Abstract
Background and Objectives
Making the noninvasive diagnosis of coronary artery disease in patients with a permanent pacemaker is difficult because of the inability to interpret electrocardiograms and the low specificity of perfusion scintigraphy. We evaluated the diagnostic accuracy of noninvasive pacemaker stress echocardiography (PASE) as a screening test for coronary artery disease in patients with atypical angina and a permanent pacemaker.
Subjects and Methods
This a prospective study, and transthoracic stress-pacing echocardiography was performed on 15 patients (9 men and 6 women; age, mean age: 71.1±11.0 years) with atypical angina and a permanent pacemaker. All the patients underwent noninvasive pacemaker-stress echocardiography by external programming (pacing the heart rate up to 150 beats per minute). Coronary angiography was performed on the 8 patients with positive PASE results. Significant coronary artery disease was defined as ≥70% stenosis in at least one major coronary artery.
Results
The echocardiographic images were interpretable for all the patients. No significant side effects were observed. The left ventricular systolic function was preserved in all the patients (left ventricular ejection fraction; 63.5±8%). Only 5 (62.5%) of 8 patients showed significant coronary artery disease, as documented by coronary angiography.
There are various methods to diagnose coronary artery disease (CAD). Because assessing the electrocardiographic rhythm induced by right ventricular pacing is difficult, non-invasively diagnosing CAD in patients who have a conventional pacemaker (PM) is an extremely difficult task.1) Perfusion scintigraphy may have low specificity or sensitivity in patients with a conventional, permanent PM,2) which is perhaps due to the impaired coronary flow reserve that's caused by alterations of left ventricular mechanical activation and the increased extramural compressive forces.3)
Noninvasive pacemaker stress echocardiography (PASE) can increase the heart rate and induce myocardial ischemia in these patients.4,5) We evaluated the diagnostic accuracy of performing noninvasive PASE as a screening test for coronary artery disease in patients with atypical angina and a permanent pacemaker.
Between May and September 2006, transthoracic stress-pacing echocardiography was performed on 15 patients (9 men and 6 women, median age: 71.1±11.0 years) with atypical angina and a permanent pacemaker. All the patients gave us their written informed consent for this study's protocol. Patients with recent myocardial infarction (<2 months), clinical signs of unstable angina, congestive heart failure, significant valvular heart disease, a prior coronary angiographic history or poor echocardiographic images were excluded.
PASE was performed by a single trained cardiologist, who was blinded to the clinical data, and with using commercially available Sequoir C-512 Ultrasound equipment (Acuson Inc., Mountain View, CA, USA) with a 3.5 MHz transducer. The images were obtained with the patient in the left lateral decubitus position and they were acquired before the stress test and every 2 minutes throughout the stress test using the standard parasternal and apical views. Continuous pacing was started at 100 beats per minute (bpm) and the heart beat was increased every 2 min (maximum-150 bpm) until a test endpoint was reached. Test endpoints were achieved by reaching the maximal ventricular pacing (heart rate 150 bpm), severe angina, systolic blood pressure decreases greater than 40 mmHg, regional wall motion abnormality or significant cardiac arrhythmias. The echocardiograms were recorded in a quad-screen format. Two experienced cardiologists, who were unaware of the clinical data, scored the echocardiograms using a standard 16-segment model as suggested by the American Society of Echocardiography.6) Regional wall motion and systolic wall thickening were scored on a 5-point scale. A segment with normal motion was scored as 1, a mild hypokinetic segment as 2, a severe hypokinetic segment as 3, an akinetic segment as 4 and a dyskinetic segment as 5. Ischemia was defined as new or worsened wall motion abnormalities during stress, as indicated by an increase of the wall motion score ≥1 grade in at least one segment. Ischemia was not present when the akinetic segments were at rest became the seg-ments became dyskinetic during stress. The myocardial septal and apical functions were evaluated on the basis of systolic thickening because the wall motion could be influenced by ventricular pacing.
Coronary angiograms were performed via the femoral approach on the 8 patients with positive test results. The angiograms were analyzed independent of the echocardiographic results by two experienced cardiologists. Coronary lesions were assessed with multiple orthogonal views and they were visually evaluated for the morphologic features that were similar to those reported by the American College of Cardilology/American Heart Association (ACC/AHA). Significant coronary stenosis was defined as a 70% or more narrowing of the luminal diameter in one or more major coronary arteries. Coronary artery disease was defined as the presence of at least one coronary vessel with significant stenosis.
The study population consisted of 15 patients (9 men, mean age: 71.1±11.0 years). The clinical and laboratory data is summarized in Table 1. All patients had hypertension and two patients had diabetes mellitus. The pacemaker had been implanted for a mean period of 61±52 months. The electrocardiogram (ECG) data and pacemaker characteristics are presented in Table 2.
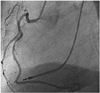
The echocardiographic images were interpretable in all the patients. No significant side effects were observed. The left ventricular systolic function was preserved in all the patients [mean left ventricular ejection fraction (LVEF): 63.5%±8.0%]. No tests were stopped due to chest pain or severe hypotension, and 8 of 15 patients showed wall motion abnormalities during pacemaker pacing. Fig. 1 shows a positive example of PASE. All the 8 patients had coronary angiography performed, but only 5 (62.5%) patients showed significant coronary artery disease as documented by coronary angiography. The other 3 patients showed correct correlation between their coronary angiography and the PASE in the coronary territories. Fig. 2 shows an example of a positive coronary angiogram with significant right coronary artery stenosis, which correlated with the PASE results (Figs. 1 and 2). One patient underwent a coronary artery bypass graft due to disease in 3 vessels and there was little indication for performing percutaneous coronary intervention in that patient.
Dobutamine stress echocardiography and methoxyisobutylisonitrile (MIBI) single photon emission computerized tomography (SPECT) can detect coronary artery disease.7) Functional imaging with either radionuclide ventriculography and intravenous pacing, or two-dimensional (2D) echocardiography associated with transesophageal atrial pacing8-10) can also help detect CAD, with lower feasibility, suboptimal patient tolerance11,12) and long preparation time.
An increased heart rate increases the myocardial oxygen demand such that tachycardia may exceed the fixed coronary flow reserve in the presence of hemodynamically significant CAD. The change in the subendocardial-to-subepicardial flow ratio that's associated with rapid pacing in the presence of a tight coronary stenosis13) is important for the development of regional dysfunction since the percent regional systolic thickening is linearly and tightly related to the subendocardial flow, and not to the transmural flow.14)
Perfusion scintigraphy may have low specificity or sensitivity in patients with a conventional, permanent PM, and perhaps this because of the impaired coronary flow reserve that's due to alterations of left ventricular mechanical activation and the increased extramural compressive forces. Grines et al.15) suggested that the reduced specificity of thallium scintigraphy in patients with permanent cardiac pacemaker dependency results from a change in the myocardial perfusion following asynchronous contraction of the interventricular septum. In patients with permanent right ventricular pacing, perfusion defects can often be found in the inferior and apical walls, which are probably the earliest activated sites under right ventricular apical pacing. However, myocardial perfusion abnormalities also occur in the septum and apex in the absence of coronary artery disease in patients with paced rhythm.16)
The regional coronary flow reserve can be impaired in the dominant coronary artery that perfuses these regions, whereas it is usually normal in the left anterior descending coronary artery. This abnormality is at least partially responsible for the uncertain specificity of stress myocardial scintigraphy.
Picano et al.5) evaluated the feasibility, safety and diagnostic accuracy of pacemaker stress echocardiography in 46 consecutive patients with a permanent pacemaker and they had suspected or known coronary artery disease. The sensitivity for detecting significant coronary artery disease was 70%, the specificity was 90% and the accuracy was 78%.
Forty-two of 46 patients (91%) achieved the target heart rate or a positive test endpoint. Four patients (9%) had a submaximal test. Pacemaker echocardiography is a simple, rapid and safe test for assessing those patients suffering with CAD, even when a permanent pacemaker is present. Pacemaker stress echocardiography seems to be less time-consuming and it is associated with fewer side effects than dobutamine stress testing; thus, it represents a reasonable choice for assessing myocardial ischemia.
We showed that the prognosis obtained with the PASE test matched with an invasive coronary angiogram performed in the patients with atypical angina and a permanent pacemaker. The major pathophysiologic limitation is that pacing stress only increases in heart rate, leading to a lower rate-pressure product than is produced during exercise stress testing. Despite the small number of patients, our single-center experience implies that noninvasive PASE is a simple, rapid, safe and diagnostically efficient tool to test for coronary artery disease following chest discomfort in patients with a permanent pacemaker. Larger studies are necessary to validate our findings.
Figures and Tables
Fig. 1
Pacemaker stress echocardiography. A: baseline echocardiography showed normal regional wall motion. B: pacemaker stress echocardiography showed no regional wall thickening in the basal posterior wall (arrow) on the PLX view and inferior wall (two headed arrow) on the 2 ch view at fixed pacing of 100 bpm compared with those at baseline. PLX: parasternal long-axis, PSX: parasternal short-axis, 4 ch: four-chamber view, 2 ch: two-chamber view.

Fig. 2
Coronary angiography showed a significant stenosis in the mid-portion of the right coronary artery.
References
1. Chaitman BR. Braunwald E, editor. Exercise stress testing. Heart Disease: A Textbook of Cardiovascular Medicine. 2001. 6th ed. Philadelphia: Saunders;129–155.
2. Lakkis NM, He ZX, Verani MS. Diagnosis of coronary artery disease by exercise thallium-201 tomography in patients with a right ventricular pacemaker. J Am Coll Cardiol. 1997. 29:1221–1225.
3. Skalidis EI, Kochiadakis GE, Koukouraki SI, et al. Myocardial perfusion in patients with permanent ventricular pacing and normal coronary arteries. J Am Coll Cardiol. 2001. 37:124–129.
4. Benchimol D, Mozanof M, Dubroca B, et al. Detection of coronary stenoses by stress echocardiography using a previously implanted pacemaker for ventricular pacing: preliminary report of a new method. Clin Cardiol. 2000. 23:842–848.
5. Picano E, Alaimo A, Chubuchny V, et al. Noninvasive pacemaker stress echocardiography for diagnosis of coronary artery disease: a multicenter study. J Am Coll Cardiol. 2002. 40:1305–1310.
6. Armstrong WF, Pellikka PA, Ryan T, Crouse L, Zoghbi WA. Stress echocardiography: recommendations for performance and interpretation of stress echocardiography. J Am Soc Echocardiogr. 1998. 11:97–104.
7. Choi SJ, Kim HS, Seo JD. Identification of ischemic myocardium with simultaneous dobutamine stress echocardiography and 99mTC-MIBI SPECT in patients with suspected coronary artery disease. Korean Circ J. 1993. 23:960–971.
8. Tzivoni D, Weiss AT, Solomon J, et al. Diagnosis of coronary artery disease by multigated radionuclide angiography during right atrial pacing. Chest. 1981. 80:562–565.
9. Chapman PD, Doyle TP, Troup PJ, Gross CM, Wann LS. Stress echocardiography with transesophageal atrial pacing: preliminary report of a new method for detection of ischemic wall motion abnormalities. Circulation. 1984. 70:445–450.
10. Atar S, Nagai T, Cercek B, Nagvi TZ, Luo H, Siegel RJ. Pacing stress echocardiography: an alternative to pharmacologic stress testing. J Am Coll Cardiol. 2000. 36:1935–1941.
11. Marangelli V, Iliceto S, Piccinni G, De Martino G, Sorgente L, Rizzon P. Detection of coronary artery disease by digital stress echocardiography: comparison of exercise, transesophageal atrial pacing and dipyridamole echocardiography. J Am Coll Cardiol. 1994. 24:117–124.
12. Schroder K, Voller H, Dingerkus H, et al. Comparison of the diagnostic potential of four echocardiographic stress tests shortly after acute myocardial infarction: submaximal exercise, transesophageal atrial pacing, dipyridamole, and dobutamine-atropine. Am J Cardiol. 1996. 77:909–914.
13. Gong G, Ugurbil K, Zhang J. Transmural metabolic heterogeneity at high cardiac work states. Am J Physiol. 1999. 277:H236–H242.
14. Takeuchi M, Nohtomi Y, Kuroiwa A. Effect of ventricular pacing on coronary blood flow in patients with normal coronary arteries. Pacing Clin Electrophysiol. 1997. 20:2463–2469.
15. Grines CL, Bashore TM, Boudoulas H, Olson S, Shafer P, Wooley CF. Functional abnormalities in isolated left bundle branch block: the effect of interventricular asynchrony. Circulation. 1989. 79:845–853.
16. Picano E. Stress Echocardiography. 2003. 4th ed. Heidelberg: Springer Verlag.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download