cases (27.7%), p53 in 55 cases (58.5%) and Ki-67 in 74 cases (78.7%) was determined. Lymph node status, tumor size and expression of CK5/6 or Ki-67 were independent prognostic factors for patients with TNBC.
Conclusion
Markers regulating cell cycle and cell death such as p53 and bcl-2 cannot be used to classify TNBCs into two subtypes with differing disease-free survival. But because our study is small in size, more abundant patient data will be needed to evaluate the factors' predictive role in regulating cell cycle and cell death.
By using DNA microarray techniques, it has been shown that breast cancers can be classified into biologically distinct groups based on their gene expression profiles [1]. These groups comprise luminal A (estrogen receptor [ER]-positive and human epidermal growth factor receptor 2 [HER2]-negative), luminal B (ER- and HER2-positive), HER-2 (ER-negative and HER2-positive), and triple negative (ER- and HER2-negative) subtypes [2]. TNBC is a heterogeneous group and is further categorized into the basal-phenotype (BP) and non-BP groups, which are positive and negative, respectively, for myoepithelial/basal markers such as basal cytokeratins (CKs) (i.e., CK5/6, CK14, and CK17), and epidermal growth factor receptor (EGFR) [3,4]. Although TNBCs account for only 10 to 17% of all breast carcinomas, this subgroup is regarded as important clinically because of the aggressive clinical behavior, poorer patient prognosis, and lack of an established therapeutic target [5]. The ratio of basal-like subtype in TNBC was estimated to be up to 56 to 84%. Among the genes regulators of the apoptotic process, the tumor suppressor gene p53 and the B-cell lymphoma (bcl)-2 gene and its family members have been studied in clinical settings of breast cancer [1,6]. Among the several biomarkers, bcl-2 is an anti-apoptotic gene, and it is a poor prognostic factor in various malignant tumors. However, the prognostic significance of bcl-2 expression in breast cancer remains controversial [7]. We retrospectively applied these factors to our series of TNBC patients, in conjunction with an evaluation of the prognostic significance of these factors influencing TNBC survival rate. Particular focus was placed on the role of CK5/6, EGFR, bcl-2, and p53.
Tissue samples were obtained from 617 patients with invasive breast cancer who were diagnosed from 2000 to 2005 at Kosin University Gospel Hospital in Busan. A total of 617 specimens of primary invasive carcinoma were obtained from resected tumors. None of these cancer patients received treatment prior to surgery. The patients underwent standard and partial mastectomies. Patients received anthracycline-containing chemotherapy if the tumor was node positive. Endocrine therapy was given for 5 years to patients with ER-positive tumors. Median follow up was 5.5 years (range, 0.3 to 14.8 years), during which there were 84 relapses and 32 deaths.
The expression of ER, PgR, HER-2/neu, CK5/6 and other biological markers was determined immunohistochemically in paraffin-embedded tissue specimens [1,6]. Table 1 summarizes all the antibodies, dilutions, incubation times, and cutoff values used for this analysis. All data were collected from the pathology reports. Histopathological features such as hormone receptor status and HER-2/neu status on immunohistochemistry (Dako, Copenhagen, Denmark) were all analyzed at the Institute of Pathology at Kosin University. Expressions of p53, ER, Ki-67 and HER-2/neu were determined immunohistochemically on paraffin sections using antibodies against ER (Dako), Ki-67 (Dako), HER-2/neu (Dako), p53 (Dako) [1,8]. Tumor necrosis was defined as the presence of necrosis of any dimension in a section of invasive cancer. Histologic grading was performed using the criteria of Bloom and Richardson [9], ER status and progesterone receptor (PgR) status were taken as positive if more than 10% of tumor cells showed staining. Immunohistochemical score of 3+ or fluorescent in situ hybridization + for HER-2/neu was accepted as HER-2/neu positivity. Immunostaining for p53 and bcl-2 was performed on wax sections cut to a thickness of 5 µm, immersed in a citric acid buffer (pH 6.0) and incubated twice in a microwave oven at 750 W power for five minutes each. The sections were subsequently immunostained using the APAAP Complex method (Dako); the primary antibodies used for detection of p53 and bcl-2 were, respectively, the Immunotech antihuman p53 protein clone DO-7 (Immunotech, Marseille, France) and the DAKO antihuman bcl-2 oncoprotein clone 124 (Dako). Ki-67 proliferative activity was determined by the avidin-biotin procedure. Briefly, after inhibition of endogenous peroxidase, slides were incubated with Ki-67 monoclonal antibody (diluted 1:50 in phosphate buffered saline [PBS]) for 1 hour at room temperature. After quickly rinsing in PBS, the sections were incubated with biotin-conjugated rabbit antimouse immunoglobulin G (Vector Laboratories, Burlingame, CA, USA) for 30 minutes. After an additional wash in PBS, slides were incubated with avidin-biotin complexes conjugated with peroxidase (Vector Laboratories) for 45 minutes. The median value of Ki-67 was 10% and this was taken as the cut-off point distinguishing slowly from quickly proliferating tumors. The slides were scored by the same pathologist. We considered the tumor positive for p53 and bcl-2 when 10% or more of the cells counted were stained [7,10].
Statistical tests were performed using the SPSS ver. 12.0 (SPSS Inc, Chicago, IL, USA). The survival function was calculated from the time of the pathologic diagnosis to the occurrence of death. Survival data were censored on December 31, 2011, which was the date on which the survival data were correlated with the death registry for the last time or 5 years after the onset of the disease. Kaplan-Meier estimates are presented for the survival function, and differences in survival were analyzed using the log rank test. Associations between specific histopathological and clinical survival estimates and curves were established using the Kaplan-Meier method and differences in observed survival distribution among patient subgroups were tested with two-sided log-rank test. All survival rates were presented with their standard errors. We used Pearson's correlation to determine the association of pairs of explanatory variables, differences in qualitative variables were evaluated by chi-squared test, where necessary. The survival differences between patients with a basal phenotype TNBC and a non-BP TNBC were calculated with the Cox proportional hazards model. A P-value of <0.05 was considered to indicate statistical significance. All P-values were two-sided and a P-value of less than 0.05 was considered to indicate a statistically significant difference.
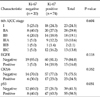
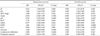
The main clinicopathological characteristics of the patients in our series are summarized in Table 2. Mean age was 54 years. Luminal A was reported in 166 patients (26.9%). Luminal B, HER-2/neu, and TNBC type were reported in 178 patients (28.9%), 162 patients (26.3%), 111 patients (17.9%), respectively. Among the 111 TNBC patients, seventeen had missing data as a result of a follow-up failure; thus, 94 TNBC patients are included in the final morphologic characteristics data set. Other reasons for ineligibility included incompetent specimen. Positive staining for CK5/6 was found in 23 cases (24.5%), 15 cases (16.0%) were determined as positive staining for EGFR. According to the positivity of CK5/6 and EGFR, 33 of the 94 patients (35.1%) had been diagnosed as basal phenotype TNBC and 61 patients (64.9%) had non-BP TNBC (Table 3). As compared with the non-basal TNBCs, basal TNBCs were not associated with a larger tumor size (P = 0.597), more advanced American Joint Committee on Cancer (AJCC) stage (P = 0.493) and shorter overall survival (OS, P = 0.438) and disease-free survival (DFS, P = 0.260). And bcl-2 in 26 cases (27.7%) and p53 in 55 cases (58.5%) was determined as positive staining. Tumor necrosis was found in 56 patients (59.6%) in TNBC. And infiltrating border was found in 70 patients (74.5%). Also continuous lymphocytic distribution and prominent nucleoli (>50%) was found in 35 patients (37.2%), and 45 patients (47.9%), respectively. No statistical relationship was found between bcl-2 positivity and other variables, such as tumor size, nodal status, AJCC stage, tumor grading, p53 and Ki-67 (Tables 4-6). At a median follow-up of 5.5 years, 84 patients (13.6%) had a recurrence, and 32 patients (5.2%) expired. Among TNBC, we observed 7 relapses in 61 patients (11.5%) with non-BP TNBC and 4 relapses in 33 patients (12.1%) with BP TNBC. The univariate analysis for prognostic factors associated with DFS revealed that the Ki-67 was statistically significant (P = 0.044). CK5/6 was also statistically significant (P = 0.034). Tumor group as T1, T2, T3, or T4, lymph node stage group as N0, N1, N2, or N3 was also significant (P = 0.008, P = 0.008 respectively) (Table 6). Also, the univariate analysis for prognostic factors associated with OS revealed that Ki-67, CK5/6 was statistically significant (P = 0.047, P = 0.036 respectively) (Figs. 1-4). Lymph node stage group as N0, N1, N2, or N3 was also statistically significant (P = 0.022) (Table 7).
Apoptosis, or programmed cell death, plays a major role not only in the formation and progression of cancer, but in the development of resistances to anticancer drugs as well [11]. The genes p53 and bcl-2 play an important role in regulating the mechanisms of apoptosis [12]. p53 is a tumor suppressor gene involved in the regulation of proliferative activity of human cells. Indeed, p53 serves a multifunctional role as a transcriptional regulator, genomic stabilizer, inhibitor of cell cycle progression, facilitator of apoptosis and also perhaps as inhibitor of angiogenesis [13]. By all these mechanisms, wild type p53 slows proliferation, while mutations of these gene in cancer cells may result in higher proliferation rates, higher genetic instability, and resistance to apoptosis [14]. Many studies have analyzed the prognostic impact of p53 alterations in breast cancer, and most of the studies have reported an association with worse outcome, either in node negative and node positive disease. However, others studies failed to demonstrate a significant association of p53 with poorer prognosis [8,11,15]. In our series, p53 over-expression was found in 60.0% of breast cancers, a value in line with the reported values between 11 and 60% of p53 mutation in breast cancer by immunohistochemistry, but did not correlate to either bcl-2 expression or to disease-free and overall survival. It has been recently accepted that gene sequencing is the most appropriate method to study p53 status; indeed different types of mutated p53 oncogene exist that do not determine protein accumulation and are therefore not detected by immunohistochemistry [15,16]. The discordance between our results and other studies may be partly due to the immunohistochemical technique used to detect p53 mutations and reflects the inconsistent data reported in literature for p53 mutation in breast cancer. The bcl-2 gene was initially identified in human bcls and its activity as apoptosis inhibitor, either drug and p53 induced, in cancer cells has been well demonstrated [7,10]. As a consequence, the expression of bcl-2 in breast cancer cells should inhibit apoptosis and therefore relate to a worse outcome [1]. On the contrary, the expression of bcl-2 in breast cancer has been found to be associated with favorable prognostic factors such as small tumor size, ER positivity, low nuclear grade and to predict a better outcome [7,10,17]. These unexpected results may be explained by the fact that the ability of bcl-2 to inhibit apoptosis depends on the intracellular balance among a number of its family members, with other pro-apoptotic members such as Bax counteracting its action [7,18]. Given its anti-apoptotic function, bcl-2 should be expected to correlate with worse prognosis. On the contrary, high levels of bcl-2 expression have been reported as associated to favorable tumor characteristics, such as low tumor size, low tumor grade, low proliferative activity and mainly with expression of ER and PgR [19]. These associations account for the favorable prognostic impacts reported for bcl-2 expression on DFS and OS in breast cancer, either node negative and node positive, even if an independent prognostic role has been confirmed only in some series [20,21]. Our data do not support the association of bcl-2 expression with other favorable prognostic factors and mainly with ERs expression, even if the percentages of bcl-2 and ERs expression in the study population are in line with the other series [22]. On the other hand, data regarding outcome in our series are consistent with other studies; that bcl-2 expression doesn't correlate with better outcome, either for DFS and OS. Reasons for this unfavorable prognostic value of bcl-2 expression are not clear; possible explanations may include the pro-apoptotic activity of other members of the bcl-2 family, an inhibitory activity of bcl-2 on cell proliferation or the estrogen-inducibility of bcl-2 expression [10]. In addition, data regarding outcome in our series are not consistent with other studies; that CK5/6 positivity correlates with better outcome, either for DFS and OS. Reasons for this favorable prognostic value of CK5/6 expression are not clear; possible explanations may include the small sample size, short-term follow-up period and no differences in survival rate between TNBC groups according to basal type.
In conclusion, paradoxically, CK5/6 positive TNBCs are higher DFS and OS than CK5/6 negative TNBCs. So, our study has some limitations in that CK5/6 can be used to classify TNBCs into at least two subtypes with differing survival rates. Also, the nuclear proliferation antigen, Ki-67, can be used to differentiate disease-free survival. But markers regulating cell cycle and cell death such as p53 and bcl-2 cannot be used to classify TNBCs into two subtypes with differing survival rates. However, because our study is small in size, there is no survival difference between TNBC groups according to basal type. So, more abundant patients' data will be needed to evaluate the pro-apoptotic activity of other members of the bcl-2 family's predictive role.
Figures and Tables
Fig. 1
Kaplan-Meier estimates of overall survival according to basal type. TNBC, triple negative breast cancer.

References
1. Nakagawa M, Bando Y, Nagao T, Morimoto M, Takai C, Ohnishi T, et al. Expression of p53, Ki-67, E-cadherin, N-cadherin and TOP2A in triple-negative breast cancer. Anticancer Res. 2011. 31:2389–2393.
2. Elnashar AT, Ali el-SM, Gaber A. The prognostic value of triple negative in stage II/III breast cancer. J Oncol Pharm Pract. 2012. 18:68–75.
3. Yerushalmi R, Tyldesley S, Kennecke H, Speers C, Woods R, Knight B, et al. Tumor markers in metastatic breast cancer subtypes: frequency of elevation and correlation with outcome. Ann Oncol. 2012. 23:338–345.
4. Montagna E, Bagnardi V, Rotmensz N, Viale G, Renne G, Cancello G, et al. Breast cancer subtypes and outcome after local and regional relapse. Ann Oncol. 2012. 23:324–331.
5. Skarlos P, Christodoulou C, Kalogeras KT, Eleftheraki AG, Bobos M, Batistatou A, et al. Triple-negative phenotype is of adverse prognostic value in patients treated with dose-dense sequential adjuvant chemotherapy: a translational research analysis in the context of a Hellenic Cooperative Oncology Group (HeCOG) randomized phase III trial. Cancer Chemother Pharmacol. 2012. 69:533–546.
6. Nishimura R, Osako T, Okumura Y, Tashima R, Toyozumi Y, Arima N. Changes in the ER, PgR, HER2, p53 and Ki-67 biological markers between primary and recurrent breast cancer: discordance rates and prognosis. World J Surg Oncol. 2011. 9:131.
7. Kallel-Bayoudh I, Hassen HB, Khabir A, Boujelbene N, Daoud J, Frikha M, et al. Bcl-2 expression and triple negative profile in breast carcinoma. Med Oncol. 2011. 28:Suppl 1. S55–S61.
8. Chae BJ, Bae JS, Lee A, Park WC, Seo YJ, Song BJ, et al. p53 as a specific prognostic factor in triple-negative breast cancer. Jpn J Clin Oncol. 2009. 39:217–224.
9. Collins LC, Marotti JD, Gelber S, Cole K, Ruddy K, Kereakoglow S, et al. Pathologic features and molecular phenotype by patient age in a large cohort of young women with breast cancer. Breast Cancer Res Treat. 2012. 131:1061–1066.
10. Tawfik K, Kimler BF, Davis MK, Fan F, Tawfik O. Prognostic significance of Bcl-2 in invasive mammary carcinomas: a comparative clinicopathologic study between "triple-negative" and non-"triple-negative" tumors. Hum Pathol. 2012. 43:23–30.
11. Lee DS, Kim SH, Suh YJ, Kim S, Kim HK, Shim BY. Clinical implication of p53 overexpression in breast cancer patients younger than 50 years with a triple-negative subtype who undergo a modified radical mastectomy. Jpn J Clin Oncol. 2011. 41:854–866.
12. Jiang Z, Jones R, Liu JC, Deng T, Robinson T, Chung PE, et al. RB1 and p53 at the crossroad of EMT and triple-negative breast cancer. Cell Cycle. 2011. 10:1563–1570.
13. Lee DS, Kim SH, Kim S, Suh YJ, Kim HK, Shim BY. Prognostic significance of breast cancer subtype and p53 overexpression in patients with locally advanced or high-risk breast cancer treated using upfront modified radical mastectomy with or without post-mastectomy radiation therapy. Int J Clin Oncol. 2011. 09. 07. [Epub]. http://dx.doi.org/10.1007/s10147-011-0309-0.
14. Biganzoli E, Coradini D, Ambrogi F, Garibaldi JM, Lisboa P, Soria D, et al. p53 status identifies two subgroups of triple-negative breast cancers with distinct biological features. Jpn J Clin Oncol. 2011. 41:172–179.
15. Guarneri V, Barbieri E, Piacentini F, Giovannelli S, Ficarra G, Frassoldati A, et al. Predictive and prognostic role of p53 according to tumor phenotype in breast cancer patients treated with preoperative chemotherapy: a single-institution analysis. Int J Biol Markers. 2010. 25:104–111.
16. Jung SY, Jeong J, Shin SH, Kwon Y, Kim EA, Ko KL, et al. Accumulation of p53 determined by immunohistochemistry as a prognostic marker in node negative breast cancer; analysis according to St Gallen consensus and intrinsic subtypes. J Surg Oncol. 2011. 103:207–211.
17. Moran MS, Yang Q, Haffty BG. The Yale University experience of early-stage invasive lobular carcinoma (ILC) and invasive ductal carcinoma (IDC) treated with breast conservation treatment (BCT): analysis of clinical-pathologic features, long-term outcomes, and molecular expression of COX-2, Bcl-2, and p53 as a function of histology. Breast J. 2009. 15:571–578.
18. Tawfik O, Davis K, Kimler BF, Davis MK, Hull S, Fan F, et al. Clinicopathological characteristics of triple-negative invasive mammary carcinomas in African-American versus Caucasian women. Ann Clin Lab Sci. 2010. 40:315–323.
19. Broustas CG, Ross JS, Yang Q, Sheehan CE, Riggins R, Noone AM, et al. The proapoptotic molecule BLID interacts with Bcl-XL and its downregulation in breast cancer correlates with poor disease-free and overall survival. Clin Cancer Res. 2010. 16:2939–2948.
20. Rhee J, Han SW, Oh DY, Kim JH, Im SA, Han W, et al. The clinicopathologic characteristics and prognostic significance of triple-negativity in node-negative breast cancer. BMC Cancer. 2008. 8:307.
21. Nozoe T, Mori E, Kono M, Iguchi T, Maeda T, Matsukuma A, et al. Serum appearance of anti-p53 antibody in triple negative breast cancer. Breast Cancer. 2012. 19:11–15.
22. Keam B, Im SA, Kim HJ, Oh DY, Kim JH, Lee SH, et al. Prognostic impact of clinicopathologic parameters in stage II/III breast cancer treated with neoadjuvant docetaxel and doxorubicin chemotherapy: paradoxical features of the triple negative breast cancer. BMC Cancer. 2007. 7:203.




 ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download