Abstract
Purpose
To investigate whether causes of anaphylaxis vary according to regions and seasons in Korean adults.
Methods
Based on previous retrospective studies of anaphylaxis between 2007 and 2011 at the 15 university hospitals. Regions were classified into 4 groups: region I, Seoul; region II, Gyeonggi; region III, Chungcheong; and region IV, Chonnam and Busan. The cases induced by 5 major allergens including drugs, food, bee sting, radiocontrast media, and exercise, were analyzed in the present study.
Results
Among a total of 1,661 cases reported (53% male, 45.9±16.0 years), 367 (22.2%), 706 (42.5%), 319 (19.2%), and 269 cases (16.2%) were enrolled in regions I, II, III, and IV, respectively. Of the 5 major allergens, drugs (37.3%) were the most frequently reported, followed by food (25.7%), bee sting (17.9%), radiocontrast media (12.9%), and exercise (6.2%). There was no significant difference in the total occurrence of anaphylaxis in 4 seasons (374 in spring, 460 in summer, 460 in autumn, and 367 in winter). Multiple logistic regression analysis revealed that drug-induced anaphylaxis was significantly associated with the winter season (odds ratio [OR] 1.0 vs. OR 0.597, P<0.05 for spring; OR 1.0 vs. OR 0.481, P<0.01 for summer; OR 1.0 vs. OR 0.653, P<0.05 for autumn). Food-associated anaphylaxis was mainly reported in region I, whereas the frequency of insect sting was relatively higher in regions II, III, and IV than in region I. Older age and female gender were significantly associated with drug-induced anaphylaxis.
Figures and Tables
Fig. 1
Seasonal variations in the proportion of 5 common causes of anaphylaxis. RCM, radiocontrast media.
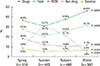
Fig. 2
Classification of regions and reported numbers of anaphylaxis cases according to the regions. SN, Seoul National University Hospital; AS, Asan Medical Center; KK, Korea University Guro Hospital; HY, Hanyang University Medical Center; AJ, Ajou University Hospital; DG, Dongguk University Ilsan Hospital; IH, Inha University Hospital; IS, National Health Insurance Service Ilsan Hospital; HL, Hallym University Sacred Heart Hospital; CB, Chungbuk National University Hospital; DK, Dankook University Hospital; PS, Pusan National University Hospital; CN, Chonnam National University Hospital; KS, Kosin University Gospel Hospital; DA, Dong-A University Hospital.

Table 1
Clinical characteristics of study population

Table 2
Multiple logistic regression analysis for the specific causalities of anaphylaxis

References
1. Simons FE, Ardusso LR, Bilo MB, El-Gamal YM, Ledford DK, Ring J, et al. World allergy organization guidelines for the assessment and management of anaphylaxis. World Allergy Organ J. 2011; 4:13–37.

4. Wood RA, Camargo CA Jr, Lieberman P, Sampson HA, Schwartz LB, Zitt M, et al. Anaphylaxis in America: the prevalence and characteristics of anaphylaxis in the United States. J Allergy Clin Immunol. 2014; 133:461–467.

5. Panesar SS, Javad S, de Silva D, Nwaru BI, Hickstein L, Muraro A, et al. The epidemiology of anaphylaxis in Europe: a systematic review. Allergy. 2013; 68:1353–1361.

7. Ye YM, Kim MK, Kang HR, Kim TB, Sohn SW, Koh YI, et al. Predictors of the severity and serious outcomes of anaphylaxis in korean adults: a multicenter retrospective case study. Allergy Asthma Immunol Res. 2015; 7:22–29.

8. Muraro A, Roberts G, Worm M, Bilo MB, Brockow K, Fernandez Rivas M, et al. Anaphylaxis: guidelines from the European Academy of Allergy and Clinical Immunology. Allergy. 2014; 69:1026–1045.

9. Russell WS, Farrar JR, Nowak R, Hays DP, Schmitz N, Wood J, et al. Evaluating the management of anaphylaxis in US emergency departments: Guidelines vs. practice. World J Emerg Med. 2013; 4:98–106.

10. Jang GC, Chang YS, Choi SH, Song WJ, Lee SY, Park HS, et al. Overview of anaphylaxis in Korea: diagnosis and management. Allergy Asthma Respir Dis. 2013; 1:181–196.

11. Koplin JJ, Martin PE, Allen KJ. An update on epidemiology of anaphylaxis in children and adults. Curr Opin Allergy Clin Immunol. 2011; 11:492–496.

12. Sicherer SH, Leung DY. Advances in allergic skin disease, anaphylaxis, and hypersensitivity reactions to foods, drugs, and insects in 2013. J Allergy Clin Immunol. 2014; 133:324–334.

13. Jerschow E, Lin RY, Scaperotti MM, McGinn AP. Fatal anaphylaxis in the United States, 1999-2010: temporal patterns and demographic associations. J Allergy Clin Immunol. 2014; 134:1318–1328.e7.

15. Rudders SA, Espinola JA, Camargo CA Jr. North-south differences in US emergency department visits for acute allergic reactions. Ann Allergy Asthma Immunol. 2010; 104:413–416.

16. Sheikh A, Alves B. Age, sex, geographical and socio-economic variations in admissions for anaphylaxis: analysis of four years of English hospital data. Clin Exp Allergy. 2001; 31:1571–1576.

17. Harduar-Morano L, Simon MR, Watkins S, Blackmore C. A populationbased epidemiologic study of emergency department visits for anaphylaxis in Florida. J Allergy Clin Immunol. 2011; 128:594–600.e1.

18. Decker WW, Campbell RL, Manivannan V, Luke A, St Sauver JL, Weaver A, et al. The etiology and incidence of anaphylaxis in Rochester, Minnesota: a report from the Rochester Epidemiology Project. J Allergy Clin Immunol. 2008; 122:1161–1165.

19. Camargo CA Jr, Clark S, Kaplan MS, Lieberman P, Wood RA. Regional differences in EpiPen prescriptions in the United States: the potential role of vitamin D. J Allergy Clin Immunol. 2007; 120:131–136.

20. Mullins RJ, Clark S, Camargo CA Jr. Regional variation in epinephrine autoinjector prescriptions in Australia: more evidence for the vitamin Danaphylaxis hypothesis. Ann Allergy Asthma Immunol. 2009; 103:488–495.

21. Yang MS, Lee SH, Kim TW, Kwon JW, Lee SM, Kim SH, et al. Epidemiologic and clinical features of anaphylaxis in Korea. Ann Allergy Asthma Immunol. 2008; 100:31–36.

22. Kim MJ, Choi GS, Um SJ, Sung JM, Shin YS, Park HJ, et al. Anaphylaxis; 10 years' experience at a university hospital in Suwon. Korean J Asthma Allergy Clin Immunol. 2008; 28:298–304.
23. Lee MY, Hong IP, Choi YS, Kim NS, Kim HK, Lee KG, et al. Present status of Korean beekeeping industry. Korean J Apiculture. 2010; 25:137–144.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download