Abstract
Purpose
To determine the prevalence and correlates of nocturia in Korean community-dwelling older men.
Materials and Methods
A study population of 439 Korean elderly men (≥65 years of age, including 299 men from a randomly sampled population) was sampled from residents of Seongnam, Korea. Standardized face-to-face interviews and questionnaires were performed. In-person interviews solicited sociodemographic information, medical history, Mini-Mental State Examination (MMSE) score, and measurement of body mass index. Transrectal ultrasonography and laboratory tests including urinalysis and measurement of creatinine and prostate-specific antigen were performed. For the analysis of prevalence, 299 randomly sampled men were included. Men who answered the International Prostate Symptom Score questionnaire (n=424) were included in the analysis of the correlates of nocturia. Nocturia was defined as having to get up to urinate two or more times per night (≥2).
Results
The overall prevalence of nocturia was 56.0% for community-dwelling older men. There was a significant correlation between age and the prevalence of nocturia (p<0.001). The univariate analysis revealed a significant association between nocturia and MMSE score (odds ratio [OR], 0.88; p<0.001), history of benign prostatic hyperplasia (BPH) (OR, 2.85; p=0.003), alpha-blocker usage (OR, 2.79; p=0.018), alcohol consumption (OR, 0.65; p=0.035), and smoking (OR, 0.58; p=0.025). Age, duration of education, MMSE score, and prostate volume were also significantly associated with nocturia. In the multivariate regression analysis using forward elimination, nocturia was significantly associated with a history of BPH and MMSE score.
Night-time voiding is a common urological problem. Nocturia is defined as waking up at night two or more times (≥2) to void [1]. It is more common among women at a younger age. In older age groups, however, it is equally or more common among men [2,3]. The frequency of nocturnal voiding increases with age for both genders [4]. Although it is underreported and rarely recognized as a problem [5], up to 60% of older men void two or more times per night [4]. Moreover, it is usually bothersome and affects quality of life (QoL).
Nocturia has an adverse effect on sleep, and it increases the risk of fracture and mortality [6,7]. Although the literature is inconsistent, previous studies have reported that cardiac disease, hypertension, depression, diuretics usage, urinary incontinence, obesity, and race are correlated with nocturia [8-15], which reflects the multifactorial etiology of nocturia.
Several studies on nocturia have been conducted in Korea [16,17]. Choo et al. [16] reported a 48.2% prevalence of nocturia in 2005 Korean subjects (1,005 females and 1,000 males) aged 40 to 89 years by telephone survey. The mean and median age of the male respondents was 59.7±11.5 years and 60.0 years, respectively. Considering the fact that the incidence of nocturia increases with age [3] and that it is also associated with increased mortality [7], it is important to investigate the prevalence and correlates of nocturia in the older age group. This article is the first population-based study in Korea to examine the prevalence of nocturia in an aged population (≥65 years of age). The aim of the present study was to estimate the prevalence of nocturia in community-dwelling older men and to identify the correlates of nocturia.
The current study was conducted as a part of the Korean Longitudinal Study on Health and Aging (KLoSHA), which was a population-based prospective cohort study on health, aging, and common geriatric diseases in elderly Koreans [18]. The baseline study was conducted from September 2005 to August 2006, and follow-up studies will be continued at 5-year intervals.
The baseline cohort of the KLoSHA consisted of two samples: a simple random sample (n=1,118) drawn from a pool of 61,730 persons aged 65 years or older living in Seongnam city on Aug 1, 2005, and a volunteer sample (n=3,166) that included all residents aged 85 years or older living in Seongnam city on Aug 1, 2005. The residents were invited to participate in the study by both letter and telephone. Of the 1,118 randomly sampled individuals, 299 men and 415 women agreed to participate in the baseline KLoSHA study. Of the 3,166 very old residents (≥85 years of age), 137 men and 141 women volunteered to participate in the baseline KLoSHA study. We used 299 randomly sampled male respondents to investigate the prevalence of nocturia. For the correlates of nocturia, 439 male participants who answered the International Prostate Symptom Score (IPSS) questionnaire, which included 299 randomly sampled respondents, were analyzed.
To assess nocturnal voids, we defined nocturia as two or more nightly voids. Information about nocturia was collected by using the Korean version of question 7 of the IPSS questionnaire ("How many times do you usually wake up at night to urinate?"). The response alternatives on a 0 to 5 scale were none (0), once (1), twice (2), three times (3), four times (4), and five or more times (5). The prevalence of nocturia was estimated from the random sample of 293 subjects, excluding 6 nonresponders, and the factors associated with nocturia were identified from the whole sample (n=424, excluding 15 nonresponders). At each participant's first visit, demographics and general health status were evaluated by using standardized self-questionnaires and interviews by three dementia-specialized nurses. Within 2 weeks of the first visit, participants arrived for a second visit, in which comprehensive neuropsychological tests were conducted by four neuropsychiatric specialists. Additionally, transrectal ultrasonography was performed for men, and laboratory tests including urinalysis, creatinine, and prostate-specific antigen (PSA) were conducted to evaluate the participants' general physical health status and the presence of common geriatric disorders.
Informed consent was provided by each participant or a legal guardian before participating in the study. The study protocol was approved by the institutional review board of Seoul National University Bundang Hospital. The recommendations of the Declaration of Helsinki for biomedical research involving human subjects were followed.
The prevalence of nocturia was calculated and stratified by age (65-69, 70-74, 75-79, and ≥80 years of age) in the randomly sampled respondents. For the analysis of correlates, nocturia was defined as a dichotomous variable with participants who reported waking up to urinate once per night or not at all coded as 0 and twice or more coded as 1. Odds ratios for each variable were calculated from univariate models including no covariate adjustments and from multivariable models adjusted for the effects of age. Based on the result of the univariate analysis, logistic regression analysis using forward elimination with p<0.2 was used for the multivariate analysis with a value of p<0.05. SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analyses.
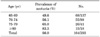
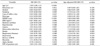
The prevalence of nocturia in Seongnam city, Korea, is summarized in Table 1. The overall prevalence of nocturia was 56.0%. The incidence of nocturia increased significantly with age (p<0.001). In a randomly sampled population, most of the participants were <75 years of age. The characteristics of the participants are shown in Table 2. The mean age of the 299 randomly sampled respondents was 71.23±5.02 years. Of these, 261 had a spouse.
Participants with nocturia tended to be older, be less educated, drink less coffee, have a lower IPSS-QoL score, have a lower MMSE score, have a higher PSA, and have a larger prostate. Although the number was small and was insignificant, people taking diuretics were more common in the nocturia group (p=0.180). There were no statistically significant differences between the nocturia and non-nocturia group except for depression and history of benign prostatic hyperplasia (BPH). Past and current medical history such as diabetes mellitus, hypertension, angina, myocardial infarction, stroke, asthma, pneumonia, tuberculosis, and other respiratory diseases were included in the analysis but did not show any statistically significant differences between the nocturia and non-nocturia group.
Data from the univariate analysis for the correlates of nocturia are presented in Table 3. Nocturia was significantly associated with age. After adjustment for age, the results from the univariate analysis revealed that a lower MMSE score, a history of BPH, alpha-blocker usage, and transitional zone volume of the prostate were significantly associated with nocturia. The multivariate logistic regression analysis using the forward elimination method revealed that nocturia was associated with a history of BPH and a lower MMSE score (Table 4).
Several studies regarding the prevalence of nocturia have been conducted in Europe and America. In Korea, however, few community-based studies have been conducted, and most of those were composed of young people. This is the first community-based study of nocturia in an aged population in Korea. For the analysis of correlates, 424 elderly men were studied, and about one third of them were ≥80 years of age. This study is meaningful because of the high prevalence of nocturia in the aged population.
The current study demonstrated a high prevalence of nocturia in community-dwelling older Korean men, indicating the need for proper assessment of nocturia in aged populations. The overall prevalence of nocturia was 56.0%, which is concordant with other previously reported studies [4].
In Korea, one study that utilized a telephone survey reported that about 60% of men aged 70 to 79 years and about 80% of men aged 80 to 89 years routinely had two or more nocturnal voiding episodes [16]. In this study, we used a randomly sampled population only for the analysis of prevalence. If we had included all the other participants, mostly representing participants in their 80s or 90s, the prevalence would have been much higher than this result. Volunteers composed of mostly participants aged 80 or older revealed a slightly higher but similar incidence of nocturia as presented in our results.
In previous studies, nocturia was shown to be correlated with age [2,4,16,19,20]. This was also evident in the present study. According to the population-based Finnish National Nocturia and Overactive Bladder (FINNO) study, urgency and snoring (both sexes), BPH (men only), and being overweight (women only) accounted for the largest proportion of individuals with nocturia [15]. However, none of the correlates affected 50% or more of men with nocturia, which thus reflects the multifactorial etiology of nocturia. In the present study, a history of BPH was associated with nocturia in the multivariate analysis. In comparison with the FINNO study, which revealed associations of prostate cancer, antidepressant usage, restless legs syndrome, and obesity with nocturia in men at the population level, the present study revealed that none of the modifiable medical conditions, such as diabetes mellitus, hypertension, and coronary heart disease, was associated with nocturia. Unlike the previous studies reporting an association of obesity and higher body mass index (BMI) with nocturia [12], BMI was not associated with nocturia in this analysis, partly because of the lower incidence of high BMI in the study population. More than 60% of the participants had a BMI less than 25 kg/m2 in both the nocturia and the non-nocturia groups.
The MMSE score is a brief 30-point questionnaire that is used to screen for cognitive impairment in general and dementia in particular. Any score ≥25 points out of 30 is normal. The MMSE score is affected by educational attainment and age [21]. A previous study reported a correlation between nocturia and MMSE score, with a higher MMSE score being protective [19]. In our study, persons who had nocturia appeared to have a lower MMSE score (OR, 0.64, 95% confidence interval, 0.46-0.88, p=0.006). The mean MMSE score was 24.36±4.005 in the nocturia group and 25.93±3.388 in the non-nocturia group. Individuals with nocturia tended to be older and less educated, which might have affected the MMSE score.
Nowadays, it is recommended that a flow-volume chart be used as a key diagnostic tool to assess the exact status of nocturia [4], because self-reported questionnaires might not reflect the exact frequency of nocturnal voiding [22]. We used question 7 on the IPSS questionnaire. This was partly because this study was part of a large population-based surveillance study and the participants were not patients by definition. Thus, we could not get a voiding diary from every participant. However, in the course of in-person interviews, we explained thoroughly to the participants the contents of the questionnaires to minimize bias; thus, the present data could well be an accurate report of nocturia. In addition, many previous studies have used questionnaires to assess nocturia [2,15,19,23].
The limitations of this study are the relatively small number of subjects (424) and the lack of a flow-volume chart in the assessment. Nocturnal polyuria other than BPH or overactive bladder is one of major causes of nocturia. With the lack of a flow-volume chart, we could not discriminate nocturnal polyuria from other causes of nocturia.
Despite those limitations, the results of this study enrich the literature on nocturia in Korea. Study strengths include its community-based design within Korean elders and the rigorous evaluation of participants thorough in-person interviews, which solicited information concerning past and current medical history, including medications, laboratory tests, and transrectal ultrasonography of the prostate, for all participants. Also, for the analysis of correlates, there was an almost even distribution in the study population of those aged 65 to 69, 70 to 79, and ≥80 years.
Figures and Tables
ACKNOWLEDGEMENTS
This work was supported by an Independent Research Grant (IRG) from Pfizer Global Pharmaceuticals (Grant No. 06-05-039) and by a grant of the Korean Health Technology R&D Project, Ministry for Health, Welfare, & Family Affairs, Republic of Korea (Grant No. A092077).
References
1. van Kerrebroeck P, Abrams P, Chaikin D, Donovan J, Fonda D, Jackson S, et al. The standardisation of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002. 21:179–183.
2. Tikkinen KA, Tammela TL, Huhtala H, Auvinen A. Is nocturia equally common among men and women? A population based study in Finland. J Urol. 2006. 175:596–600.
3. Bing MH, Moller LA, Jennum P, Mortensen S, Skovgaard LT, Lose G. Prevalence and bother of nocturia, and causes of sleep interruption in a Danish population of men and women aged 60-80 years. BJU Int. 2006. 98:599–604.
4. Bosch JL, Weiss JP. The prevalence and causes of nocturia. J Urol. 2010. 184:440–446.
5. Chen FY, Dai YT, Liu CK, Yu HJ, Liu CY, Chen TH. Perception of nocturia and medical consulting behavior among community-dwelling women. Int Urogynecol J Pelvic Floor Dysfunct. 2007. 18:431–436.
6. Kupelian V, Fitzgerald MP, Kaplan SA, Norgaard JP, Chiu GR, Rosen RC. Association of nocturia and mortality: results from the Third National Health and Nutrition Examination Survey. J Urol. 2011. 185:571–577.
7. Nakagawa H, Niu K, Hozawa A, Ikeda Y, Kaiho Y, Ohmori-Matsuda K, et al. Impact of nocturia on bone fracture and mortality in older individuals: a Japanese longitudinal cohort study. J Urol. 2010. 184:1413–1418.
8. Fitzgerald MP, Litman HJ, Link CL, McKinlay JB;. The association of nocturia with cardiac disease, diabetes, body mass index, age and diuretic use: results from the BACH survey. J Urol. 2007. 177:1385–1389.
9. Johnson TM 2nd, Sattin RW, Parmelee P, Fultz NH, Ouslander JG. Evaluating potentially modifiable risk factors for prevalent and incident nocturia in older adults. J Am Geriatr Soc. 2005. 53:1011–1016.
10. Johnson TV, Abbasi A, Ehrlich SS, Kleris RS, Raison CL, Master VA. Nocturia associated with depressive symptoms. Urology. 2011. 77:183–186.
11. Kupelian V, Rosen RC, Link CL, McVary KT, Aiyer LP, Mollon P, et al. Association of urological symptoms and chronic illness in men and women: contributions of symptom severity and duration: results from the BACH Survey. J Urol. 2009. 181:694–700.
12. Tikkinen KA, Auvinen A, Huhtala H, Tammela TL. Nocturia and obesity: a population-based study in Finland. Am J Epidemiol. 2006. 163:1003–1011.
13. Asplund R. Obesity in elderly people with nocturia: cause or consequence? Can J Urol. 2007. 14:3424–3428.
14. Häkkinen JT, Shiri R, Koskimäki J, Tammela TL, Auvinen A, Hakama M. Depressive symptoms increase the incidence of nocturia: Tampere Aging Male Urologic Study (TAMUS). J Urol. 2008. 179:1897–1901.
15. Tikkinen KA, Auvinen A, Johnson TM 2nd, Weiss JP, Kern A, Hakama M. A systematic evaluation of factors associated with nocturia: the population-based FINNO study. Am J Epidemiol. 2009. 170:361–368.
16. Choo MS, Ku JH, Park CH, Lee YS, Lee KS, Lee JG, et al. Prevalence of nocturia in a Korean population aged 40 to 89 years. Neurourol Urodyn. 2008. 27:60–64.
17. Lee YS, Lee KS, Jung JH, Han DH, Oh SJ, Seo JT, et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol. 2011. 29:185–190.
18. Park JH, Lim S, Lim JY, Kim KI, Han MK, Yoon IY, et al. An overview of the Korean Longitudinal Study on Health and Aging. Psychiatry Investig. 2007. 4:84–95.
19. Burgio KL, Johnson TM 2nd, Goode PS, Markland AD, Richter HE, Roth DL, et al. Prevalence and correlates of nocturia in community-dwelling older adults. J Am Geriatr Soc. 2010. 58:861–866.
20. Bing MH, Moller LA, Jennum P, Mortensen S, Lose G. Pathophysiological aspects of nocturia in a danish population of men and women age 60 to 80 years. J Urol. 2007. 178:552–557.
21. Crum RM, Anthony JC, Bassett SS, Folstein MF. Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA. 1993. 269:2386–2391.
22. Blanker MH, Bohnen AM, Groeneveld FP, Bernsen RM, Prins A, Ruud Bosch JL. Normal voiding patterns and determinants of increased diurnal and nocturnal voiding frequency in elderly men. J Urol. 2000. 164:1201–1205.
23. Häkkinen JT, Hakama M, Shiri R, Auvinen A, Tammela TL, Koskimäki J. Incidence of nocturia in 50 to 80-year-old Finnish men. J Urol. 2006. 176(6 Pt 1):2541–2545.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download