Abstract
Chronic hyperglycemia is the primary risk factor for the development of complications in diabetes mellitus (DM); however, it is believed that frequent or large glucose fluctuations may independently contribute to diabetes-related complications. Postprandial spikes in blood glucose, as well as hypoglycemic events, are blamed for increased cardiovascular events in DM. Glycemic variability (GV) includes both of these events; hence, minimizing GV can prevent future cardiovascular events. Correcting GV emerges as a target to be pursued in clinical practice to safely reduce the mean blood glucose and to determine its direct effects on vascular complications in diabetes. Modern diabetes management modalities, including glucagon-related peptide-1-based therapy, newer insulins, modern insulin pumps and bariatric surgery, significantly reduce GV. However, defining GV remains a challenge primarily due to the difficulty of measuring it and the lack of consensus regarding the optimal approach for its management. The purpose of this manuscript was not only to review the most recent evidence on GV but also to help readers better understand the available measurement options and how the various definitions relate differently to the development of diabetic complications.
Glycemic variability (GV), which refers to swings in blood glucose levels, has a broader meaning because it alludes to blood glucose oscillations that occur throughout the day, including hypoglycemic periods and postprandial increases, as well as blood glucose fluctuations that occur at the same time on different days. The broad definition of GV considers the intraday glycemic excursions, including episodes of hyperglycemia and hypoglycemia.
The concept of variability is often used in a negative sense when referring to human pathology. However, variability plays a fundamental role in all of the primary control systems in our body. The circadian rhythm of the hormones involved in glucose metabolism has been related to variations in glucose tolerance and insulin action [1]. Therefore, GV is not always negative because changes in glycemia are the physiological consequence not only of the circadian rhythm of hormones involved in the control of glucose metabolism, but also of carbohydrate intake. Although a certain degree of variability is also observed in subjects with normal glucose tolerance [2], GV is increased in people with diabetes and in people with impaired blood glucose regulation. Therefore, it is crucial not only to identify the boundary beyond which GV takes on a pathological meaning but also, more importantly, to better define the concept of GV. However, the literature on glucose GV is extensive yet inconsistent, especially regarding cardiovascular (CV) mortality [3456]. In this review, we will discuss the most recent reports, clinical implications, and measures for controlling GV in clinical practice.
According to various studies, the occurrence of various microvascular and macrovascular complications in diabetes is attributed to hyperglycemia and dysglycemia (peaks and nadirs). Several pathophysiological mechanisms were reported, unifying the two primary mechanisms: excessive protein glycation end products and activation of oxidative stress, which causes vascular complications. Intermittent high blood glucose exposure, rather than constant exposure to high blood glucose, has been shown to have deleterious effects in experimental studies [78]. In vitro and in vivo data have presented the mechanisms that are at the basis of the adverse CV effects of GV, which are mainly associated with oxidative stress; the atherogenic action of postprandial glucose (PPG) also involves insulin sensitivity, the postprandial increase of serum lipids and the glycemic index of food [9]. In In vitro experimental settings and in animal studies, glycemic fluctuations display a more deleterious effect on the parameters of CV risk, such as endothelial dysfunction [10]. There is a significant association between GV and the increased incidence of hypoglycemia [11]. Hypoglycemic events may trigger inflammation by inducing the release of inflammatory cytokines. Hypoglycemia also induces increased platelet and neutrophil activation. The sympathoadrenal response during hypoglycemia increases adrenaline secretion and may induce arrhythmias and increase the cardiac workload. Underlying endothelial dysfunction leading to decreased vasodilation may contribute to CV risk [12]. Published studies have demonstrated that GV, particularly when associated with severe hypoglycemia, could be harmful not only to people with diabetes but also to nondiabetic patients in critical care settings [17]. Overall, the pathophysiological evidence appears to be highly suggestive of GV being an important key determinant of vascular damage [13].
Extensive clinical trials have confirmed the association between hyperglycemia and the development of long-term complications in type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) [9]. The majority of these studies have used time-averaged glucose values measured as glycosylated hemoglobin (HbA1c), an indicator of the degree of glycemic control, which is why HbA1c has become the reference parameter for therapies aimed at reducing the risk of complications from diabetes. Chronic hyperglycemia is almost universally assessed by HbA1c, which in a longitudinal study by Nathan et al. [14] has been shown to correlate closely with mean glucose levels over time, as determined by continuous glucose monitoring (CGM). However, the relative contribution of postprandial glycemic excursions and fasting to overall hyperglycemia has been the subject of considerable debate. Monnier et al. [15] suggested that the relative contributions of fasting and postprandial glucose differ according to the level of overall glycemic control. Fasting glucose concentrations present the most important contribution to hemoglobin glycosylation, whereas at lower levels of HbA1c, the relative contribution of postprandial hyperglycemia becomes predominant [1516]. Collectively, GV is likely to be incompletely expressed by HbA1c, particularly in patients with good metabolic control as shown in Fig. 1.
The studies identified here illustrate that a large number of different methods are currently used to assess GV (Table 1). Currently, a clear consensus on the gold-standard method for measuring GV in clinical practice and research is lacking, although numerous indicators have been proposed [1]. On the contrary, an excessive amount of variability indices could lead to an increase of the existing confusion surrounding this important issue. Several of these indices can now be obtained by downloading self-monitoring blood glucose (SMBG) data, thereby making them available not only to diabetologists but also to patients. However, other indices are particularly complex, even when determined using the most innovative blood glucose monitoring systems, such as CGM. The majority of studies that have examined the degree of correlation between different assessment methods demonstrated that the most widely used methods are closely correlated among themselves and with previously developed measures [17]. Additionally, GV mandates restriction to a description of glucose excursions exclusive of a time component. Glycemic exposure (glucose excursion×time) and slope (glucose excursion/time) are indicators of the rate of glucose change but not its extent [18]. More details on the methodology for each of the indicators are described in a 2013 review by Service [18]. Rather than comment on all of the indicators, we would like to discuss a few salient points regarding the most commonly used measures. Although standard deviation (SD) is widely used, it has a limitation in that its use implies that glucose measures are normally distributed, which is typically not the case. However, SD remains a fairly robust measure because a linear relation has been established between the interquartile range and the SD [19]. The mean amplitude of glucose excursion (MAGE) was designed to capture mealtime-related glucose excursions. To separate mealtime-induction from other glucose excursions, investigations conducted in healthy volunteers found that excursions larger than 1.0 SD of the glucose measurements obtained were consistently related to mealtime. Detailed calculation of MAGE is depicted in Fig. 2. MAGE has also been criticized on five points [20]. First, with the introduction of CGM, postprandial excursions can be assessed more precisely by using the area under the curve and the trapezoidal method. Second, the calculation of MAGE is operator-dependent and not unambiguously defined. Third, the outcome differs depending on whether ascending or descending limbs are used for calculating MAGE. Fourth, there is a high correlation with the SD. Fifth, it is questionable whether only mealtime excursions or excursions larger than 1.0 SD would have clinical importance. The methods used for evaluating GV represent a critical issue because all of the methods suffer from the fact that GV is significantly influenced by the mean blood glucose: higher mean blood glucose levels are associated with higher GV values, unless they are corrected for the mean blood glucose. Correcting for the mean glucose of any relation between GV and a given outcome is important because high correlations between GV and the mean glucose have been demonstrated [20]. Because many studies have not made this correction, the reliability of their results could be questionable. For reasons outlined in this counterpoint, the coefficient of variation (CoV) has been proposed as the preferred measure of GV [2021]. The CoV in CGM was significantly associated with the presence of CV autonomic neuropathy in patients with inadequately controlled T2DM [22]. Jin et al. [23] identified independent factors associated with measures of GV. Fasting C-peptide levels inversely correlated with CoV in T1DM and insulin-treated T2DM. In T2DM without insulin therapy, high density lipoprotein and low density lipoprotein levels and the use of sulfonylurea were significantly correlated with the CoV [23].
SMBG revolutionized the management of diabetes, becoming an integral part of the standard diabetes treatment in daily practice and recommended in the guidelines for managing therapy [24]. Frequent blood glucose monitoring is essential for managing the therapy of insulin-treated diabetes and in reducing HbA1c and the risk of hypoglycemia [25]. However, it should be noted that SMBG may not be appropriate for assessing GV because of the high number of determinations (at least hourly) that are needed to evaluate the parameters, such as SD, MAGE, and continuous overall net glycemic action (CONGA) [26]. Another major limitation of the methods for measuring GV associated with SMBG-based measures is that they provide an unsophisticated measure of variability, with a significant dependence on patient cooperation that makes the planning of long-term studies difficult. This observation casts doubt on the significance of the lack of correlation between GV and complications when GV is assessed with 7-point blood glucose profiles [11]. CGM, which is a new frontier for the overall assessment of GV, has revolutionized the management of patients with T1DM and has allowed for better troubleshooting in several patients with T2DM [2728]. CGM can provide information on daily glucose fluctuations and can show how those numbers are affected by everyday activities and stress levels. For this reason, clinical studies on CGM use may be easily performed to provide valuable data with minimal inconvenience to patients. CGM is particularly useful in clinical practice for various conditions as shown in Table 2. A meta-analysis suggests that, compared with SMBG, CGM is associated with a short-term reduction of HbA1c of 0.26% [29]. However, the long-term effectiveness of CGM needs to be determined. It also plays an integral part in emerging technology billed as an "artificial pancreas" partnering with continuous sensing technology to form a closed-loop glycemic control system that includes an insulin pump and controlling algorithms.
For routine clinical practice, it is likely that the SD and corresponding CoV obtained using either SMBG or CGM will be sufficient to permit the assessment of changes in GV with time or following therapeutic interventions, and to permit comparisons with reference populations of patients with a similar type, duration, and level of control of HbA1c or mean glucose [2127]. Despite the various formulas offered, simple and standard clinical tools for defining GV have yet to evolve and different indexes of GV should be used, depending on the metabolic profile of the studied population.
In addition to the indices mentioned, simple markers of glycemia, such as glycated albumin (GA) and 1,5-anhydroglucitol (1,5-AG), may have clinical utility for diagnosing and evaluating GV and predicting diabetic complications [3031]. We have already shown that these glycemic markers are significantly correlated with all of the GV parameters from CGM [16]. GA was demonstrated to be a more useful glycation index than HbA1c for monitoring short-term glycemic control in patients with T2DM [32], especially those with fluctuating and poorly controlled glycemic conditions [33]. Additionally, a high GA/HbA1c ratio reflects higher glycemic excursions, irrespective of the type of diabetes [34]. The 1,5-AG level is also reflective of the short-term glucose status, postprandial hyperglycemia, and GV that is not captured using HbA1c assay in patients with T1DM and T2DM [3536]. Simultaneous measurements of GA, 1,5-AG, and HbA1c may help to identify a group of patients who warrant closer monitoring in relation to GV.
There is considerable clinical evidence that supports the negative role of GV in the development of diabetes complications. The role of GV in the development of microvascular complications was initially suggested by the analysis of the diabetes control and complications trial (DCCT) data [37], which showed that increased HbA1c explained only 11% of the variation in the risk of retinopathy, meaning that factors independent of HbA1c must presumably explain the remaining 89%. In recent years, GV has been proposed to be an additional risk factor for complications of diabetes independent of hyperglycemia [3839]. Growing evidence indicates that significant GV, particularly when accompanied by hypoglycemia, can have a harmful effect not only on the onset and progression of diabetes complications but also in clinical conditions other than diabetes treated in intensive care units (ICUs) [20]. Regarding GV, it is important to note the differences among patients with T1DM, patients with insulin-treated T2DM and patients with T2DM using dietary therapy or oral hypoglycemic agents [24]. GV is always important in T1DM, where alternating hyperglycemia, normoglycemia and hypoglycemia are linked to an absolute insulin deficiency, erratic absorption of exogenous insulin, incomplete suppression of hepatic glucose production and altered hormonal counterregulation, among other factors. Recent studies using CGM showed a significant fluctuation in the blood glucose values of children with T1DM, as well as in those with excellent HbA1c values. This finding suggests that in addition to HbA1c, GV may have a predictive value for the development of T1DM complications [40]. A recent study identified the important association between GV and diabetes-related quality of life and treatment satisfaction in patients with T1DM [41].
In insulin-treated T2DM, the relevance of GV varies according to the heterogeneity of the disease, the presence of residual insulin secretion and insulin resistance, in addition to the factors mentioned above. The findings from studies on T2DM support the likelihood that increased levels of short-term GV may play a substantial role in the development of microvascular complications [20]. Hsu et al. [42] showed a significant association of GV with diabetes retinopathy in patients with T1DM and T2DM. Jin et al. [43] found a significant association between urinary albumin excretion and GV measured by CGM. Less clear is the relationship between GV and CV events and overall mortality [11]. Several years ago, Muggeo et al. [44] found that all-cause and CV mortality in elderly people with T2DM was primarily associated with the variability/instability of fasting glucose levels, rather than its absolute values. The second clue in favor of this hypothesis is based primarily on the observation that in individuals with diabetes and in those with impaired glucose tolerance (IGT), blood glucose two hours after oral glucose loading has a higher predictive value for CV events than fasting plasma glucose (FPG) [45]. A third supporting element is based on the consideration that an increase in postprandial glycemia may have a particularly harmful effect on the onset of CV complications, a concept supported by the study to prevent non-insulin-dependent diabetes mellitus (study to prevent non-insulin-dependent diabetes mellitus [STOP-NIDDM]) [46], but not by a study of hyperglycemia and its effect after acute myocardial infarction on CV outcomes in patients with T2DM (hyperglycemia and its effect after acute myocardial infarction on cardiovascular outcomes in patients with type 2 diabetes mellitus [HEART2D]) [3], which has led to a heated debate. Another supporting factor is based on the fact that the presence of acute hyperglycemia during acute myocardial infarction [47] or in intensive care patients [48] is associated with worse prognosis in individuals with diabetes or without diabetes. Therefore, PPG is not only a key determinant of HbA1c but also an independent parameter in the risk stratification of CV events and total mortality [4]. Since 1997, more than 15 observational studies have been published showing that elevated PPG, even in the high nondiabetic IGT range, contributes to an approximately 3-fold increase in the risk of developing coronary heart disease or a CV event [13]. Moreover, the meta-analysis of the published data from 20 studies of 95,783 individuals found a progressive relationship between the GV and CV risk [49]. In summary, the accumulated data that GV seems to be associated with the development of microvascular complications appear to be impressive. However, the evidence is less convincing in terms of a unique role for the long-term prediction of macrovascular complications above and beyond other glycemic parameters, such as FPG and HbA1c. Nevertheless, we should still include GV in the list of potential risk factors for diabetes complications.
The hypothesis that the maintenance of close glycemic control is of importance in all of the clinical settings is highlighted by the recent evidence that in individuals with normal glucose tolerance, glycemia is maintained within a narrow range between 68.4 and 138.6 mg/dL [50]. Translated into clinical terms, this suggests that maintaining a normal glycemic level is important not only in diabetes but also in clinical contexts in which glycemia tends to increase. However, caution is required in treatment, particularly with insulin, to avoid excessive fluctuations and the risk of hypoglycemia, especially in ICUs. It is advisable to make every effort to maintain stable glycemic values, even above strictly physiological levels.
Severe hypoglycemia is strongly associated with the increased risks of a range of adverse clinical outcomes in patient with diabetes [51]. In the DCCT trial, a 10% to 30% incidence of hypoglycemia was observed in the intensive insulin arm group. Hypoglycemia was the primary accompanying complication when the desired glucose target was intensively achieved. The frequency of severe hypoglycemia increases exponentially when lowering blood glucose [52] and several studies have reported that low GV coincided with decreased occurrence of hypoglycemia [53]. HbA1c is a poor predictor of hypoglycemic episodes because it only considers 8% of the likelihood of severe hypoglycemia [54]; on the contrary, GV can account for an estimated 40% to 50% of future hypoglycemic episodes. In a study by Kilpatrick et al. [55] using datasets of the DCCT, GV was independently predictive of hypoglycemia, similar to the mean blood glucose. They also showed that HbA1c is a poor predictor of hypoglycemic risk, whereas GV is a strong predictor of hypoglycemic episodes. Kim et al. [56] found that Korean T1DM patients with hypoglycemic events had a significantly higher GV index, as calculated from the CGM data. Collectively, patients at risk for hypoglycemia (i.e., those receiving insulin or insulin secretagogues) constitute one category that requires GV monitoring.
The primary purpose of diabetes treatment is to obtain the most optimal metabolic control to avoid metabolic imbalance related to diabetes itself and the onset of complications. Of the various parameters required to evaluate the therapeutic efficacy of a given agent, in addition to the parameters that are most frequently used, such as fasting glycemia, postprandial glycemia and HbA1c, the options include GV. The target GV has been a topic of debate. Monnier and Colette [57] proposed that a MAGE value of 40 mg/dL as the target level of GV and found that GV was an independent predictor of chronic diabetic complications, in addition to HbA1c. An independent association exists between increased GV and higher mortality in ICU patients [58]. In nondiabetic critically ill patients, diminishing hyperglycemic excursions will improve mortality [7]. As in recent studies, for example, the action to control cardiovascular risk in diabetes (ACCORD) study, hypoglycemia must be avoided. The study of Brunner et al. [59] showed that strict glycemic control using CGM did not decrease GV. Therefore, it is difficult, if not impossible, to decrease GV. The importance of GV and PPG has also been demonstrated in the results of intervention studies [60]. It appears indisputable that PPG excursions play an important role in determining the overall metabolic control in diabetes mellitus because an increase in PPG has a greater prognostic significance in terms of GV [61]. Thus, trials specifically aimed at correcting GV have not been conducted; however, trials that tended to correct PPG, at least in theory, have been conducted (i.e., STOP-NIDDM, HEART2D, nateglinide and valsartan in impaired glucose tolerance outcomes research [NAVIGATOR]) and are ongoing (acarbose cardiovascular evaluation [ACE]). If all of the intervention studies are taken together, there is no definite proof that targeting postprandial hyperglycemia results in a more beneficial outcome of CV complications in subjects with IGT or overt T2DM [13]. However, we should note that PPG and GV are not identical, even if they are closely related. Moreover, the absence of a uniformly accepted standard of how to estimate postprandial hyperglycemia and GV adds another challenge to this debate. Additional studies are warranted for confirming or refuting the role of GV as a treatment target.
The attention dedicated to GV is derived from the above evidence concerning its effects on oxidative stress and, from the latter, on chronic diabetes complications. Control of GV has been the focus of a number of interventional studies aimed at reducing this fluctuation. Diet and weight reduction are the first therapeutic instrument that can be used for reducing GV. Glucagon-like peptide-1 analogs and dipeptidyl-peptidase 4 inhibitors demonstrated a significant impact on GV in people with T2DM [17]. Regarding insulin therapy, the evolution of fast-acting and long-acting insulin has had a positive impact on the control of GV. One of the aims of the ultraslow analog degludec, which was recently approved for clinical use, is to reduce GV by virtue of its smaller pharmacodynamic variability. To date, the published results show that degludec is capable of reducing the frequency of episodes of hypoglycemia in patients with T1DM and postprandial glycemia oscillations in patients with T2DM, suggesting potential efficacy in the control of GV [62]. Continuous Subcutaneous Insulin Infusion (CSII) and bariatric surgery were also associated with significant reductions in hyperglycemic excursions along with the mean glucose [763]. Lastly, the development of new technologies for diabetes education, monitoring and therapy, particularly in T1DM, has made it possible to identify GV as an emerging target for improving overall diabetes treatment [1]. There should be no doubt that pharmacological advances directed at the ultimate goal of physiological insulin replacement will continue to the point where the postprandial glycemic curve will be bent to conform to that of nondiabetic subjects. In that ideal situation, the currently available measures of GV can be retired.
GV is a physiological phenomenon that assumes an even more important dimension in the presence of diabetes because it not only contributes to increasing the mean blood glucose values but it also favors the development of chronic diabetes complications. It appears that GV is poised to become a future target parameter for optimum glycemic control over and above standard glycemic parameters, such as blood glucose and HbA1c. Avoiding both hyperglycemia and hypoglycemia by careful use of SMBG and the availability of new agents to correct hyperglycemia without inducing hypoglycemia is expected to reduce the burden of premature mortality and disabling CV events associated with diabetes mellitus. However, defining GV remains a challenge primarily due to the difficulty of measuring it and the lack of consensus regarding the most optimal approach for patient management.
Figures and Tables
Fig. 1
Glycemic variability in three hypothetical patients who have the same mean blood glucose concentration. Patient B has relatively small variations during the day and on different days; this patient should have little difficulty in lowering daily mean blood glucose concentrations without inducing hypoglycemia. In comparison, patient A has marked blood glucose variations on the same day and patient C has marked blood glucose variations on different days.
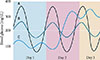
Fig. 2
Calculation of mean amplitude of glucose excursion (MAGE). In the first step, all the local maximum/minimum values are determined. The next step is an assessment of maximum/minimum pairs against the standard deviation (SD). If the difference from minimum to maximum is greater than the SD, this variation from mean measure is retained. If the local maximum/minimum is less than 1 SD it is excluded from further calculations. These troughs are retained and summed to achieve the MAGE.

Table 1
Glycemic variability indices

Table 2
Indications for continuous glucose monitoring

References
1. Frontoni S, Di Bartolo P, Avogaro A, Bosi E, Paolisso G, Ceriello A. Glucose variability: an emerging target for the treatment of diabetes mellitus. Diabetes Res Clin Pract. 2013; 102:86–95.
2. Wang C, Lv L, Yang Y, Chen D, Liu G, Chen L, Song Y, He L, Li X, Tian H, Jia W, Ran X. Glucose fluctuations in subjects with normal glucose tolerance, impaired glucose regulation and newly diagnosed type 2 diabetes mellitus. Clin Endocrinol (Oxf). 2012; 76:810–815.
3. Siegelaar SE, Kerr L, Jacober SJ, Devries JH. A decrease in glucose variability does not reduce cardiovascular event rates in type 2 diabetic patients after acute myocardial infarction: a reanalysis of the HEART2D study. Diabetes Care. 2011; 34:855–857.
4. Cavalot F, Petrelli A, Traversa M, Bonomo K, Fiora E, Conti M, Anfossi G, Costa G, Trovati M. Postprandial blood glucose is a stronger predictor of cardiovascular events than fasting blood glucose in type 2 diabetes mellitus, particularly in women: lessons from the San Luigi Gonzaga Diabetes Study. J Clin Endocrinol Metab. 2006; 91:813–819.
5. Muggeo M, Zoppini G, Bonora E, Brun E, Bonadonna RC, Moghetti P, Verlato G. Fasting plasma glucose variability predicts 10-year survival of type 2 diabetic patients: the Verona Diabetes Study. Diabetes Care. 2000; 23:45–50.
6. Nalysnyk L, Hernandez-Medina M, Krishnarajah G. Glycaemic variability and complications in patients with diabetes mellitus: evidence from a systematic review of the literature. Diabetes Obes Metab. 2010; 12:288–298.
7. Satya Krishna SV, Kota SK, Modi KD. Glycemic variability: clinical implications. Indian J Endocrinol Metab. 2013; 17:611–619.
8. Risso A, Mercuri F, Quagliaro L, Damante G, Ceriello A. Intermittent high glucose enhances apoptosis in human umbilical vein endothelial cells in culture. Am J Physiol Endocrinol Metab. 2001; 281:E924–E930.
9. Cavalot F. Do data in the literature indicate that glycaemic variability is a clinical problem? Glycaemic variability and vascular complications of diabetes. Diabetes Obes Metab. 2013; 15:Suppl 2. 3–8.
10. Ceriello A, Esposito K, Piconi L, Ihnat M, Thorpe J, Testa R, Bonfigli AR, Giugliano D. Glucose "peak" and glucose "spike": impact on endothelial function and oxidative stress. Diabetes Res Clin Pract. 2008; 82:262–267.
11. Smith-Palmer J, Brandle M, Trevisan R, Orsini Federici M, Liabat S, Valentine W. Assessment of the association between glycemic variability and diabetes-related complications in type 1 and type 2 diabetes. Diabetes Res Clin Pract. 2014; 105:273–284.
12. Desouza CV, Bolli GB, Fonseca V. Hypoglycemia, diabetes, and cardiovascular events. Diabetes Care. 2010; 33:1389–1394.
13. Standl E, Schnell O, Ceriello A. Postprandial hyperglycemia and glycemic variability: should we care? Diabetes Care. 2011; 34:Suppl 2. S120–S127.
14. Nathan DM, Turgeon H, Regan S. Relationship between glycated haemoglobin levels and mean glucose levels over time. Diabetologia. 2007; 50:2239–2244.
15. Monnier L, Lapinski H, Colette C. Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA(1c). Diabetes Care. 2003; 26:881–885.
16. Suh S, Joung JY, Jin SM, Kim MY, Bae JC, Park HD, Lee MS, Lee MK, Kim JH. Strong correlation between glycaemic variability and total glucose exposure in type 2 diabetes is limited to subjects with satisfactory glycaemic control. Diabetes Metab. 2014; 40:272–277.
17. Rodbard D. New and improved methods to characterize glycemic variability using continuous glucose monitoring. Diabetes Technol Ther. 2009; 11:551–565.
18. Service FJ. Glucose variability. Diabetes. 2013; 62:1398–1404.
19. Rodbard D. Optimizing display, analysis, interpretation and utility of self-monitoring of blood glucose (SMBG) data for management of patients with diabetes. J Diabetes Sci Technol. 2007; 1:62–71.
20. DeVries JH. Glucose variability: where it is important and how to measure it. Diabetes. 2013; 62:1405–1408.
21. Rodbard D. Clinical interpretation of indices of quality of glycemic control and glycemic variability. Postgrad Med. 2011; 123:107–118.
22. Jun JE, Jin SM, Baek J, Oh S, Hur KY, Lee MS, Lee MK, Kim JH. The association between glycemic variability and diabetic cardiovascular autonomic neuropathy in patients with type 2 diabetes. Cardiovasc Diabetol. 2015; 14:70.
23. Jin SM, Kim TH, Bae JC, Hur KY, Lee MS, Lee MK, Kim JH. Clinical factors associated with absolute and relative measures of glycemic variability determined by continuous glucose monitoring: an analysis of 480 subjects. Diabetes Res Clin Pract. 2014; 104:266–272.
24. Inchiostro S, Candido R, Cavalot F. How can we monitor glycaemic variability in the clinical setting? Diabetes Obes Metab. 2013; 15:Suppl 2. 13–16.
25. Schiffrin A, Belmonte M. Multiple daily self-glucose monitoring: its essential role in long-term glucose control in insulin-dependent diabetic patients treated with pump and multiple subcutaneous injections. Diabetes Care. 1982; 5:479–484.
26. Baghurst PA, Rodbard D, Cameron FJ. The minimum frequency of glucose measurements from which glycemic variation can be consistently assessed. J Diabetes Sci Technol. 2010; 4:1382–1385.
27. American Diabetes Association. (6) Glycemic targets. Diabetes Care. 2015; 38:Suppl. S33–S40.
28. Kim SK, Kim HJ, Kim T, Hur KY, Kim SW, Lee MK, Min YK, Kim KW, Chung JH, Kim JH. Effectiveness of 3-day continuous glucose monitoring for improving glucose control in type 2 diabetic patients in clinical practice. Diabetes Metab J. 2014; 38:449–455.
29. Yeh HC, Brown TT, Maruthur N, Ranasinghe P, Berger Z, Suh YD, Wilson LM, Haberl EB, Brick J, Bass EB, Golden SH. Comparative effectiveness and safety of methods of insulin delivery and glucose monitoring for diabetes mellitus: a systematic review and meta-analysis. Ann Intern Med. 2012; 157:336–347.
30. Selvin E, Francis LM, Ballantyne CM, Hoogeveen RC, Coresh J, Brancati FL, Steffes MW. Nontraditional markers of glycemia: associations with microvascular conditions. Diabetes Care. 2011; 34:960–967.
31. Koga M. 1,5-Anhydroglucitol and glycated albumin in glycemia. Adv Clin Chem. 2014; 64:269–301.
32. Koga M, Kasayama S. Clinical impact of glycated albumin as another glycemic control marker. Endocr J. 2010; 57:751–762.
33. Lee EY, Lee BW, Kim D, Lee YH, Kim KJ, Kang ES, Cha BS, Lee EJ, Lee HC. Glycated albumin is a useful glycation index for monitoring fluctuating and poorly controlled type 2 diabetic patients. Acta Diabetol. 2011; 48:167–172.
34. Ogawa A, Hayashi A, Kishihara E, Yoshino S, Takeuchi A, Shichiri M. New indices for predicting glycaemic variability. PLoS One. 2012; 7:e46517.
35. Kim WJ, Park CY. 1,5-Anhydroglucitol in diabetes mellitus. Endocrine. 2013; 43:33–40.
36. Seok H, Huh JH, Kim HM, Lee BW, Kang ES, Lee HC, Cha BS. 1,5-Anhydroglucitol as a useful marker for assessing short-term glycemic excursions in type 1 diabetes. Diabetes Metab J. 2015; 39:164–170.
37. Lachin JM, Genuth S, Nathan DM, Zinman B, Rutledge BN. DCCT/EDIC Research Group. Effect of glycemic exposure on the risk of microvascular complications in the diabetes control and complications trial: revisited. Diabetes. 2008; 57:995–1001.
38. Brownlee M, Hirsch IB. Glycemic variability: a hemoglobin A1c-independent risk factor for diabetic complications. JAMA. 2006; 295:1707–1708.
39. Sartore G, Chilelli NC, Burlina S, Di Stefano P, Piarulli F, Fedele D, Mosca A, Lapolla A. The importance of HbA1c and glucose variability in patients with type 1 and type 2 diabetes: outcome of continuous glucose monitoring (CGM). Acta Diabetol. 2012; 49:Suppl 1. S153–S160.
40. Salardi S, Zucchini S, Santoni R, Ragni L, Gualandi S, Cicognani A, Cacciari E. The glucose area under the profiles obtained with continuous glucose monitoring system relationships with HbA(lc) in pediatric type 1 diabetic patients. Diabetes Care. 2002; 25:1840–1844.
41. Ayano-Takahara S, Ikeda K, Fujimoto S, Hamasaki A, Harashima S, Toyoda K, Fujita Y, Nagashima K, Tanaka D, Inagaki N. Glycemic variability is associated with quality of life and treatment satisfaction in patients with type 1 diabetes. Diabetes Care. 2015; 38:e1–e2.
42. Hsu CR, Chen YT, Sheu WH. Glycemic variability and diabetes retinopathy: a missing link. J Diabetes Complications. 2015; 29:302–306.
43. Jin SM, Kim TH, Oh S, Baek J, Joung JY, Park SM, Cho YY, Sohn SY, Hur KY, Lee MS, Lee MK, Kim JH. Association between the extent of urinary albumin excretion and glycaemic variability indices measured by continuous glucose monitoring. Diabet Med. 2015; 32:274–279.
44. Muggeo M, Verlato G, Bonora E, Zoppini G, Corbellini M, de Marco R. Long-term instability of fasting plasma glucose, a novel predictor of cardiovascular mortality in elderly patients with non-insulin-dependent diabetes mellitus: the Verona Diabetes Study. Circulation. 1997; 96:1750–1754.
45. Ceriello A. Postprandial hyperglycemia and diabetes complications: is it time to treat? Diabetes. 2005; 54:1–7.
46. Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M. STOP-NIDDM Trial Research Group. Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA. 2003; 290:486–494.
47. Deedwania P, Kosiborod M, Barrett E, Ceriello A, Isley W, Mazzone T, Raskin P. American Heart Association Diabetes Committee of the Council on Nutrition, Physical Activity, and Metabolism. Hyperglycemia and acute coronary syndrome: a scientific statement from the American Heart Association Diabetes Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2008; 117:1610–1619.
48. Langouche L, Vanhorebeek I, Van den Berghe G. Therapy insight: the effect of tight glycemic control in acute illness. Nat Clin Pract Endocrinol Metab. 2007; 3:270–278.
49. Coutinho M, Gerstein HC, Wang Y, Yusuf S. The relationship between glucose and incident cardiovascular events. A metaregression analysis of published data from 20 studies of 95,783 individuals followed for 12.4 years. Diabetes Care. 1999; 22:233–240.
50. Waden J, Forsblom C, Thorn LM, Gordin D, Saraheimo M, Groop PH. Finnish Diabetic Nephropathy Study Group. A1C variability predicts incident cardiovascular events, microalbuminuria, and overt diabetic nephropathy in patients with type 1 diabetes. Diabetes. 2009; 58:2649–2655.
51. Zoungas S, Patel A, Chalmers J, de Galan BE, Li Q, Billot L, Woodward M, Ninomiya T, Neal B, MacMahon S, Grobbee DE, Kengne AP, Marre M, Heller S, Group AC. Severe hypoglycemia and risks of vascular events and death. N Engl J Med. 2010; 363:1410–1418.
52. Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, Raskin P, Zinman B. Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005; 353:2643–2653.
53. Jeha GS, Karaviti LP, Anderson B, Smith EO, Donaldson S, McGirk TS, Haymond MW. Insulin pump therapy in preschool children with type 1 diabetes mellitus improves glycemic control and decreases glucose excursions and the risk of hypoglycemia. Diabetes Technol Ther. 2005; 7:876–884.
54. The Diabetes Control and Complications Trial Research Group. Hypoglycemia in the diabetes control and complications trial. Diabetes. 1997; 46:271–286.
55. Kilpatrick ES, Rigby AS, Goode K, Atkin SL. Relating mean blood glucose and glucose variability to the risk of multiple episodes of hypoglycaemia in type 1 diabetes. Diabetologia. 2007; 50:2553–2561.
56. Kim SK, Suh S, Kim MY, Chung HS, Hur KY, Kim SW, Chung JH, Lee MS, Min YK, Kim KW, Kim JH. Three-day continuous glucose monitoring for rapid assessment of hypoglycemic events and glycemic variability in type 1 diabetic patients. Endocr J. 2011; 58:535–541.
57. Monnier L, Colette C. Glycemic variability: should we and can we prevent it? Diabetes Care. 2008; 31:Suppl 2. S150–S154.
58. Krinsley JS. Glycemic variability: a strong independent predictor of mortality in critically ill patients. Crit Care Med. 2008; 36:3008–3013.
59. Brunner R, Adelsmayr G, Herkner H, Madl C, Holzinger U. Glycemic variability and glucose complexity in critically ill patients: a retrospective analysis of continuous glucose monitoring data. Crit Care. 2012; 16:R175.
60. van Haeften TW, Pimenta W, Mitrakou A, Korytkowski M, Jenssen T, Yki-Jarvinen H, Gerich JE. Relative conributions of beta-cell function and tissue insulin sensitivity to fasting and postglucose-load glycemia. Metabolism. 2000; 49:1318–1325.
61. Avignon A, Radauceanu A, Monnier L. Nonfasting plasma glucose is a better marker of diabetic control than fasting plasma glucose in type 2 diabetes. Diabetes Care. 1997; 20:1822–1826.
62. Vora J, Cariou B, Evans M, Gross JL, Harris S, Landstedt-Hallin L, Mithal A, Rodriguez MR, Meneghini L. Clinical use of insulin degludec. Diabetes Res Clin Pract. 2015; 109:19–31.
63. Heinemann L, Fleming GA, Petrie JR, Holl RW, Bergenstal RM, Peters AL. Insulin pump risks and benefits: a clinical appraisal of pump safety standards, adverse event reporting, and research needs: a joint statement of the European Association for the Study of Diabetes and the American Diabetes Association Diabetes Technology Working Group. Diabetes Care. 2015; 38:716–722.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download