1. Song WJ, Chang YS, Faruqi S, Kim JY, Kang MG, Kim S, et al. The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J. 2015; 45:1479–1481. PMID:
25657027.

2. Kang MG, Song WJ, Kim HJ, Won HK, Sohn KH, Kang SY, et al. Point prevalence and epidemiological characteristics of chronic cough in the general adult population: The Korean National Health and Nutrition Examination Survey 2010–2012. Medicine (Baltimore). 2017; 96:e6486. PMID:
28353590.
3. Song WJ, Faruqi S, Klaewsongkram J, Lee SE, Chang YS. Chronic cough: an Asian perspective. Part 1: epidemiology. Asia Pac Allergy. 2015; 5:136–144. PMID:
26240790.

4. Morice AH. Epidemiology of cough. Pulm Pharmacol Ther. 2002; 15:253–259. PMID:
12099774.

5. French CL, Irwin RS, Curley FJ, Krikorian CJ. Impact of chronic cough on quality of life. Arch Intern Med. 1998; 158:1657–1661. PMID:
9701100.

6. Birring SS, Prudon B, Carr AJ, Singh SJ, Morgan MD, Pavord ID. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ). Thorax. 2003; 58:339–343. PMID:
12668799.

7. Kwon JW, Moon JY, Kim SH, Song WJ, Kim MH, Kang MG, et al. Reliability and validity of a Korean version of the Leicester Cough Questionnaire. Allergy Asthma Immunol Res. 2015; 7:230–233. PMID:
25749761.

8. Song WJ, Morice AH, Kim MH, Lee SE, Jo EJ, Lee SM, et al. Cough in the elderly population: relationships with multiple comorbidity. PLoS One. 2013; 8:e78081. PMID:
24205100.

9. Hulme K, Dogan S, Parker SM, Deary V. ‘Chronic cough, cause unknown’: a qualitative study of patient perspectives of chronic refractory cough. J Health Psychol. 2017; 1359105316684204. PMID:
28810370.

10. Song WJ, Morice AH. Cough hypersensitivity syndrome: a few more steps forward. Allergy Asthma Immunol Res. 2017; 9:394–402. PMID:
28677352.

11. Morice AH, Millqvist E, Belvisi MG, Bieksiene K, Birring SS, Chung KF, et al. Expert opinion on the cough hypersensitivity syndrome in respiratory medicine. Eur Respir J. 2014; 44:1132–1148. PMID:
25142479.

12. Morice AH, Jakes AD, Faruqi S, Birring SS, McGarvey L, Canning B, et al. A worldwide survey of chronic cough: a manifestation of enhanced somatosensory response. Eur Respir J. 2014; 44:1149–1155. PMID:
25186267.

13. Chung KF, Pavord ID. Prevalence, pathogenesis, and causes of chronic cough. Lancet. 2008; 371:1364–1374. PMID:
18424325.

14. Irwin RS, Baumann MH, Bolser DC, Boulet LP, Braman SS, Brightling CE, et al. Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129:1S–23S. PMID:
16428686.
15. Morice AH, Fontana GA, Sovijarvi AR, Pistolesi M, Chung KF, Widdicombe J, et al. The diagnosis and management of chronic cough. Eur Respir J. 2004; 24:481–492. PMID:
15358710.

16. Birring SS, Kavanagh J, Lai K, Chang AB. Adult and paediatric cough guidelines: ready for an overhaul? Pulm Pharmacol Ther. 2015; 35:137–144. PMID:
25681276.

17. Gibson P, Wang G, McGarvey L, Vertigan AE, Altman KW, Birring SS, et al. Treatment of unexplained chronic cough: CHEST guideline and expert panel report. Chest. 2016; 149:27–44. PMID:
26426314.
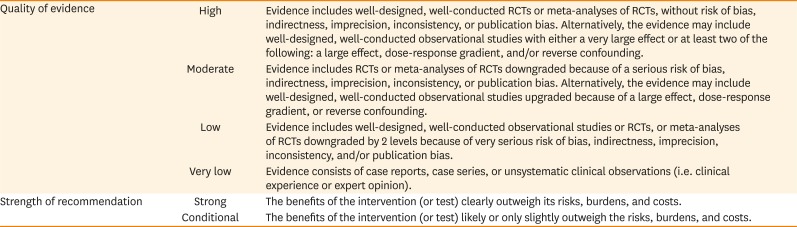
18. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011; 64:383–394. PMID:
21195583.

19. Houghton LA, Lee AS, Badri H, DeVault KR, Smith JA. Respiratory disease and the oesophagus: reflux, reflexes and microaspiration. Nat Rev Gastroenterol Hepatol. 2016; 13:445–460. PMID:
27381074.

20. Lilienfield LS, Rose JC, Princiotto JV. Antitussive activity of diphenhydramine in chronic cough. Clin Pharmacol Ther. 1976; 19:421–425. PMID:
773581.

21. Tanaka S, Hirata K, Kurihara N, Yoshikawa J, Takeda T. Effect of loratadine, an H1 antihistamine, on induced cough in non-asthmatic patients with chronic cough. Thorax. 1996; 51:810–814. PMID:
8795669.

22. Fujimori K, Suzuki E, Arakawa M. Effects of oxatomide, H1-antagonist, on postinfectious chronic cough; a comparison of oxatomide combined with dextromethorphan versus dextromethorphan alone. Arerugi. 1998; 47:48–53. PMID:
9528165.
23. van Asperen PP, McKay KO, Mellis CM, Loh RK, Harth SC, Thong YH, et al. A multicentre randomized placebo-controlled double-blind study on the efficacy of Ketotifen in infants with chronic cough or wheeze. J Paediatr Child Health. 1992; 28:442–446. PMID:
1466940.

24. Ciprandi G, Tosca M, Ricca V, Passalacqua G, Riccio AM, Bagnasco M, et al. Cetirizine treatment of rhinitis in children with pollen allergy: evidence of its antiallergic activity. Clin Exp Allergy. 1997; 27:1160–1166. PMID:
9383256.

25. Shields MD, Bush A, Everard ML, McKenzie S, Primhak R. British Thoracic Society Cough Guideline Group. BTS guidelines: recommendations for the assessment and management of cough in children. Thorax. 2008; 63(Suppl 3):iii1–iii15. PMID:
17905822.
26. Chang AB, Oppenheimer JJ, Weinberger MM, Rubin BK, Weir K, Grant CC, et al. Use of management pathways or algorithms in children with chronic cough: CHEST guideline and expert panel report. Chest. 2017; 151:875–883. PMID:
28104362.
27. Chaudhuri R, McMahon AD, Thomson LJ, MacLeod KJ, McSharry CP, Livingston E, et al. Effect of inhaled corticosteroids on symptom severity and sputum mediator levels in chronic persistent cough. J Allergy Clin Immunol. 2004; 113:1063–1070. PMID:
15208586.

28. Ribeiro M, Pereira CA, Nery LE, Beppu OS, Silva CO. High-dose inhaled beclomethasone treatment in patients with chronic cough: a randomized placebo-controlled study. Ann Allergy Asthma Immunol. 2007; 99:61–68. PMID:
17650832.

29. Pizzichini MM, Pizzichini E, Parameswaran K, Clelland L, Efthimiadis A, Dolovich J, et al. Nonasthmatic chronic cough: no effect of treatment with an inhaled corticosteroid in patients without sputum eosinophilia. Can Respir J. 1999; 6:323–330. PMID:
10463960.
30. Davies MJ, Fuller P, Picciotto A, McKenzie SA. Persistent nocturnal cough: randomised controlled trial of high dose inhaled corticosteroid. Arch Dis Child. 1999; 81:38–44. PMID:
10373132.

31. Mincheva RK, Kralimarkova TZ, Rasheva M, Dimitrov Z, Nedeva D, Staevska M, et al. A real-life observational pilot study to evaluate the effects of two-week treatment with montelukast in patients with chronic cough. Cough. 2014; 10:2. PMID:
24649919.

32. Wang K, Birring SS, Taylor K, Fry NK, Hay AD, Moore M, et al. Montelukast for postinfectious cough in adults: a double-blind randomised placebo-controlled trial. Lancet Respir Med. 2014; 2:35–43. PMID:
24461900.

33. Spector SL, Tan RA. Effectiveness of montelukast in the treatment of cough variant asthma. Ann Allergy Asthma Immunol. 2004; 93:232–236. PMID:
15478381.

34. Dicpinigaitis PV, Dobkin JB, Reichel J. Antitussive effect of the leukotriene receptor antagonist zafirlukast in subjects with cough-variant asthma. J Asthma. 2002; 39:291–297. PMID:
12095178.

35. Bao W, Liu P, Qiu Z, Yu L, Hang J, Gao X, et al. Efficacy of add-on montelukast in nonasthmatic eosinophilic bronchitis: the additive effect on airway inflammation, cough and life quality. Chin Med J (Engl). 2015; 128:39–45. PMID:
25563311.
36. Kooi EM, Schokker S, Marike Boezen H, de Vries TW, Vaessen-Verberne AA, van der Molen T, et al. Fluticasone or montelukast for preschool children with asthma-like symptoms: randomized controlled trial. Pulm Pharmacol Ther. 2008; 21:798–804. PMID:
18647656.

37. Kopřiva F, Sobolová L, Szotkowská J, Zápalka M. Treatment of chronic cough in children with montelukast,a leukotriene receptor antagonist. J Asthma. 2004; 41:715–720. PMID:
15584630.
38. Faruqi S, Molyneux ID, Fathi H, Wright C, Thompson R, Morice AH. Chronic cough and esomeprazole: a double-blind placebo-controlled parallel study. Respirology. 2011; 16:1150–1156. PMID:
21707852.

39. Kahrilas PJ, Howden CW, Hughes N, Molloy-Bland M. Response of chronic cough to acid-suppressive therapy in patients with gastroesophageal reflux disease. Chest. 2013; 143:605–612. PMID:
23117307.

40. Rane PP, Guha S, Chatterjee S, Aparasu RR. Prevalence and predictors of non-evidence based proton pump inhibitor use among elderly nursing home residents in the US. Res Social Adm Pharm. 2017; 13:358–363. PMID:
27033427.

41. Yadlapati R, Kahrilas PJ. The “dangers” of chronic proton pump inhibitor use. J Allergy Clin Immunol. 2018; 141:79–81. PMID:
28729001.

42. Kahrilas PJ, Altman KW, Chang AB, Field SK, Harding SM, Lane AP, et al. Chronic cough due to gastroesophageal reflux in adults: CHEST guideline and expert panel report. Chest. 2016; 150:1341–1360. PMID:
27614002.
43. Gibson PG, Dolovich J, Denburg J, Ramsdale EH, Hargreave FE. Chronic cough: eosinophilic bronchitis without asthma. Lancet. 1989; 333:1346–1348.

44. Kang SY, Kim GW, Song WJ, Chang YS, Cho SH. Chronic cough in Korean adults: a literature review on common comorbidity. Asia Pac Allergy. 2016; 6:198–206. PMID:
27803879.

45. Lim KH, Kim MH, Yang MS, Song WJ, Jung JW, Lee J, et al. The KAAACI Standardization Committee Report on the procedure and application of the bronchial provocation tests. Allergy Asthma Respir Dis. 2018; 6:14–25.

46. Kim MH, Kim MY, Lim KH, Yang MS, Song WJ, Lee J, et al. KAAACI Standardization Committee report on the procedure and application of induced sputum examination. Allergy Asthma Respir Dis. 2017; 5:307–311.

47. Alving K, Malinovschi A. Basic aspects of exhaled nitric oxide. Eur Respir Monogr. 2010; 49:1–31.

48. Song WJ, Kwon JW, Kim EJ, Lee SM, Kim SH, Lee SY, et al. Clinical application of exhaled nitric oxide measurements in a Korean population. Allergy Asthma Immunol Res. 2015; 7:3–13. PMID:
25553257.

49. Song WJ, Kim HJ, Shim JS, Won HK, Kang SY, Sohn KH, et al. Diagnostic accuracy of fractional exhaled nitric oxide measurement in predicting cough-variant asthma and eosinophilic bronchitis in adults with chronic cough: a systematic review and meta-analysis. J Allergy Clin Immunol. 2017; 140:701–709. PMID:
28088474.
50. Kwon JW, Song WJ, Kim MH, Lim KH, Yang MS, Jung JW, et al. The KAAACI Standardization Committee Report on the procedure and application of fractional exhaled nitric oxide measurement. Allergy Asthma Respir Dis. 2017; 5:185–192.

51. Song WJ, Won HK, Moon SD, Chung SJ, Kang SY, Sohn KH, et al. Could fractional exhaled nitric oxide test be useful in predicting inhaled corticosteroid responsiveness in chronic cough? A systematic review. J Allergy Clin Immunol Pract. 2017; 5:135–143.e1. PMID:
27707661.

52. Agache I, Rogozea L. Asthma biomarkers: do they bring precision medicine closer to the clinic? Allergy Asthma Immunol Res. 2017; 9:466–476. PMID:
28913985.

53. Oh MJ, Lee JY, Lee BJ, Choi DC. Exhaled nitric oxide measurement is useful for the exclusion of nonasthmatic eosinophilic bronchitis in patients with chronic cough. Chest. 2008; 134:990–995. PMID:
18583518.

54. Cao X, Wu Y. Measurement of fractional nitric oxide concentration in exhaled breath to assess cough variant asthma in child patients. Acta Acad Med Xuzhou. 2015; 35:328–330.
55. Ji X, Wang K, Chen J, Zhou X, Wang D, Zheng C. Clinical significance of fractional exhaled nitric oxide test in children with chronic cough. China Mod Dr. 2013; 20:42–45.
56. Wang T, Shang Y, Zhang H, Liu F, Feng Y. Clinical value of expired nitric oxide level in predicting bronchial hyperreactivity in children with chronic cough. Chin J Pract Pediatr. 2015; 30:203–206.
57. Zhu H, Yu X, Hao C, Wang Y, Yang X, Lu Y, et al. The diagnostic value of the fractional exhaled nitric oxide for cough variant asthma in children. Zhonghua Jie He He Hu Xi Za Zhi. 2015; 38:352–355. PMID:
26463486.
58. Korevaar DA, Westerhof GA, Wang J, Cohen JF, Spijker R, Sterk PJ, et al. Diagnostic accuracy of minimally invasive markers for detection of airway eosinophilia in asthma: a systematic review and meta-analysis. Lancet Respir Med. 2015; 3:290–300. PMID:
25801413.

59. Marchant JM, Masters IB, Taylor SM, Cox NC, Seymour GJ, Chang AB. Evaluation and outcome of young children with chronic cough. Chest. 2006; 129:1132–1141. PMID:
16685002.

60. Chang AB, Upham JW, Masters IB, Redding GR, Gibson PG, Marchant JM, et al. Protracted bacterial bronchitis: The last decade and the road ahead. Pediatr Pulmonol. 2016; 51:225–242. PMID:
26636654.

61. Chang AB, Glomb WB. Guidelines for evaluating chronic cough in pediatrics: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129:260S–283S. PMID:
16428719.
62. Chang AB, Landau LI, Van Asperen PP, Glasgow NJ, Robertson CF, Marchant JM, et al. Cough in children: definitions and clinical evaluation. Med J Aust. 2006; 184:398–403. PMID:
16618239.

63. Marchant J, Masters IB, Champion A, Petsky H, Chang AB. Randomised controlled trial of amoxycillin clavulanate in children with chronic wet cough. Thorax. 2012; 67:689–693. PMID:
22628120.

64. Chang AB, Oppenheimer JJ, Weinberger MM, Rubin BK, Grant CC, Weir K, et al. Management of children with chronic wet cough and protracted bacterial bronchitis: CHEST Guideline and Expert Panel Report. Chest. 2017; 151:884–890. PMID:
28143696.
65. Song WJ, Chang YS, Morice AH. Changing the paradigm for cough: does ‘cough hypersensitivity’ aid our understanding? Asia Pac Allergy. 2014; 4:3–13. PMID:
24527404.

66. Chung KF, McGarvey L, Mazzone SB. Chronic cough as a neuropathic disorder. Lancet Respir Med. 2013; 1:414–422. PMID:
24429206.

67. Morice AH, Menon MS, Mulrennan SA, Everett CF, Wright C, Jackson J, et al. Opiate therapy in chronic cough. Am J Respir Crit Care Med. 2007; 175:312–315. PMID:
17122382.

68. Ryan NM, Birring SS, Gibson PG. Gabapentin for refractory chronic cough: a randomised, double-blind, placebo-controlled trial. Lancet. 2012; 380:1583–1589. PMID:
22951084.

69. Ando A, Smallwood D, McMahon M, Irving L, Mazzone SB, Farrell MJ. Neural correlates of cough hypersensitivity in humans: evidence for central sensitisation and dysfunctional inhibitory control. Thorax. 2016; 71:323–329. PMID:
26860344.

70. Cass LJ, Frederik WS. Evaluation of a new antitussive agent. N Engl J Med. 1953; 249:132–136. PMID:
13063699.

71. Cass LJ, Frederik WS. Quantitative comparison of cough-suppressing effects of romilar and other antitussives. J Lab Clin Med. 1956; 48:879–885. PMID:
13376983.
72. Kirchheiner J, Schmidt H, Tzvetkov M, Keulen JT, Lötsch J, Roots I, et al. Pharmacokinetics of codeine and its metabolite morphine in ultra-rapid metabolizers due to CYP2D6 duplication. Pharmacogenomics J. 2007; 7:257–265. PMID:
16819548.

73. Vertigan AE, Kapela SL, Ryan NM, Birring SS, McElduff P, Gibson PG. Pregabalin and speech pathology combination therapy for refractory chronic cough: a randomized controlled trial. Chest. 2016; 149:639–648. PMID:
26447687.
74. Jeyakumar A, Brickman TM, Haben M. Effectiveness of amitriptyline versus cough suppressants in the treatment of chronic cough resulting from postviral vagal neuropathy. Laryngoscope. 2006; 116:2108–2112. PMID:
17146380.

75. Vertigan AE, Theodoros DG, Gibson PG, Winkworth AL. Efficacy of speech pathology management for chronic cough: a randomised placebo controlled trial of treatment efficacy. Thorax. 2006; 61:1065–1069. PMID:
16844725.

76. Chamberlain Mitchell SA, Garrod R, Clark L, Douiri A, Parker SM, Ellis J, et al. Physiotherapy, and speech and language therapy intervention for patients with refractory chronic cough: a multicentre randomised control trial. Thorax. 2017; 72:129–136. PMID:
27682331.

77. Petitti DB, Teutsch SM, Barton MB, Sawaya GF, Ockene JK, DeWitt T, et al. Update on the methods of the U.S. Preventive Services Task Force: insufficient evidence. Ann Intern Med. 2009; 150:199–205. PMID:
19189910.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download