Abstract
Background and Objectives
Predictive factors of mortality in acute coronary syndrome (ACS) patients with left ventricular dysfunction were analyzed during 5-year clinical follow-up after percutaneous coronary intervention (PCI).
Subjects and Methods
A total of 329 ACS consecutive patients (64.6±11.3 years, 227 males) who underwent PCI from January 2001 to March 2006 were followed for 5 years. All patients had lower than 40% of left ventricular ejection fraction (LVEF). Patients were divided into Group I (survived longer than 5-years: n=130, 101 males) and Group II (survived shorter than 5 years: n=199, 126 males).
Results
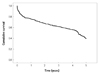
The cumulative survival rate was 88.0% at 1 month, 78.0% at 6 months, 75.0% at 1 year, 67.0% at 2 years, 62.0% at 3 years, 57.0% at 4 years and 40% at 5-years. Group II was older (61.6±11.2 years vs. 66.4±11.4 years, p<0.001), and showed higher prevalence of female gender (28.4% vs. 36.7%, p=0.006) and lower LVEF (35.3±5.2 vs. 33.6±5.6) than Group I. The independent predictors for mortality were LVEF <30% {odds ratio (OR)=1.793, 95% confidence interval (CI): 1.234-2.452, p=0.002}, serum creatinine >3.0 mg/dL (OR=2.455, 95% CI: 1.306-4.614, p=0.005), older than 65 years (OR=1.594, 95% CI: 1.152-2.206, p=0.005), and female gender (OR=1.524, 95% CI: 1.090-2.130, p=0.014).
In Korea, the prevalence of acute coronary syndrome (ACS) patients is increasing, as is resultant mortality.1) High-risk ACS patients require active treatment because of very high mortality. Recent treatment guidelines recommend percutaneous coronary intervention (PCI) as an active invasive method at the early stage for high-risk patients.2) Left ventricular ejection fraction (LVEF) is a very important clinical factor for diagnosis, treatment, and prognosis, particularly for patients with acute myocardial infarction (AMI).3) Recently, PCI has been more widely used in patients with left ventricular dysfunction because of advanced techniques and instruments. Previous reports showed that a major adverse cardiac event (MACE) following PCI was associated with pre-procedural left ventricular dysfunction,4) and survival rate at the acute stage and the later stage was higher in patients with normal left ventricular function compared to those with left ventricular dysfunction.5) Age, renal insufficiency, multi-vessel disease, and left ventricular dysfunction obviously also affect short-term survival rate of patients with AMI undergoing PCI.6) In a study investigating mortality after PCI in patients with left ventricular dysfunction, the survival rate tended to be lower in patients with low LVEF than in those with normal LVEF.7) However, there has been no established definite predictor of long-term survival after PCI in patients with ACS accompanied by left ventricular dysfunction. Therefore, the present study aimed at identifying factors affecting the long-term survival rate after PCI in ACS patients with low LVEF.
From January 2001 to March 2006, a total of 329 patients with ACS undergoing PCI and preprocedural LVEF below 40% was analyzed. They were divided into the group surviving 5 years or longer {Group I, n=130, sex ratio (M : F)=101 : 29} and the group surviving less than 5 years {Group II, n=199, sex ratio (M : F)=126 : 73}.
We divided 329 ACS patients who admitted to Chonnam National University Hospital and LVEF below 40% into the group surviving 5 years or longer (Group I) and the group surviving less than 5 years (Group II), and examined differences between the two groups in sex, age, clinical diagnosis, LVEF, coronary disease risk factors (hypertension, diabetes mellitus, smoking, hypercholesterolemia), laboratory findings, coronary angiographic characteristics, and concomitant medication. LVEF was measured by Simpson's method.8) The morphological characteristics of coronary artery lesions were analyzed through the classification method of the American College of Cardiology/American Heart Association (ACC/AHA).9) Blood flow was classified using Thrombolysis in Myocardial Infarction (TIMI).10) Significant stenosis of lesion was defined narrowing of the coronary artery more than 75%. Successful reperfusion was defined as post-procedural TIMI flow of III with residual stenosis less than 25%. A total of 254 (77.2%) patients were followed up by clinical visits. The other patients were followed-up by telephone and mail to ascertain the occurrence of long-term outcomes. A total of 329 (100%) patients were followed for up to 5 years.
For continuous variables, the differences between the 2 groups were evaluated by an independent sample t-test or Mann-Whitney rank-sum test, and were presented in mean±standard deviation. For discrete variables, differences were expressed as counts and percent-ages and percentages were analyzed with chi-square test between the groups as appropriate. We constructed Kaplan-Meier curves for survival rate. Cox regression was used in order to identify independent prognostic factors. All statistical analyses were 2-tailed, with clinical significance defined as p<0.05. All statistical analyses were performed with Statistical Package for the Social Sciences (SPSS version 18.0, SPSS Inc., Chicago, IL, USA).
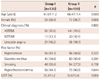
A total 329 patients were analyzed and they were divided into Group I (n=130, 39.5%) and Group II (n=199, 60.5%). The cumulative survival rate in these patients was 88.0% in 1 month, 78.0% in 6 months, 75.0% in 1 year, 67.0% in 2 years, 62.0% in 3 years, 57.0% in 4 years, and 40.0% in 5 years (Fig. 1). The average age was significantly higher in Group II than Group I (61.6±11.2 vs. 66.4±11.4 years old, p<0.001). Female gender was more common in Group II than Group I {29 (28.4%) vs. 73 (36.7%), p=0.006}. Disease distribution included 233 (70.8%) patients with acute ST elevation myocardial infarction, 37 (11.2%) patients with non-ST elevation myocardial infarction, and 59 (17.9%) patients with unstable angina, no difference between the two groups. As to the risk factors of cardiovascular disease, 100 (30.4%) patients were smokers, 135 (41.0%) patients had hypercholesterolemia, 152 (46.2%) hypertension, and 125 (38.0%) diabetes mellitus, and there was no significant difference between the two groups. In echocardiogram, the mean LVEF was significantly higher in Group I than Group II (35.3±5.2% vs. 33.6±5.6%, p=0.004) (Table 1).
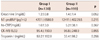
The creatinine level was 1.2±0.8 mg/dL in Group I and 1.4±1.4 mg/dL in Group II, and there was no significant difference between the two groups (p=0.052). N-terminal B-type natriuretic peptide was 4701±6586.9 pg/mL in Group I and 12411±40229.5 pg/mL in Group II and high-sensitivity C-reactive protein was 1.6±3.0 mg/dL and 5.2±38.1 mg/dL, respectively, and there were no significant differences between the two groups. Creatine kinase-MB on visit was 95.4±150.9 U/L in Group I and 96.8±248.9 U/L in Group II, and there was no significant difference between the two groups. Troponin I on visit was 50.2±152.8 ng/mL in Group I and 33.4±86.2 ng/mL in Group II, and there was no significant difference between the two groups (Table 2).
In coronary angiographic findings, culprit lesion was left main in 13 patients (4.0%), left anterior descending artery in 189 (57.4%), right coronary artery in 74 (22.5%), and left circumflex artery in 49 (14.9%). The number of involved vessels was one in 182 patients (55.3%), two in 91 (27.7%), and three in 52 (15.8%). The lesion type according to ACC/AHA classification was A in 0 patient (0%), B1 in 103 (31.3%), B2 in 98 (29.8%), and C in 128 (38.9%). The type of coronary flow according to TIMI classification was 0 in 131 patients (39.8%), I in 18 (5.5%), II in 89 (27.1%), and III in 82 (24.9%). The number of patients who underwent intra-aortic balloon pump insertion was 31 (15.6%) in Group I and 19 (14.6%) in Group II. The number of patients who used abciximab was 25 (19.28%) in Group I and 29 (14.6%) in Group II. The PCI success rate was 90.8% (118/130) in Group I and 93.0% (185/199) in Group II, and there was no significant difference between the two groups (Table 3).
All the patients were prescribed aspirin and clopidogrel, and beta blocker was prescribed to 114 patients (87.7%) in Group I and 165 (85.1%) in Group II, angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker to 119 (91.5%) in Group I and 167 (86.1%) in Group II, statin to 82 (63.1%) in Group I and 121 (61.0%) in Group II, and calcium channel blocker to 65 (50.0%) in Group I and 88 (44.7%) in Group II. There were no significant differences between the two groups in any medication (Table 4).
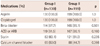
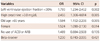
Cox regression survival analysis was used to identify independent predictors affecting 5-year mortality. Significant predictors for mortality were LVEF below 30% {odds ratio (OR)=1.793, 95% confidence interval (CI): 1.234-2.452, p=0.002}, serum creatinine over 3.0 mg/dL (OR=2.455, 95% CI: 1.306-4.614, p=0.005), age over 65 (OR=1.594, 95% CI: 1.152-2.206, p=0.005), and female gender (OR=1.524, 95% CI: 1.090-2.130, p=0.014) (Table 5).
Cardiovascular disease is increasing steadily not only in developed countries but also in Korea, and is one of the most common cause of death. Among cardiovascular diseases, ACS comprises over 50% of deaths and the prevalence is also rising steadily. Mortality becomes higher if patients have ACS accompanied by left ventricular dysfunction. Therefore, the present study was to analyze factors that might predict death in ACS patients with low LVEF in order to identify high-risk patients earlier and enhance survival. The present study showed that independent predictors affecting the long-term survival rate were low LVEF, high serum creatinine, old age, and female gender.
In the present study, the cumulative survival rate was 88.0% in 1 month, 78.0% in 6 months, 75.0% in 1 year, 62.0% in 3 years, and 40.0% in 5 years. In a previous study regarding all AMI patients, the cumulative survival rate was 87.0% in the initial 48 hours and 83.0% in 1 year, and went down to 81.0%, 79.0% and 77.0% each year.10) The reason for the lower survival rate in the present study compared with previous study was the patients in the present study were limited to ACS patients with LVEF lower than 40%. Considering that a study with Korean subjects showed similar survival rates at 1-year 89.2% and at 2-year 86.2%, LVEF is believed to have a significant effect on the survival rate in the present study.11) Furthermore, survival analysis in the present study showed that mortality was the highest within 1 year, especially within 6 months. It might suggest that clinicians should give more intensive care in acute phase after PCI in ACS patients with low LVEF.
Left ventricular function measured by echocardiogram is known to be an objective and important marker for evaluating the prognosis of AMI patients.12) It has been proved by many studies that left ventricular function is an important prognostic factor affecting the survival rate.13-15) In the present study as well, LVEF below 30% as an independent variable measured by echocardiogram was an important prognostic factor affecting the 5-year survival rate. Accordingly, it might be essential to evaluate ventricular function with echocardigram during ACS patients' hospital stay and it is important in planning patient treatment and predicting survival.
Walsh et al.16) reported that decreased glomerular filtration rate was associated with worse clinical outcomes and was an independent predictor for in-hospital mortality in patients with STEMI undergoing primary PCI. Also, the previous study showed that patients with serum creatinine over 1.5 mg/dL showed higher 1-year mortality than those with normal level,17) and serum creatinine level higher than 3.0 mg/dL was an independent predictor affecting the 5-year long-term survival rate. Analysis with Korea Heart Dysfunction Registry showed that serum creatinine level higher than 2.0 mg/dL as independent predictor for long term clinical outcomes (hazard ratio=2.29, 95% CI: 1.90-2.76).18) Like these reports, the present study also showed that serum creatinine level was an independent predictor affecting not only the 1-year short-term survival rate but also the 5-year long survival rate. Therefore, it would be helpful for improving the survival rate in ACS patients with low LVEF and renal insufficiency undergoing PCI through combination of treatments for renal dysfunction and active treatment for cardiovascular disease.
As to difference according to gender, previous studies showed inconsistent results. Choi et al.19) reported that cumulative mortality was 21% in men and 30% in women, indicating significantly higher women's mortality than men. Even more, the Minnesota Heart Survey20) showed that women's mortality was higher than men's among AMI patients even after correction for factors such as clinical symptoms and past history. Also, He et al.21) studied the prognosis of 754 patients admitted for AMI and found that women had higher than men in short-term (relative odds=1.74, 95% CI: 1.17-2.60) and long-term mortality (51% vs. 35.9%, log rank p=0.002). In the present study as well, female gender was found to be an independent predictor affecting ACS patients' 5-year survival rate. In contrast, Maynard et al.22) and Karlson et al.23) reported that the short-term mortality of AMI patients did not showed any significance after correction with age between men and women, although unadjusted mortality was higher in women than men (16% in women vs. 11% in men). Also, Fiebach et al.24) reported that AMI patients' mortality on admission and for 3 years were higher in women than in men, but no difference was observed between men and women after correction for basic clinical characteristics. This might be explained that although mortality is higher in women than men, gender itself is not an independent risk factor for long-term survival in patients with ACS. This phenomenon was caused by women's comorbidities, especially hypertension, diabetes and left ventricular dysfunction. In the present study, women's mortality was higher than men's, and female gender itself was found to be an independent predictor for long-term prognosis in ACS patients with low EF even after adjusting confounding factors including basic demographic findings. It might suggest that female gender itself is an important prognostic factor for the ACS patients in the situation of low LVEF. However, larger-scale prospective research may be necessary to get more accurate results.
The present study has several limitations. First, it was conducted as long-term retrospective research. Larger scale prospective randomized clinical trials are needed to support the results of the present study. Second, the cause of death could not be confirmed for some cases. Third, the effect of continuous drug therapy, drug switch and stopping of medication were not measured completely in all patients.
In conclusion, the 5-year survival rate was 40% among 329 ACS patients with LVEF below 40% who underwent PCI during the period from January 2001 to March 2006. And LVEF below 30%, serum creatinine over 3.0 mg/dL, age over 65, and being female were independent predictors for the 5-year survival rate in ACS patients undergoing PCI with low LVEF.
Figures and Tables
Acknowledgments
This study was conducted with the support of the Health & Medical Technology R&D Program of the Ministry of Health and Welfare (A084869).
References
1. Korea National Statistical Office. 2004 annual report on the course of as death statistics. 2004. Korea National Statistical Office;32–34.
2. Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction). Circulation. 2004. 110:e82–e292.
3. Pfeffer MA, Braunwald E, Moyé LA, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction: results of the survival and ventricular enlargement trial: the SAVE Investigators. N Engl J Med. 1992. 327:669–677.
4. Schühlen H, Kastrati A, Dirschinger J, et al. Intracoronary stenting and risk for major adverse cardiac events during the first month. Circulation. 1998. 98:104–111.
5. Kohli RS, DiSciascio G, Cowley MJ, Nath A, Goudreau E, Vetrovec GW. Coronary angioplasty in patients with severe left ventricular dysfunction. J Am Coll Cardiol. 1990. 16:807–811.
6. Halkin A, Singh M, Nikolsky E, et al. Prediction of mortality after primary percutaneous coronary intervention for acute myocardial infarction: the CADILLAC risk score. J Am Coll Cardiol. 2005. 45:1397–1405.
7. Holper EM, Blair J, Selzer F, et al. The impact of ejection fraction on outcomes after percutaneous coronary intervention in patients with congestive heart failure: an analysis of the National Heart, Lung, and Blood Institute Percutaneous Transluminal Coronary Angioplasty Registry and Dynamic Registry. Am Heart J. 2006. 151:69–75.
8. Quinones MA, Waggoner AD, Reduto LA, et al. A new, simplified and accurate method for determining ejection fraction with two-dimensional echocardiography. Circulation. 1981. 64:744–753.
9. Scanlon PJ, Faxon DP, Audet AM, et al. ACC/AHA guidelines for coronary angiography: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on Coronary Angiography): developed in collaboration with the Society for Cardiac Angiography and Interventions. J Am Coll Cardiol. 1999. 33:1756–1824.
10. Gibson CM, Cannon CP, Daley WL, et al. TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation. 1996. 93:879–888.
11. Gwon HC, Lyu OY, Park SW, et al. Long term survival rate and prognostic factors of acute myocardial infarction. Korean Circ J. 1990. 20:687–696.
12. Zannad F, Briancon S, Juilliere Y, et al. Incidence, clinical and etiologic features, and outcomes of advanced chronic heart failure: the EPICAL Study: Epidémiologie de l'Insuffisance Cardiaque Avancée en Lorraine. J Am Coll Cardiol. 1999. 33:734–742.
13. Halkin A, Stone GW, Dixon SR, et al. Impact and determinants of left ventricular function in patients undergoing primary percutaneous coronary intervention in acute myocardial infarction. Am J Cardiol. 2005. 96:325–331.
14. Kouvaras G, Cokkinos D, Spyropoulou M. Increased mortality of diabetics after acute myocardial infarction attributed to diffusely impaired left ventricular performance as assessed by echocardiography. Jpn Heart J. 1988. 29:1–9.
15. Krumholz HM, Howes CJ, Murillo JE, Vaccarino LV, Radford MJ, Ellerbeck EF. Validation of a clinical prediction rule for left ventricular ejection fraction after myocardial infarction in patients > or = 65 years old. Am J Cardiol. 1997. 80:11–15.
16. Walsh CR, O'Donnell CJ, Camargo CA Jr, Giugliano RP, Lloyd-Jones DM. Elevated serum creatinine is associated with 1-year mortality after acute myocardial infarction. Am Heart J. 2002. 144:1003–1011.
17. Kim JY, Jeong MH, Ahn YK, et al. Decreased glomerular filtration rate is an independent predictor of in-hospital mortality in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Korean Circ J. 2011. 41:184–190.
18. Tofler GH, Stone PH, Muller JE, et al. Effects of gender and race on prognosis after myocardial infarction: adverse prognosis for women, particularly black women. J Am Coll Cardiol. 1987. 9:473–482.
19. Choi DJ, Han S, Jeon ES, et al. Characteristics, outcomes and predictors of long-term mortality for patients hospitalized for acute heart failure: a report from the Korean Heart Failure Registry. Korean Circ J. 2011. 41:363–371.
20. Demirovic J, Blackburn H, McGovern PG, Luepker R, Sprafka JM, Gilbertson D. Sex differences in early mortality after acute myocardial infarction (the Minnesota Heart Survey). Am J Cardiol. 1995. 75:1096–1101.
21. He J, Klag MJ, Whelton PK, Zhoa Y, Weng X. Short- and long-term prognosis after acute myocardial infarction in Chinese men and women. Am J Epidemiol. 1994. 139:693–703.
22. Maynard C, Litwin PE, Martin JS, Weaver WD. Gender differences in the treatment and outcome of acute myocardial infarction: Results from the Myocardial Infarction Triage and Intervention Registry. Arch Intern Med. 1992. 152:972–976.
23. Karlson BW, Herlitz J, Hartford M. Prognosis in myocardial infarction in relation to gender. Am Heart J. 1994. 128:477–483.
24. Fiebach NH, Viscoli CM, Horwitz RI. Differences between women and men in survival after myocardial infarction: biology or methodology? JAMA. 1990. 263:1092–1096.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download