Trigger finger or flexor tenosynovitis is one of the most common reasons for referral to hand surgery outpatient clinics. The lifetime risk of developing trigger finger is between 2% and 3%.1)
Patients frequently present with a painful triggering or clicking during active motion of an affected digit. This is due to the loss of normal smooth gliding of the tendon beneath the pulley system, most commonly at the level of the A1 pulley. This may be as a result of a nodule in the tendon or a diffuse swelling within the sheath as a result of a tenosynovitis.
In 1953, Howard2) described the technique of steroid injection into the flexor sheath as an effective treatment. It has since become an accepted initial treatment for the condition3) largely due to its ease of use within the outpatient setting, its low complication rate and the low rate of associated morbidity.
This study investigated the efficacy of steroid injections at the level of the A1 pulley as a treatment for trigger digit. It also considered whether the efficacy of steroid injection is related to the severity of the condition at presentation, the presence of two common co-morbidities-diabetes and osteoarthritis-the presence of a nodule and the digit in which the tenosynovitis was present. The study is unique in that it uses Green's classification for the severity of the condition and it investigates the efficacy of the steroid injections in all the individual digits.
METHODS
A retrospective review of the medical records of all the patients treated for acquired trigger digit over a 3 year period between 2005 and 2008 was performed. All patients over 18 years of age were offered an injection at their initial consultation, regardless of the severity or duration of their symptoms. All patients who had previous surgery or a steroid injection for the condition in the affected digit were excluded from the study. There was a total of 90 trigger digits included in the study in 61 patients. There were 36 females and 25 males in the study, with a mean age of 62 years (range, 33 to 91 years).
The results found that the most commonly affected digit with the condition was the ring finger (28 digits) followed by the thumb (25 digits), middle finger (22 digits), little finger (8 digits) and lastly the index finger (7 digits). There were 42 patients in the study who only had a single trigger digit and 19 patients with multiple digit involvement (12 patients with two digits, 6 with three digits and 1 with six digits).
All the patients had at least a two month clinical appointment following their final treatment. An additional telephone follow up was made at least one year after their final appointment to ensure there was no recurrence of their symptoms.
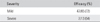
The study focused on the overall efficacy of the steroid injections for the treatment of trigger digit. It also looked at whether the efficacy was related to the severity at initial presentation. The study graded the severity of the trigger digit in accordance with Green's classification3) (Table 1). Grade I and II were then grouped as mild triggering and III and IV as severe triggering.
The trigger digits were separated into those with a nodule and those with a diffuse swelling. If the digit was clinically found to have a well defined round nodule at the level of the A1 pulley then they were designated as nodular and the remainder were classed as diffuse.
All the co-morbidities of the patients in the study were noted in order to see whether there was a correlation with the efficacy of the injections. There were 20 patients who suffered from generalised osteoarthritis, which involved any joint in the body. There were 21 with either insulin or non-insulin dependent diabetes. There were no other co-morbidities in significant numbers to warrant further investigation.
All patients were injected under aseptic conditions using 1 mL (10 mg) triamcinolone acetonide (Adcortyl, Squibb & Sons Ltd, Uxbridge, Middlesex, UK). A 26 gauge needle was used to inject the solution directly into the flexor sheath just distal to A1 pulley. The needle was inserted without ultrasound guidance at the level of the proximal digital crease, located at the base of the digit. It was advanced at a 45-degree angle and directed proximally towards the pulley. No splint was used post-injection and the patient was encouraged to use the digit.
Patients were followed up in clinic after two months. The injection was considered effective if the patient had relief from their symptoms at their follow-up appointment. They were then given an open appointment to return in the event their symptoms returned. If the patient had partial or no symptom relief they were offered a second injection followed by another two month appointment. If there was no relief after the second injection the patient was then offered either a third and final injection or an open surgical release of the pulley. After three failed injections without benefit, patients were then encouraged to pursue surgical management.
RESULTS
The study found the total efficacy for steroid injections to be 66% (59/90). There was a 34% success rate with the first injection (31/90). This rose to 63% (57/90) with the second injection and 66% (59/90) with the third injection (Fig. 1). This is the cumulative success rate of the injections.
Surgery in the form of an open release of the A1 pulley was performed on a total of 26 digits, whilst four patients had no relief of their symptoms after three injections but refused surgery in light of their poor health or personal reasons.
The success of the injection varied depending on the digit being injected. The thumb was found to have the best response to the steroid injections, with a success rate of 23/25 (92%). This was followed by the ring, index, middle and lastly the little finger (Fig. 2). There was a statistically significant difference in the efficacy between the thumb and the fingers in accordance with the Fisher exact test (p = 0.001).
The study showed that the presence of a palpable nodule reduced the success rate of the steroid injection. The efficacy was found to be 18/33 (55%) with a nodule compared with a success rate of 41/57 (72%) in digits with a diffuse pattern (Fig. 3). This finding was however not statistically significant (chi squared = 2.797 with one degree of freedom, p = 0.0944).
Grading of the severity of the triggering was done using Green's classification.3) In order to increase the sample sizes grade I and II were classed as mild triggering and III and IV as severe. The success of the injection with mild triggering was 47/65 (72%), compared with 7/13 (54%) for severe triggering (Table 2). Some of the digits were not properly classified in the notes and were therefore omitted from the study. Even though there seems to be an observed reduction in the success in the different severities, there is no statistical difference using Fisher's exact test (p = 0.323).
The study found an increased efficacy of the steroid injections in those who only suffered from a single digit compared to those with multiple digit involvement. The steroid injections were effective in 32/42 single digits (76%) compared with 27/48 digits (56%) with multiple digit involvement. The efficacy appears to be improved in the presence of a single digit; however it is not considered to be statistically significant (Fisher's exact test: p = 0.0745).
The presence of two common co-morbidities was recorded and the efficacy of the treatment with steroid injections was analysed. It was found that there was a success rate of 12/20 (60%) in patients that suffered from osteoarthritis and a rate of 12/21 (57%) in those with diabetes (Fig. 4). The efficacy appears lower in the presence of both co-morbidities, however there is no statistical significance. (Fischer-Freeman-Halt's exact test p = 0.5992 in osteoarthritis and p = 0.6065 in diabetes).
In this study there were no complications encountered through the injections of steroids.
DISCUSSION
Steroid injections have an established role as the first line treatment for trigger digit, as they are safe, easy to administer and cost-effective.4) Surgical release of a trigger digit has a reported success rate of between 60%5) and 97%.6) Unfortunately, surgery is associated with complications such as infection, nerve injury, tendon laceration, long-standing pain, contracture of the proximal interphalangeal joint and recurrence.7) A study by Thorpe5) in 1988 reported a total complication rate of 28% after surgery. It remains however the definitive treatment for patients who have no response to steroid injections or who have recurred following two or three steroid injections.
Steroid injections have been found to be effective in the treatment of trigger digit. Its efficacy varies from between 67 and 90%.8-11) This study shows a slightly lower total efficacy of 66% with no reported complications.
This study has found that steroids can be administered safely up to three times in the same digit. However, the study showed that the third injection only increased the overall efficacy by 2% (Fig. 1). Only those patients who had at least a partial response were offered a third injection.
A recent study from the United States found that two steroid injections followed by open surgery was the most cost-effective algorithm to follow. The study also found that if the success rate of the third injection was found to be greater than 9%, then three injections followed by surgery would be more cost effective.4)
There was a significant difference in the efficacy of the injections in the different digits. The highest success rate was clearly seen in the thumb, with a success rate of 92%. The study found a statistical difference in the success of the steroids in the thumb compared with the fingers. This is similar to what was found in Marks and Gunther's study in 1989.12) The increased efficacy in the thumb could be due to the anatomical difference in its flexor tendon pulley system; alternatively it could be due to the placement of the steroid injection, as by using the described technique the needle is inserted closer to the nodule in the thumb than in the other digits.
The study found no correlation between the presence of a nodule and the efficacy of steroid injections. Freiberg et al.13) in 1989 found that the clinical distinction between nodular and diffuse trigger digits greatly influences the success of the steroid injection. They found that 93% of patients with nodules were relieved of their symptoms after a single injection compared with 48% of patients with a diffuse trigger finger pattern. This study suggests the opposite, with a 56% success rate with a nodule compared with 72% without. However, there was no statistical difference between the two types.
There is limited literature on whether the efficacy of the injections is related to the severity of the disease at presentation. Kazuki et al.7) in 2006 found that fewer injections were needed for mild symptoms, but used their own classification rather than a recognised classification. This study found an observed reduction in the efficacy with severe triggering; however the sample size was not large enough to statistically show a difference. The study also found an increased efficacy in patients with single digit involvement compared to multiple digits; however no statistical difference could be shown.
Studies have found an association between trigger digit and other conditions, such as carpal tunnel syndrome,14) de Quervain's,15) rheumatoid arthritis, osteoarthritis,16) hypothyroidism,9) and diabetes mellitus.17) However, there is little research into whether the conditions have a relationship with the efficacy of the injections. The exception is diabetes, where there is shown to be a reduced efficacy.17) In this study there were 21 patients with diabetes and 20 with generalised osteoarthritis. The success of the injections was found to be reduced in both diabetics (12/21) and osteoarthritis (12/20). Studies have shown that diabetics with trigger digits are more difficult to treat, are more likely to develop triggering in other digits and are more likely to require open surgery, which is turn is more likely to fail. Diabetics are thought to have a poor microvascular tissue bed and hence an abnormal cellular response to the steroid injection.17)
No complications were reported in this study after the administration of the steroids into the pulley. A review of 11 studies on steroid injections for trigger finger revealed no serious adverse side effects in 1,246 digits.18) However there have been reports of hypopigmentation of the skin,19) tendon rupture,20,21) digital necrosis18) and fat atrophy at the injection site.22) This stresses the importance of properly administering the steroids into the sheath.
In conclusion, steroid injection is a successful first-line intervention for the treatment of trigger digit, especially in the thumb. The total efficacy of the steroid injections was 66% in the study. There was statistically a greater success of the injections in treating the thumb compared with other fingers. The severity of the condition at presentation, the presence of a nodule at the site and osteoarthritis or diabetes all reduced the efficacy of the steroid injection. However the study was not large enough to demonstrate a statistically significant difference between these variables.
The efficacy of a third steroid injection needs to be investigated in a larger study, but the findings of this study suggest that a third injection does not substantially increase the efficacy of the treatment. It is therefore recommended that after two steroid injections the patient with recurrent symptoms is offered a surgical or percutaneous release of the triggering digit.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download