Abstract
Figures and Tables
Fig. 2
Chest radiographs of four patients. (A) Embolization of the remnant lead tip (arrow) after lead extraction in Patient 1. (B) The remaining lead tip (arrow) after lead extraction in Patient 2. (C) The remnant lead tip (arrow) after lead extraction in Patient 3. A new pacemaker was implanted on the contralateral side. (D) The remnant lead tip (arrow) after lead extraction in Patient 4. A new epicardial pacemaker was implanted.

Fig. 3
Chest radiographs of patient 5. (A) The lead of the right sided pacemaker (generator removed previously): and the left sided VVI pacemaker. (B) The remnant lead tip (arrow) after lead extraction. (C) The remnant lead tip (arrow) and the VVI pacemaker implanted three months after lead extraction. (D) The newly implanted epicardial pacemaker after surgical removal. VVI: ventricular demand pacing.
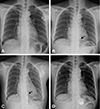
Table 1-1
Baseline characteristics and clinical manifestation

PPM: permanent pacemaker, DDD: dual chamber pacing, SSS: sick sinus syndrome, CAVB: complete atrioventricular block, VDD: atrial synchronous, ventricular demand pacing, TBS: tachy-brady syndrome, VVI: ventricular demand pacing, MSSA: methicillin-susceptible Staphylococcus aureus, RV: right ventricle, RA: right atrium, TV: tricuspid valve, IAS: interatrial septum
Table 1-2
Treatment and follow-up

*These 2 patients underwent surgery for the lead removal initially: but the atrial and ventricular leads could not be removed: and decision was made to perform a secondary lead removal via a transvenous approach. IV: intravenous, FU: follow up, DT: direct traction, CT: counter traction, V: ventricle, TV: tricuspid valve, RV: right ventricle, TEI: teicoplanin, PO: per os, CFX: cefixime, VAN: vancomycin, AMP/SUL: ampicillin/sulbactam, GEN: gentamycin, RIF: rifampin, NAF: nafcillin, LFX: levofloxacin, ARB: arbekacin




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download