Abstract
Background
Recently, various femoral head fixation devices (HFDs) for trochanteric fractures have become available. However, there are some cases in which femoral head rotation with excessive sliding of the HFD is observed and it is often followed by cutout. The purpose of this study is to compare the ability of the three types of HFDs to prevent femoral head rotation.
Methods
Between July 2005 and December 2009, 206 patients aged over 60 years with trochanteric fractures who had undergone surgical treatment using a short femoral nail in our institution were enrolled into the study. We used the gamma 3 nail (GMN) as the screw-type HFD in 66 cases, the gliding nail (GLN) as a non-cylindrical blade in 76 cases, and the proximal femoral nail antirotation (PFNA) as a cylindrical blade in 64 cases. The sliding length of HFDs and the occurrence of femoral head rotation were evaluated by assessing radiographs as the main outcome, and the results were compared among these devices.
Results
A comparison of the degree of sliding in the GMN group showed that femoral head rotation was observed significantly more frequently in cases with rotation. Further, it appeared that femoral head rotation occurred more frequently in comminuted fractures. However, no significant differences between the sliding lengths of the different HFDs were observed among three groups. Femoral head rotation was observed in 15 cases of GMN (22.7%), 0 case of GLN, and 5 case of PFNA (7.8%). Significant differences with regard to the occurrence of femoral head rotation were observed among the three groups. Furthermore, significant differences were also observed between GLN and PFNA with respect to the occurrence of femoral head rotation.
Conclusions
The ability to stabilize femoral head appears to be greater with blade-type materials than with screw-type materials. Furthermore, we believe that a non-cylindrical blade is preferable to a cylindrical blade for the surgical treatment of comminuted, unstable trochanteric fractures in order to prevent femoral head rotation and cut-out.
A rising number of trochanteric fractures associated with an increasingly elderly population have recently been reported.12) The key to a successful clinical outcome is early mobilization, allowing immediate full weight-bearing and rehabilitation.3) As stable fixation between the femoral head and femoral shaft is essential, a short intramedullary nail is the preferred choice, owing to its biomechanical and technical advantages,345) such as being less invasive and involving a shorter skin incision and less blood loss. Although intramedullary nailing has become popular for these reasons, some complications have been reported. Among these, two major complications-femoral shaft fractures and cut-out,67) which require revision surgery-are serious.
When this operation was in its infancy, a number of femoral shaft fractures were reported, especially in the USA; therefore, it was believed to be dangerous and not to be recommended. However, a modification of the technique developed in Asia and Europe, which removes the need for hammering and instruments and uses shorter and thinner nails, has decreased this complication dramatically.
However, cut-out is still a serious and unresolved complication. Previous reports have concluded that factors such as a screw positioning are the cause of this complication.8) However, in our observations, this can occur even when the screw is inserted at the optimal site. Fig. 1 shows our hypothesis that a "lack of bony support" is the most important factor involved in such complications, and we consider that the degree of sliding would be the indicator to evaluate the factor. However, orthopaedic surgeons cannot control lack of bony support because it is fixed at the point of injury and we have to accept the occurrence of excessive sliding to some extent. Therefore, we focused on the management of femoral head rotation to prevent cut-out in many cases. For this purpose, a blade has been developed to prevent femoral head fixation. There are two types of blade: a cylindrical spiral blade and a non-cylindrical H-shaped blade. The purpose of this study is to compare the capability of these three types of femoral head fixation devices with regard to the prevention of femoral head rotation. In this report, we use the term "femoral head fixation device" (HFD) as a general term to include both hip screws and various types of blades.
Between July 2005 and December 2009, 216 patients with trochanteric or basal neck fractures, transferred to our institution's emergency department, met the present study's inclusion criteria. Of these, 206 aged over 60 years were enrolled in the study. The exclusion criteria were pathological fractures, fractures associated with polytrauma, fractures associated with previous surgery on the ipsilateral femur, intracapsular femoral neck fractures, and subtrochanteric fractures. The Institutional Review Board of Takatsuki General Hospital approved the study.
We used a gamma 3 nail (GMN, Stryker, Mahwah, NJ, USA) as the screw-type HFD in 66 cases, a gliding nail (GLN, Smith & Nephew, Memphis, TN, USA) as the non-cylindrical blade in 76 cases, and a proximal femoral nail antirotation (PFNA, Synthes, Oberdorf, Switzerland) as the cylindrical blade in 64 cases (Fig. 2). The selection of HFD changed during the study: from 2005 to 2008, we used GMN and GLN, but since 2008, we have used PFNA.
When using these three implants, we generally recognized their features as follows: the GMN was developed in an attempt to overcome several problems, such as the disadvantage of the dynamic hip screw and fracture of the base of the great trochanter when nailing with a Zickel nail. GMN transmits weight closer to the calcar than the dynamic hip screw and it has greater mechanical strength.9) PFNA is preferred because some surgeons believe that the helical blade design affords rotational and angular stability to the fracture. Another advantage of PFNA is that drilling of the femoral head is not required and it can preserve bone stocks by compressing the surrounding cancellous bone when inserted.1011) GLN also has a rotationally stable blade profile but differs in having an H-shaped blade.7) In biomechanical tests, GLN showed a reduction of 50% in the transmigration rate compared with GMN and 75% in comparison with the PFN double screw.712)
All surgeries were performed under fluoroscopic closed reduction. All surgeons were well trained and were supervised by an experienced surgeon (TH, MT, and MD) to confirm and guide the procedures. The intramedullary nail was inserted from the tip of the great trochanter after reaming the medullary canal up to the minor trochanter. The HFD was inserted using the respective target device aiming at the center of the femoral head in both anteroposterior and lateral views.
In our institution, all patients start rehabilitation as soon as practicable after surgery. For example, exercises such as standing at the bedside and partial and full weight-bearing were also allowed (as far as it could be tolerated) with the assistance of a physiotherapist shortly after surgery.
The fracture type (according to Jensen's classification), operating time, degree of sliding of the HFD at two weeks postoperatively, and the occurrence of femoral head rotation were evaluated and compared among the devices (evaluated by NC, TH, and TN). With regard to the follow-up time point, serious complications such as cut-out or femoral shaft fractures tend to be observed even during the early postoperative period.13) Therefore, we decided to evaluate the degree of sliding of HFD at two weeks postoperatively for the early detection of complications.
We measured the degree of sliding of HFD (Fig. 3). If we define the HFD axis as AB, and the intersection of AB and the nail axis as C, then the central length was calculated as AC / AB × actual HFD length; the degree of sliding was calculated by subtracting the central length at two weeks postoperatively from the length just after the surgery.1415) We also assessed femoral head rotation radiologically at two weeks or more postoperatively. Femoral head rotation was confirmed by an apparent change in H': H or N': N (Fig. 4). Postoperative follow-ups were planned at two weeks post-surgery, one month after discharge from hospital, followed by monthly until six months post-surgery, and thereafter according to the estimated occurrence of bone union.
Statistical analysis was performed using the SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). For statistical evaluation, we used the chi-test and one-way analysis of variance among the three groups, and the t-test among two groups. A p < 0.05 was considered significant.
A total of 41 male and 165 female subjects, with an average age of 84.7 ± 7.3 years (mean ± standard deviation; range, 60 to 98 years) were included in this study. No significant differences were found with regard to age and gender among fracture repair devices (p > 0.05). No enrolled patients were lost to follow-up or died before 6 months. Fracture repair devices and fracture types are shown in Table 1. GLN was used predominantly for basal neck and comminuted fractures, but the distribution of bone fracture type did not differ among the three groups (p > 0.05). Mean operating time and standard deviation were 31.5 ± 12.0 minutes, 34.8 ± 12.6 minutes, and 33.3 ± 11.7 minutes for GMN, GLN, and PFNA, respectively, with no significant differences among the three groups (p > 0.05). A comparison of the degree of sliding of GMN according to whether femoral head rotation was observed showed that this was significantly higher in cases with rotation (p < 0.05) (Table 2). The mean sliding length was measured and no significant differences were noted for mean degree of sliding among the three groups (p > 0.05) (Table 3). The frequency of fracture type leading to femoral head rotation among the three groups is shown in Table 4. Significant differences were found for the occurrence of femoral head rotation in PFNA (p < 0.05) but not in GMN (p > 0.05). Femoral head rotation was observed in 15 cases of GMN (22.7%), no case of GLN (0%), and 5 cases of PFNA (7.8%). Significant differences with respect to the occurrence of femoral head rotation were observed among the three groups (p < 0.05) (Table 5). Furthermore, significant differences were observed between GLN and PFNA (p < 0.05).
There were no intraoperative complications, but three patients suffered the postoperative complication of cut-out. In two patients (one GMN and one GLN), the cause of the cut-out was falling, as opposed to natural causes. These patients were managed by total hip replacements, and the results were satisfactory. In one patient with PFNA, perforation of the blade through the femoral head occurred following a fall on the buttocks three weeks postoperatively; bipolar hip hemiarthroplasty was performed, and the results were satisfactory. No collapse or periprosthetic fractures were observed during the follow-up periods.
Although it is generally believed that cut-out of HFD occurs after poor HFD positioning,8) it can also occur in patients where the HFD is in an acceptable position within the femoral head. We previously hypothesized that in GMN, the occurrence of cut-out was dependent on fracture type; in fractures with insufficient contact between bones, an excessive degree of sliding of the HFD could occur because of the lack of bony support, followed by femoral head rotation and subsequent cut-out. In contrast, with regard to the relationship between the increased sliding of the screw and cut-out, we found insufficient evidence of this in the literature.16) We consider that an excessive degree of sliding of the HFD might lead to insufficient fixation followed by cut-out because when we examined patients treated by GMN, we discovered an excessive degree of sliding and a high level of femoral head rotation. In contrast, no significant differences were observed when we examined the degree of sliding in GMN, GLN, and PFNA. It appeared that femoral head rotation occurred more frequently in comminuted fractures. As mentioned above, we consider that the degree of sliding was influenced more or less by the type of fracture; however, as this was a patient-dependent factor, it was outside the control of the orthopaedic surgeon. Therefore, we reconsidered that the reasons for the higher incidence of femoral head rotation observed in GMN compared with the other two HFDs was not due to the degree of sliding, but to differences in the rotational stability of the HFD. With respect to the relationship between femoral head rotation and cut-out, many authors have reported the importance of femoral head rotation as the cause of cut-out.171819202122) Taking our results into consideration, we also emphasized that femoral head rotation would lead to implant cut-out. Therefore, prevention of femoral head rotation can reduce the possibility of cut-out. From this viewpoint, the single screw-type HFD was at a disadvantage because it virtually had no ability to prevent rotation. Alternatively, the use of two screws was introduced to prevent rotation of the femoral head (PFN, Synthes). However, this technique proved to be less popular because it was a relatively complex procedure and involved the loss of bone stock and an unexpected screw movement called the Z-effect,2324) and higher revision rates using PFN were reported, e.g., a cut-out rate of up to 8%.625)
Blade-type HFD is another solution for preventing femoral head rotation.26) In this study, femoral head rotation was significantly less frequent in patients with blade-type HFDs than in those with single screw-type HFDs. Strauss et al.27) reported the biomechanical superiority of a blade compared with a hip screw, and several other published reports have shown that blade-type materials provided greater resistance to cut-out than lag screw design. 2028) In addition, blade-type HFDs have the further advantage of preserving cancellous bone because they are inserted in such a way to compress the surrounding cancellous bone without reaming and have a smaller cross-section and greater contact area.729)
We used two types of blades: one cylindrical (PFNA) and the other non-cylindrical (GLN). Gehr et al.7) reported zero occurrence of cranial perforations or cut-out when GLN was used. As GLN has an H-shaped cross section at the top, but is not constricted at the base, cancellous bone is compressed at this point and protected against perforation. In our study, GLN completely prevented femoral head rotation, whereas five cases were observed with the use of PFNA. In addition, we revealed that femoral head rotation occurred more frequently in comminuted fractures (according to Jensen's classification). From these results, we suggest that blade-type materials, particularly a non-cylindrical blade such as GLN should be used for such severe fracture types to avoid the likelihood of femoral head rotation leading to cut-out.
We consider that there are three limitations to the study. First, it is a retrospective study and the choice of the three implants used was not arbitrary, and the selection of the three implants was not randomized. Second, bone mineral density was not measured as a parameter of osteoporosis in all patients; we had to exclude the data on osteoporosis despite recognizing this as an important factor in cut-out. Third, with regard to measurement of the degree of sliding, we used the methods referenced by Tsukada et al.15) However, because no report on the radiographic measurement of femoral head rotation was found to the extent we could examine, detection of this parameter was performed using our original method.14)
The ability to stabilize femoral head rotation appeared to be greater with blade-type materials than with screw-type materials. Furthermore, we believe that a non-cylindrical blade is preferable to a cylindrical blade for the surgical treatment of the comminuted, unstable trochanteric fractures to prevent femoral head rotation and cut-out.
Figures and Tables
Fig. 1
Hypothesis of the mechanism of cut-out. We hypothesized that a lack of bony support would lead to femoral head rotation and cut-out.

Fig. 2
Fixation devices. We used a gamma 3 nail as the screw-type head fixation device (A), gliding nail as the non-cylindrical blade (B), and proximal femoral nail antirotation as the cylindrical blade (C) in our study.

Fig. 3
Measurement of the sliding length of head fixation device (HFD). The sliding length was calculated by subtracting the central length (AC/AB × real HFD length) measured at two weeks after surgery from the length measured immediately after surgery. AB: HFD axis, C: intersection of AB and nail axis.

Fig. 4
Recognition of femoral head rotation. Femoral head rotation was detected by an apparent change in H': H or N':N.
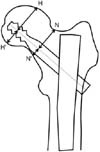
Table 1
Fixation Devices and Fracture Types (n = 206)

Table 2
Comparison of the Degree of Sliding of Gamma 3 Nail according to the Presence of Femoral Head Rotation

| Rotation | (+) | (-) | p-value |
|---|---|---|---|
| Sliding length (mm) | 8.54 (2.8 to 14.9) | 3.83 (0 to 12.8) | < 0.05 |
Table 3
Mean Sliding Length among the Three Groups
| Fixation device | GMN | GLN | PFNA | p-value |
|---|---|---|---|---|
| Sliding length (mm) | 4.40 (0 to 14.9) | 4.39 (0 to12.8) | 4.05 (0 to 11.9) | > 0.05 |
ACKNOWLEDGEMENTS
The authors would like to thank Enago (www.enago.jp) for the English language review. We also would like to thank the Central Japan Association of Orthopaedic Surgery & Traumatology for the permission to publish our manuscript in this journal. This manuscript is a revised edition of a paper published in the Central Japan Journal of Orthopaedic Surgery & Traumatology (2011;54;581-582) in Japanese. Finally, we would like to thank the Japanese Society for Fracture Repair (JSFR) for the permission to use Figure 1 in this journal. This Figure is cited from Kossetsu (2008;30;458-461) in Japanese.
References
1. Kannus P, Parkkari J, Sievanen H, Heinonen A, Vuori I, Jarvinen M. Epidemiology of hip fractures. Bone. 1996; 18:1 Suppl. 57S–63S.
2. Xu YZ, Geng DC, Mao HQ, Zhu XS, Yang HL. A comparison of the proximal femoral nail antirotation device and dynamic hip screw in the treatment of unstable pertrochanteric fracture. J Int Med Res. 2010; 38(4):1266–1275.
3. Fritz T, Weiss C, Krieglstein C, Quentmeier A. The classic nail in the therapy of trochanteric fractures: a prospective, controlled study. Arch Orthop Trauma Surg. 1999; 119(5-6):308–314.
4. Curtis MJ, Jinnah RH, Wilson V, Cunningham BW. Proximal femoral fractures: a biomechanical study to compare intramedullary and extramedullary fixation. Injury. 1994; 25(2):99–104.
5. Radford PJ, Needoff M, Webb JK. A prospective randomised comparison of the dynamic hip screw and the gamma locking nail. J Bone Joint Surg Br. 1993; 75(5):789–793.
6. Saudan M, Lubbeke A, Sadowski C, Riand N, Stern R, Hoffmeyer P. Pertrochanteric fractures: is there an advantage to an intramedullary nail?: a randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma. 2002; 16(6):386–393.
7. Gehr J, Arnold T, Hilsenbeck F, Friedl W. The gliding nail, a universal implant in the treatment of proximal femur fractures. Eur J Trauma. 2006; 32(6):562–569.
8. Baumgaertner MR, Solberg BD. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg Br. 1997; 79(6):969–971.
9. Halder SC. The Gamma nail for peritrochanteric fractures. J Bone Joint Surg Br. 1992; 74(3):340–344.
10. Zhou F, Zhang ZS, Yang H, et al. Less invasive stabilization system (LISS) versus proximal femoral nail anti-rotation (PFNA) in treating proximal femoral fractures: a prospective randomized study. J Orthop Trauma. 2012; 26(3):155–162.
11. Cheung JP, Chan CF. Cutout of proximal femoral nail antirotation resulting from blocking of the gliding mechanism during fracture collapse. J Orthop Trauma. 2011; 25(6):e51–e55.
12. Friedl W, Clausen J. Experimental examination for optimized stabilisation of trochanteric femur fractures, intra- or extramedullary implant localisation and influence of femur neck component profile on cut-out risk. Chirurg. 2001; 72(11):1344–1352.
13. Lucke M, Burghardt RD, Siebenlist S, Ganslmeier A, Stockle U. Medial migration of lag screw with intrapelvic dislocation in gamma nailing: a unique problem? A report of 2 cases. J Orthop Trauma. 2010; 24(2):e6–e11.
14. Hiranaka T, Chinzei N, Hida Y, Tsuji M. Accurate measurement of the sliding length of femoral head fixation devices of intramedullary nail for trochanteric fractures. Kossetsu. 2011; 33(3):652–654.
15. Tsukada S, Okumura G, Matsueda M. Postoperative stability on lateral radiographs in the surgical treatment of pertrochanteric hip fractures. Arch Orthop Trauma Surg. 2012; 132(6):839–846.
16. Pascarella R, Cucca G, Maresca A, et al. Methods to avoid gamma nail complications. Chir Organi Mov. 2008; 91(3):133–139.
17. De Bruijn K, den Hartog D, Tuinebreijer W, Roukema G. Reliability of predictors for screw cutout in intertrochanteric hip fractures. J Bone Joint Surg Am. 2012; 94(14):1266–1272.
18. Brown RH, Burstein AH, Frankel VH. Telemetering in vivo loads from nail plate implants. J Biomech. 1982; 15(11):815–823.
19. Bergmann G, Graichen F, Rohlmann A. Hip joint loading during walking and running, measured in two patients. J Biomech. 1993; 26(8):969–990.
20. Sommers MB, Roth C, Hall H, et al. A laboratory model to evaluate cutout resistance of implants for pertrochanteric fracture fixation. J Orthop Trauma. 2004; 18(6):361–368.
21. Ehmke LW, Fitzpatrick DC, Krieg JC, Madey SM, Bottlang M. Lag screws for hip fracture fixation: evaluation of migration resistance under simulated walking. J Orthop Res. 2005; 23(6):1329–1335.
22. Bojan AJ, Beimel C, Taglang G, Collin D, Ekholm C, Jonsson A. Critical factors in cut-out complication after Gamma Nail treatment of proximal femoral fractures. BMC Musculoskelet Disord. 2013; 14:1.

23. Brunner A, Jockel JA, Babst R. The PFNA proximal femur nail in treatment of unstable proximal femur fractures: 3 cases of postoperative perforation of the helical blade into the hip joint. J Orthop Trauma. 2008; 22(10):731–736.

24. Tyllianakis M, Panagopoulos A, Papadopoulos A, Papasimos S, Mousafiris K. Treatment of extracapsular hip fractures with the proximal femoral nail (PFN): long term results in 45 patients. Acta Orthop Belg. 2004; 70(5):444–454.
25. Al-yassari G, Langstaff RJ, Jones JW, Al-Lami M. The AO/ASIF proximal femoral nail (PFN) for the treatment of unstable trochanteric femoral fracture. Injury. 2002; 33(5):395–399.

26. Wild M, Jungbluth P, Thelen S, et al. The dynamics of proximal femoral nails: a clinical comparison between PFNA and Targon PF. Orthopedics. 2010; 33(8):DOI: 10.3928/01477447-20100625-04.

27. Strauss E, Frank J, Lee J, Kummer FJ, Tejwani N. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: a biomechanical evaluation. Injury. 2006; 37(10):984–989.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download