Abstract
Stroke is a rare but serious complication of acute myocardial infarction (AMI). Currently, glycoprotein (GP) IIb/IIIa inhibitor is used in clinical practice for acute coronary syndromes and percutaneous coronary interventions (PCIs). The incidence of stroke in patients receiving GP IIb/IIIa inhibitor during PCIs is very low. We report the case of a 47-year-old man who presented with AMI and suffered an acute cerebral infarction after infusion of a GP IIb/IIIa inhibitor following primary PCI.
Stroke is a rare but serious complication of acute myocardial infarction (AMI). The incidence of in-hospital stroke complicating AMI is approximately 1%.1) Hemorrhagic stroke during the first 24 hours is a well-known consequence of thrombolytic therapy. However, even without thrombolytic intervention, both hemorrhagic and ischemic strokes have been documented as complications of AMI and its treatment with anticoagulants.2)
Glycoprotein (GP) IIb/IIIa inhibitors are currently used in clinical practice for acute coronary syndrome and percutaneous coronary intervention (PCI). The incidence of stroke in patients receiving GP IIb/IIIa inhibitor during PCI is very low. Abciximab in addition to aspirin and heparin does not increase the risk of stroke in patients undergoing PCI.3) We report here the case of a 47-year-old man who presented with AMI and suffered from an acute cerebral ischemic stroke after infusion of a GP IIb/IIIa inhibitor following primary PCI.
A 47-year-old male presented to the emergency department at our hospital with prolonged chest pain. Electrocardigraphy revealed ST elevation in lead II, III, and aVF (Fig. 1). Transthoracic echocardiography, which was performed when the patient arrived at the hospital, demonstrated hypokinesia of the inferior wall, preserved systolic function (ejection fraction=50%), no thrombi in the cardiac chambers and no structural abnormalities. The patient was diagnosed as having ST-elevation myocardial infarction and underwent primary PCI.
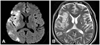
Coronary angiography revealed total occlusion of distal right coronary artery with a large occlusive thrombus (B2, 100%, 0, 0) (Fig. 2). A 0.014 inch Runthrough® guidewire (Terumo, Tokyo, Japan) was passed across the stenotic lesion into the distal vessel. Thrombus aspiration was performed using an Export Aspiration Catheter (Medtronic, Minneapolis, MN, USA) by slowly advancing it during aspiration through the lesion. The lesion was then overlap-stented using a 4.0×23 mm everolimus-eluting stent at 15 atm and a 3.5×24 mm zotarolimus-eluting stent at 15 atm. The final coronary angiogram revealed Thrombolysis In Myocardial Infarction II flow with residual thrombus (Fig. 3), and GP IIb/IIIa inhibitor infusion was initiated. Twelve hours after the infusion, the patient complained of left-sided weakness. Brain magnetic resonance imaging revealed foci of acute to hyperacute infarctions in the right middle cerebral artery territory (Fig. 4). Transesophageal echocardiography demonstrated no right to left shunt flow and no thrombi in the cardiac chambers.
We suspected that systemic thrombolysis associated with intravenous GP IIb/IIIa inhibitor contributed to the fragmentation and lysis of a cardiac thrombus, which subsequently embolized distally to block the cerebral circulation and cause cerebral infarction.
Cerebrovascular events are well known complications that follow AMI, and although they rarely occur, they may have severe or long term adverse effects.
A case-control study reported that the risk of stroke onset was highest shortly after AMI, and nearly 10 times higher than that of patients with stroke but without an MI. This risk declined rapidly to the rate of controls within several days.4) This high risk was attributed to intracardiac thrombus formation, artery-to-artery embolism or in situ thrombosis, in the background of a prothrombotic state secondary to MI. In addition, older age, anterior site of MI, high enzyme levels, impaired left ventricular function, atrial arrhythmias, and prior cerebrovascular disease were the most reliable predictors of stroke during AMI.5) In the present case, although the patient had none of the risk factors mentioned above, cerebral infarction still occurred.
GP IIb/IIIa inhibitors interfere with the final common pathway to platelet aggregation, blocking receptors on activated platelets that bind fibrinogen molecules which form bridges between adjacent platelets. Thus, by competitive inhibition with fibrinogen, GP IIb/IIIa inhibitors could support endogenous thrombolysis by reducing thrombus growth and preventing thrombus reformation. Although intravenous thrombolysis with recombinant tissue plasminogen activator is the only treatment with proven benefits on improved functional outcome up to 4.5 hours from symptom onset in patients with acute ischemic stroke, a GP IIb/IIIa inhibitor might also be useful in patients with ischemic stroke.6) The known complications of GP IIb/IIIa inhibitor therapy are limited to hemorrhage, thrombocytopenia7) and allergic reactions.8)
Although symptomatic intracerebral hemorrhage is a more common and severe side effect of the use of GP IIb/IIIa inhibitors, in this case, ischemic stroke occurred after infusion of a GP IIb/IIIa inhibitor. The present case is unique in that the ischemic stroke occurred during GP IIb/IIIa inhibitor infusion for AMI after primary PCI. The most likely mechanism is fragmentation of an intracardiac thrombus by the use of a GP IIa/IIIa inhibitor.9)
In conclusion, this case highlights that the administration of intravenous administration of a GP IIb/IIIa inhibitor may lead to fragmentation and lysis of an intracardiac thrombus with subsequent embolization to cerebral arteries and ischemic stroke.
Figures and Tables
Fig. 2
Coronary angiogram reveals total occlusion of distal right coronary artery with a large occlusive thrombus.

Fig. 3
Coronary angiogram after stent implantation demonstrates adequate luminal diameter of distal right coronary artery but residual thrombus.

Fig. 4
Brain magnetic resonance scan reveals acute ischemic infarction in the right middle cerebral artery territory after glycoprotein IIb/IIIa inhibitor infusion. A diffusion-weighted image reveals a region of hyperintensity in the distribution of the right middle cerebral artery (A). A T2-weighted image demonstrates a high signal intensity in the territory of the right middle cerebral artery (B).
References
1. Hess DC, D'Cruz IA, Adams RJ, Nichols FT 3rd. Coronary artery disease, myocardial infarction, and brain embolism. Neurol Clin. 1993. 11:399–417.
2. Komrad MS, Coffey CE, Coffey KS, McKinnis R, Massey EW, Califf RM. Myocardial infarction and stroke. Neurology. 1984. 34:1403–1409.
3. Akkerhuis KM, Deckers JW, Lincoff AM, et al. Risk of stroke associated with abciximab among patients undergoing percutaneous coronary intervention. JAMA. 2001. 286:78–82.
4. Mooe T, Olofsson BO, Stegmayr B, Eriksson P. Ischemic stroke: impact of a recent myocardial infarction. Stroke. 1999. 30:997–1001.
5. Behar S, Tanne D, Abinader E, et al. Cerebrovascular accident complicating acute myocardial infarction: incidence, clinical significance and short- and long-term mortality rates. Am J Med. 1991. 91:45–50.
6. Torgano G, Zecca B, Monzani V, et al. Effect of intravenous tirofiban and aspirin in reducing short-term and long-term neurologic deficit in patients with ischemic stroke: a double-blind randomized trial. Cerebrovasc Dis. 2010. 29:275–281.
7. Oh YJ, Park TH, Choi YJ, et al. Abciximab (ReoPro)-induced thrombocytopenia diagnosed through measurement of heparin-dependent antibody. Korean Circ J. 2009. 39:75–78.
8. Frishman WH, Burns B, Atac B, Alturk N, Altajar B, Lerrick K. Novel antiplatelet therapies for treatment of patients with ischemic heart disease: inhibitors of the platelet glycoprotein IIb/IIIa integrin receptor. Am Heart J. 1995. 130:877–892.
9. Chang GY. An ischemic stroke during intravenous recombinant tissue plasminogen activator infusion for evolving myocardial infarction. Eur J Neurol. 2001. 8:267–268.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download