Abstract
Purpose
To evaluate the ultrasonographic measurements of the thickness of the extensor carpai radialis brevis tendons in patients with lateral epicondylitis.
Materials and Methods
Twenty nine patients diagnosed with lateral epicondylitis were examined prospectively. Eight were male and twenty one were female. The mean age was 48 (34-62) years. The average time from the onset of symptoms until the examination was 9 (1-24) months. Eighteen patients did not show improvement in their symptoms after conservative treatment. Six underwent arthroscopic debridement and 4 underwent electric shock wave therapy. Three patients showed calcification on the simple x-ray. The thickness of the extensor carpai radialis brevis tendons on both the lesion and contralateral sides was measured and compared using ultrasonography.
Results
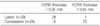
There were no significant differences in age and gender between the thickness of the extensor carpai radialis brevis tendons on the lesion and contralateral sides (p=0.83, 0.25, 0.80, 0.64). The thickness of the extensor carpai radialis brevis tendons on the lesion and contralateral sides were 4.9 mm and 3.2 mm, respectively, and the lesion side was significantly thicker (p<0.001). The best cut off value of the ECRB thickness at its origin was 3.95 mm, which had a sensitivity, specificity and accuracy of 96.6%, 79.3% and 87.9%, respectively.
Figures and Tables
Fig. 1
Receiver operation characteristic curve fitted for sonography as the reference standard. The area under the curve was 0.88 (95% CI, 0.79-0.97).

Fig. 2
A transverse image of extensor carpi radialis brevis tendon of symptomatic 49-year-old man with lateral epicondylitis is shown. The tendon of lesion (left) side is more thickened measuring 0.54 cm than contralateral (right) side measuring 0.31 cm. The ECRB origin (diamond shape area between midline of the radiocapitella joint and top of the capitellum) and scan area (black arrow, oval) for measurement are shown.

References
1. Kijowski R, De Smet AA. Magnetic resonance imaging findings in patients with medial epicondylitis. Skeletal Radiol. 2005. 34:196–202.

2. Cohen MS, Romeo AA, Hennigan SP, Gordon M. Lateral epicondylitis: anatomic relationships of the extensor tendon origins and implications for arthroscopic treatment. J Shoulder Elbow Surg. 2008. 17:954–960.

3. Levin D, Nazarian LN, Miller TT, et al. Lateral epicondylitis of the elbow: US findings. Radiology. 2005. 237:230–234.

4. Maffulli N, Regine R, Carrillo F, Capasso G, Minelli S. Tennis elbow: an ultrasonographic study in tennis players. Br J Sports Med. 1990. 24:151–155.

5. Struijs PA, Spruyt M, Assendelft WJ, van Dijk CN. The predictive value of diagnostic sonography for the effectiveness of conservative treatment of tennis elbow. AJR Am J Roentgenol. 2005. 185:1113–1118.

6. Miller TT, Shapiro MA, Schultz E, Kalish PE. Comparison of sonography and MRI for diagnosing epicondylitis. J Clin Ultrasound. 2002. 30:193–202.

8. Connell D, Burke F, Coombes P, et al. Sonographic examination of lateral epicondylitis. AJR Am J Roentgenol. 2001. 176:777–782.

9. Nirschl RP. Prevention and treatment of elbow and shoulder injuries in the tennis player. Clin Sports Med. 1988. 7:289–308.

10. Pomerance J. Radiographic analysis of lateral epicondylitis. J Shoulder Elbow Surg. 2002. 11:156–157.

11. Ohberg L, Lorentzon R, Alfredson H. Neurovascularisation in Achilles tendons with painful tendinosis but not in normal tendons: an ultrasonographic investigation. Knee Surg Sports Traumatol Arthrosc. 2001. 9:233–238.
12. Park GY, Lee SM, Lee MY. Diagnostic value of ultrasonography for clinical medial epicondylitis. Arch Phys Med Rehabil. 2008. 89:738–742.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download