Abstract
Anthrax, caused by Bacillus anthracis, is a non-contagious infectious disease that affects a wide range of animal species (primarily ruminants) including humans. Due to the often-fatal outcome in humans, quick administration of definitely effective antimicrobials is crucial either as prophylaxis or as a clinical case therapy. In this study, 110 B. anthracis strains, temporally, geographically, and genetically different, isolated during anthrax outbreaks in Italy from 1984 to 2017, were screened using a broth microdilution method to determine their susceptibility to 16 clinically relevant antimicrobial agents. The strains were isolated from various matrices (human, animal, and environmental samples) and were representative of thirty distinct genotypes previously identified by 15-loci multiple-locus variable-number of tandem repeats analysis. The antimicrobials tested were gentamicin, ceftriaxone, streptomycin, penicillin G, clindamycin, chloramphenicol, vancomycin, linezolid, cefotaxime, tetracycline, erythromycin, rifampin, amoxicillin, ciprofloxacin, doxycycline, and trimethoprim. All isolates were susceptible to most of the tested antimicrobials, with the exception of trimethoprim for which all of them showed high minimal inhibitory concentration values. An intermediate level of susceptibility was recorded for ceftriaxone and cefotaxime. Although the Centers for Disease Control and Prevention recommend the use of doxycycline, ciprofloxacin, penicillin G, and amoxicillin for treatment of human cases and for post-exposure prophylaxis to anthrax spores, this study shows a high degree of in vitro susceptibility of B. anthracis to many other antimicrobials, suggesting the possibility of an alternative choice for prophylaxis and therapy.
Anthrax is a serious infectious disease, that mainly affects ruminants (farmed and wild animals) and can be transmitted to humans exposed to infected animals or infected products of animal origin (farmers, vets, butchers, carders, workers in the textile industry, etc.) [7]. The etiological agent of anthrax is Bacillus anthracis, a Gram-positive rod-shaped bacterium able to produce extremely resistant spores that, under unfavorable environmental conditions, can survive in the environment for several decades.
In particularly receptive animals (cattle, buffalo, sheep, goats, deer, and other wild ungulates), anthrax develops without apparent symptoms but has a fatal outcome characterized by sudden death due to acute or hyperacute septicemia and leakage of uncoagulated blood from natural openings.
In humans, anthrax can occur in three different forms with clinical signs dependent on the penetration route of the pathogen: cutaneous (generally non-fatal), pulmonary, and gastrointestinal [7]. Moreover, another fatal form has been described in drug users occurring after the intravenous injection of drugs contaminated with anthrax spores [2].
B. anthracis lives most of its existence in the form of a spore in soil, until ideal conditions develop allowing it to enter the reproductive cycle, which is presented mainly in domestic and wild ruminants. In animals, B. anthracis expresses its pathogenic activity primarily through the antiphagocytic activity of the capsule (whose genes are localized on the pXO2 plasmid) and the production of a toxic complex consisting of three proteins: protective antigen (PA), lethal factor (LF), and edema factor (EF) (whose genes are localized on the pXO1 plasmid) [7].
In Italy, animal anthrax is an endemic disease and most of the recorded animal outbreaks are characterized as sporadic episodes occurring usually during summer and after a rainy spring. The occurrence of new cases is generally linked to climate changes (with major incidences under warmer and extreme weather) or human activities that interfere with soil surfaces (drainage- or excavation-related work). Cases typically involve a low number of animals (one to three on average) grazing on contaminated pastures. With the exception of rare outbreaks, the disease is predominantly diffused in southern and island regions of Italy, especially in Basilicata, Apulia, and Sicily [9]. In Italy, over the last 50 years, about 200 outbreaks of animal anthrax have been recorded, while, more recently, between 2006 and 2017, 5 human cases of cutaneous anthrax occurred (unpublished data).
Furthermore, B. anthracis is considered one of the most important agents of bioterrorism. Because of its characteristics, it can be potentially misused as a biological weapon, as was confirmed by bioterrorism events in the United States in 2001 [10]. Due to the often-fatal outcome of human cases, quick administration of definitely effective antimicrobials is crucial either in prophylaxis, after presumptive exposure, or for therapy of clinical cases.
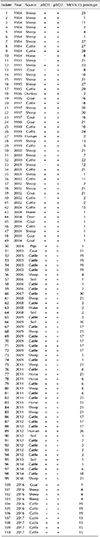
The B. anthracis strains selected for this study are members of the strain collection of the Anthrax Reference Institute of Italy (Ce.R.N.A.) located at the Istituto Zooprofilattico Sperimentale della Puglia e della Basilicata. The selected strains were isolated in Italy between 1984 and 2017 from different outbreaks and various sources: 2 strains were isolated from two different cases of human cutaneous anthrax, 102 were isolated from animals (50 from cattle, 34 from sheep, 10 from goats, 5 from horses, 1 from donkey, 1 from deer, and 1 from a pig), and 6 were isolated from environmental samples (1 from water and 5 from soils) (Table 1). In addition, 3 B. anthracis vaccine strains were included: B. anthracis Sterne 34F2 (pXO1+, pXO2−), Carbosap (pXO1+, pXO2+), and Pasteur I type (pXO1−, pXO2+).
All strains have been identified and characterized to assess the presence of plasmids pXO1 and pXO2 by polymerase chain reaction (PCR) as previously described [8]. Moreover, all strains were genotyped by 15-loci multiple-locus variable-number of tandem repeats analysis (MLVA) as reported by Van Ert et al. [13]. All work involving live B. anthracis was performed in a biosafety level 3 laboratory within a class II safety cabinet.
Antimicrobial susceptibility was determined by applying a broth microdilution method according to Clinical and Laboratory Standards Institute (CLSI) guidelines [45]. The following most-common broad-spectrum antimicrobials, all from Acros Organics (Thermo Fisher Scientific, USA), were used at the indicated concentrations: gentamicin (0.008–16 µg/mL), streptomycin (0.015–32 µg/mL), penicillin G (0.001–2 µg/mL), amoxicillin (0.008–16 µg/mL), clindamycin (0.008–16 µg/mL), chloramphenicol (0.06–128 µg/mL), vancomycin (0.06–64 µg/mL), linezolid (0.06–64 µg/mL), erythromycin (0.008–16 µg/mL), tetracycline (0.008–16 µg/mL), ciprofloxacin (0.004–8 µg/mL), doxycycline (0.004–4 µg/mL), rifampin (0.004–8 µg/mL), cefotaxime (0.25–512 µg/mL), ceftriaxone (0.25–512 µg/mL), and trimethoprim (0.125–128 µg/mL). Each molecule was dissolved in the appropriate solvent and two-fold diluted in cation-adjusted Mueller Hinton broth (CAMHB) (BD Biosciences, USA) using microplates (100 µL/well).
Overnight cultures of each B. anthracis strain were suspended in sterile saline to match a 0.5 McFarland standard using a densitometer. The cell suspensions were further diluted 1:100 in CAMHB to obtain a bacterial concentration of approximately 1–5 × 104 CFU/mL (CFU, colony-forming unit), and 100 µL bacterial aliquots were added to each well of the microplate.
Two microliters of a resazurin solution (6.75 mg/mL) (Sigma-Aldrich, USA) were added to each well to assess bacterial growth [11], and the plates were incubated overnight at 37℃. The color change caused by the resazurin was observed in the plate wells: a change from purple to pink/colorless indicated cell growth. The lowest concentration of each antibiotic that prevented bacterial growth was deemed the minimal inhibitory concentration (MIC). The use of resazurin allowed easy detection of microbial growth in extremely small solution volumes in microtiter plates; thus, there was no need for spectrophotometry of the plate samples.
The reported CLSI breakpoints (µg/mL) for B. anthracis were used for penicillin, amoxicillin, ciprofloxacin, doxycycline, and tetracycline while the breakpoints for Bacillus spp. were used for the cephem antibiotics [4]. Interpretative criteria for Staphylococcus spp. were used for gentamicin, clindamycin, chloramphenicol, vancomycin, linezolid, erythromycin, rifampin, and trimethoprim, according to CLSI guidelines [5]. As CLSI breakpoints for streptomycin were not available, it was not possible to give any comparable interpretation to the activity of this antimicrobial.
To check the validity of the antimicrobial susceptibility testing method, Staphylococcus aureus ATCC 29213 and Escherichia coli ATCC 25922 were tested in parallel as control strains.
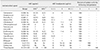
The B. anthracis pX01 plasmid was not detected by PCR in five of the examined strains, including the Pasteur I type vaccine strain, whereas the pX02 plasmid of B. anthracis was present in all examined strains except the Sterne vaccine strain (Table 1). In total, 30 different genotypes were identified by the 15-loci MLVA (Table 1), and to each genotype, an identification number was arbitrarily attributed by Ce.R.N.A. (data not shown). The concentration that inhibited the growth of 50% (MIC50) and 90% (MIC90) of the isolates, the MIC range of each antimicrobial substance tested, and the susceptibility percentages are shown in Table 2.
Antimicrobial susceptibility testing has a key role in the management of anthrax infections. In this study, a total of 110 B. anthracis strains, isolated in Italy between 1984 and 2017 were studied to determine their susceptibility to antimicrobials. The presence of virulence factors, which were evaluated by PCR, showed that all isolates, except the Sterne vaccine strain, harbored the capC gene (on plasmid pXO2). The pagA, lef, and cya genes (on plasmid pXO1 and encoding PA, LF, and EF, respectively) were not detected in five of the tested isolates. However, it appeared that the susceptibility to antimicrobials of isolates lacking plasmids was comparable to those with both pXO1 and pXO2 plasmids.
All isolates were susceptible to most of the tested antimicrobial with the exception of trimethoprim, as expected [1], for which a high level of resistance was observed, whereas for ceftriaxone and cefotaxime intermediate susceptibility levels were recorded. The results are in agreement with other previously published studies [6]. Moreover, all 30 investigated genotypes showed no difference in antimicrobial susceptibility, probably due to the high genetic homogeneity of B. anthracis.
There are few reports on the antimicrobial susceptibility profiles of B. anthracis. This can be probably explained by the rarity of human anthrax in industrialized and developed countries, where the most of the scientific research is concentrated, by the elaboration of effective control programs over the last 50 years and by efficient therapies with well-known antimicrobials such as amoxicillin, doxycycline, ciprofloxacin, and penicillin [312]. The latter are the antibiotics of first choice, as recommended by the Centers for Disease Control and Prevention, for the treatment of anthrax in human cases.
In order to be effective, an antimicrobial treatment should be timely, starting immediately after infection. Healing is possible if you intervene in the initial stages of the disease, and the late administration of antibiotics is often useless. The results in the present study suggest a high degree of in vitro susceptibility of B. anthracis to many antimicrobials. The effective activity of gentamicin, streptomycin, clindamycin, chloramphenicol, vancomycin, linezolid, tetracycline, erythromycin, and rifampin, on all tested B. anthracis strains demonstrates several appropriate alternative antimicrobials for B. anthracis prophylaxis and/or treatment. All of the tested B. anthracis strains showed intermediate susceptibility to cephems (cefotaxime and ceftriaxone) and resistance to trimethoprim. The resistance of B. anthracis to trimethoprim supports a previous report of an intrinsic resistance of B. anthracis to this compound [1].
The relationship between the indications obtainable from in vitro tests and the real clinical efficacy of an antimicrobial is obviously not absolute and depends on a complex set of factors including the effective in vivo role of the microorganism and the correct modality and timing of administration of the antimicrobial, as well as the pharmacokinetic and pharmacodynamic characteristics of the antimicrobial.
Interestingly, in this study, we demonstrated that the B. anthracis isolates, belonging to different genotypes and isolated from different sources over a long period (1984–2017) showed the same levels of susceptibility to the tested antimicrobials. Further monitoring of the antibiotic susceptibility of B. anthracis is important for the identification of resistant clones and for choosing the best therapeutic strategy when an anthrax outbreak occurs.
Figures and Tables
Acknowledgments
The authors would like to thank Michela Iatarola, Angela Aceti, Elena Poppa and Francesco Tolve for the skillful technical support. This study was funded by the Ministry of Health of Italy, Current Research 2017, project “IZSPB 03/17”, which supported the work of Istituto Zooprofilattico Sperimentale della Puglia e della Basilicata. The funders had no role in study design, data collection, and interpretation, or the decision to submit the work for publication.
References
1. Barrow EW, Bourne PC, Barrow WW. Functional cloning of Bacillus anthracis dihydrofolate reductase and confirmation of natural resistance to trimethoprim. Antimicrob Agents Chemother. 2004; 48:4643–4649.

2. Berger T, Kassirer M, Aran AA. Injectional anthrax - new presentation of an old disease. Euro Surveill. 2014; 19:20877.


3. Cavallo JD, Ramisse F, Giradet M, Vaissaire J, Mock M, Hernandez E. Antibiotic susceptibilities of 96 isolates of Bacillus anthracis isolated in France between 1994 and 2000. Antimicrob Agents Chemother. 2002; 46:2307–2309.



4. Clinical and Laboratory Standards Institute (CLSI). Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria. CLSI Guideline M45. 3rd ed. Wayne: CLSI;2016.
5. Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing. CLSI Supplement M100. 27th ed. Wayne: CLSI;2017.
6. Esel D, Doganay M, Sumerkan B. Antimicrobial susceptibilities of 40 isolates of Bacillus anthracis isolated in Turkey. Int J Antimicrob Agents. 2003; 22:70–72.


7. Fasanella A, Galante D, Garofolo G, Jones MH. Anthrax undervalued zoonosis. Vet Microbiol. 2010; 140:318–331.


8. Fasanella A, Losito S, Trotta T, Adone R, Massa S, Ciuchini F, Chiocco D. Detection of anthrax vaccine virulence factors by polymerase chain reaction. Vaccine. 2001; 19:4214–4218.


9. Fasanella A, Van Ert M, Altamura SA, Garofolo G, Buonavoglia C, Leori G, Huynh L, Zanecki S, Keim P. Molecular diversity of Bacillus anthracis in Italy. J Clin Microbiol. 2005; 43:3398–3401.



10. Hudson MJ, Beyer W, Böhm R, Fasanella A, Garofolo G, Golinski R, Goossens PL, Hahn U, Hallis B, King A, Mock M, Montecucco C, Ozin A, Tonello F, Kaufmann SH. Bacillus anthracis: balancing innocent research with dual-use potential. Int J Med Microbiol. 2008; 298:345–364.


11. Sarker SD, Nahar L, Kumarasamy Y. Microtitre plate-based antibacterial assay incorporating resazurin as an indicator of cell growth, and its application in the in vitro antibacterial screening of phytochemicals. Methods. 2007; 42:321–324.



12. Turnbull PC, Sirianni NM, LeBron CI, Samaan MN, Sutton FN, Reyes AE, Peruski LF Jr. MICs of selected antibiotics for Bacillus anthracis, Bacillus cereus, Bacillus thuringiensis, and Bacillus mycoides from a range of clinical and environmental sources as determined by the Etest. J Clin Microbiol. 2004; 42:3626–3634.



13. Van Ert MN, Easterday WR, Huynh LY, Okinaka RT, Hugh-Jones ME, Ravel J, Zanecki SR, Pearson T, Simonson TS, U'Ren JM, Kachur SM, Leadem-Dougherty RR, Rhoton SD, Zinser G, Farlow J, Coker PR, Smith KL, Wang B, Kenefic LJ, Fraser-Liggett CM, Wagner DM, Keim P. Global genetic population structure of Bacillus anthracis. PLoS One. 2007; 2:e461.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download