Abstract
Background
Mucoid degeneration of the anterior cruciate ligament is a rare pathological entity. Several authors have identified this condition, described their experiences, and suggested their own guidelines for management. The aim of this study was to detail the clinical, radiological, arthroscopic, and pathological findings of mucoid degeneration of the anterior cruciate ligament and report the clinical outcomes following arthroscopic treatment.
Methods
A historical cohort of patients who underwent arthroscopic total or partial excision of the anterior cruciate ligament due to mucoid degeneration between 2011 and 2014 were reviewed. The minimum follow-up was 3 years. Demographic, radiological, and histological findings, type of surgery, and clinical pre- and postoperative data were analyzed. The visual analogue scale score, the International Knee Documentation Committee score, and the Tegner Lysholm Knee Score were collected preoperatively, postoperatively, and during the follow-up period.
Results
Seventeen females (67%) and eight males (33%) were included in the final analysis. The mean age at the time of surgery was 57 years (range, 31 to 78 years). Partial resection of the anterior cruciate ligament was done in seven cases and a complete resection in 18 cases. No reconstruction was performed at the same time. A positive Lachman test and a negative pivot shift were noted after surgery in all cases. Anterior cruciate ligament reconstruction was required in only one young patient due to disabling instability. At last follow-up, the mean visual analogue scale score, International Knee Documentation Committee score, and Tegner Lysholm Knee score improved (p < 0.01).
Conclusions
Our study provides further evidence that arthroscopic total or partial excision of anterior cruciate ligament is a safe and effective treatment for mucoid degeneration of the anterior cruciate ligament, improving patient satisfaction and function without causing clinical instability in daily activities. However, young patients should be forewarned about the risk of instability, and an anterior cruciate ligament reconstruction could be necessary.
Mucoid degeneration (MD) of the anterior cruciate ligament (ACL) is a rare pathological entity that has been found in patients with pain and limited range of motion of the knee in association with a bulky ACL shown on magnetic resonance imaging (MRI).1) However, this association is not sufficient to establish an accurate diagnosis, as its presentation and appearance can mimic other pathologies such as partial ACL tears, ganglion cysts, and synovial chondromatosis.2) The prevalence of ACL MD on MRI has been reported to range from 1.8% to 5.3%; nevertheless, not all the lesions are symptomatic.3)
This pathology characterized by infiltration of mucoid-like substance (glycosaminoglycans) interspersed within the substance of ACL was first described by Kumar et al.4) in 1999. Since then, many entities have been described in relation to this pathology with different names. Kumar et al.4) referred to the condition as mucoid cystic degeneration of the ACL. Kim et al.1) named this lesion as mucoid hypertrophy. Bergin et al.3) specifically used the term, MD. One of the explanations for the disagreement on nosology of mucoid pathology of the ACL is the lack of available patients for studies. It is a rare condition not well known by physicians and thus clinically underdiagnosed or confused with ACL tears.56) For such reasons, most previous literatures are case reports.
Several authors have identified this condition, described their experiences, and suggested their own guidelines for management.127891011121314151617) The aim of this study was to detail the clinical, radiological, arthroscopic, and pathological findings of this condition and report the clinical outcomes following arthroscopic treatment of MD of the ACL. Based on previous reports in the literature, our hypothesis was that partial or total ACL resection would improve pain, symptoms, and range motion at the expense of residual anterior laxity that would not necessitate additional treatment. Furthermore, a review of the literature of this disease and its surgical treatment has been performed.
A historical cohort study was performed. Institutional Review Board approval was obtained to retrospectively review patients who had undergone surgery because of MD of the ACL between 2011 and 2014 (IRB No. ID-RTF065). Patients were identified through our institutional registry. The inclusion criteria were patients who had arthroscopic total or partial excision of the ACL with a minimum follow-up of 3 years. Diagnosis in all patients was done based on clinical, MRI, arthroscopic, and histological findings. Patients with open surgery, incomplete clinical history or MRI performed in other hospital were excluded. MRI and arthroscopic findings were described in agreement with previous studies (Table 1).16)
Patients were treated initially with nonsteroidal anti-inflammatory drugs and physiotherapy for a minimum of 6 months before considering surgery. Physiotherapy was an aerobic exercise program that included range of motion and strengthening exercises.
A single team of knee orthopedic surgery specialists (JHN, NJJ, EC, JM) performed all surgeries. During surgery, all compartments were explored to evaluate the state of menisci, ligaments, and cartilage. Arthroscopic treatment consisted of a total or partial excision of the ACL with a motorized shaver. Previously, a sample of the degenerated part of the ACL was taken for histological study. The hypertrophied ACL was excised as needed to achieve impingement-free motion between the ACL and the intercondylar notch. Partial or total excision was determined based on the surgical criteria and previous experience of the surgeon. If a meniscal tear was found, they were treated at the same time during surgery. Notchplasty was not performed in any case.
Postoperatively, patients started rapid mobilization of the knee and immediate weight bearing according to pain tolerance. Excised materials were stained with hematoxylin and eosin and Alcian blue and were examined by light microscopy.
Demographic and clinical data including the patient's age at the time of surgery, sex, the presenting symptoms, range of motion, and ligament instability assessed using the Lachman test and the pivot-shift test were collected. In addition, the visual analogue scale (VAS) score, the International Knee Documentation Committee (IKDC) score, and the Tegner Lysholm Knee Score were collected preoperatively, postoperatively, and during the follow-up period (1, 3, 6, and 12 months postoperatively and every year thereafter). The latest data from each patient were used for analysis. All scores were measured by the same observer (DV). MRI analysis included measurement of the thickness of the ACL, measurement of the middle intercondylar space, the presence of bone edema, intraosseous and soft tissue cysts, and presence of concomitant MD of the posterior cruciate ligament. All MRI findings were reported and measured by a single expert radiologist (RDO) in musculoskeletal pathology.
Among the 37 patients, only 25 patients met our inclusion criteria and were available for analysis. There were 17 females (67%) and eight males (33%) with a mean age of 57 years (range, 31 to 78 years) at the time of surgery. The mean follow-up was 53 months (range, 37 to 64 months). All of the patients presented with knee pain, which was exacerbated by flexion. In 75% of the cases, the pain was located in the posterior region of the knee. At the preoperative examination, the range of motion ranged from 0° to 120°. All patients had restricted flexion. Extension deficits were found in four patients. All patients had a stable knee with negative Lachman and pivot shift tests.
All MRIs showed a bulky ACL, occupying almost the entire intercondylar notch, with a marked increase in signal, particularly in the T2-weighted images, and with a mass-like configuration intertwined with its fibers with “celery stalk” sign (Fig. 1). Continuity of the ligament and the preservation of its insertions and orientation of the fibers were always observed. The mean ACL thickness in the sagittal cut was 14.2 mm (range, 7 to 19 mm), and the mean intercondylar space in the axial section was 19.8 mm (range, 6 to 24 mm). Fifty-two percent had a distal femoral or a proximal tibia edema and 68% presented with intraosseous and soft tissue cysts. Twelve percent had a concomitant MD of the posterior cruciate ligament (Table 2). In all cases, histology revealed loss of hyaline fibrocollagenous tissue, many MD vesicles, and positive Alcian blue stain.
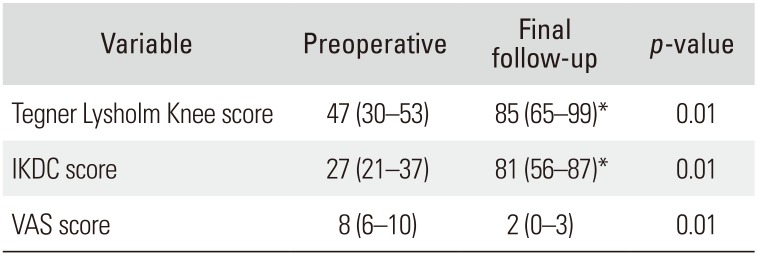
Partial ACL resection was done in seven cases and complete resection in 18 cases (Fig. 2). Eight patients had meniscal tears; in these patients, meniscectomy was also performed (Table 2). No ACL reconstruction was performed at the same time. A positive Lachman test and a negative pivot shift test were noted after surgery in all cases. ACL reconstruction was required in only one young patient due to disabling instability. At last follow-up, 22 patients were pain-free. The mean knee flexion increased by 23.32°. All clinical scores (Tegner Lysholm Knee, IKDC, and VAS) improved with statistical significance (p < 0.01) (Table 3).
MD of the ACL, until now, has been a rare pathological entity because it has been underdiagnosed and confused with other pathologies.1) It is characterized by infiltration of mucoid-like substance (glycosaminoglycans) interspersed within the substance of ACL causing pain and limited motion of the knee.2) It seems that not only clinical examination and MRI are necessary for diagnosis, but histology helps in its detection. The differential diagnosis must be done above all with the ACL ganglion cyst. Both lesions of ACL are two different entities that occasionally coexist.18) The aim of this study was to detail the clinical, radiological, arthroscopic and pathological findings of this condition and report the clinical outcomes following arthroscopic treatment of MD of the ACL.
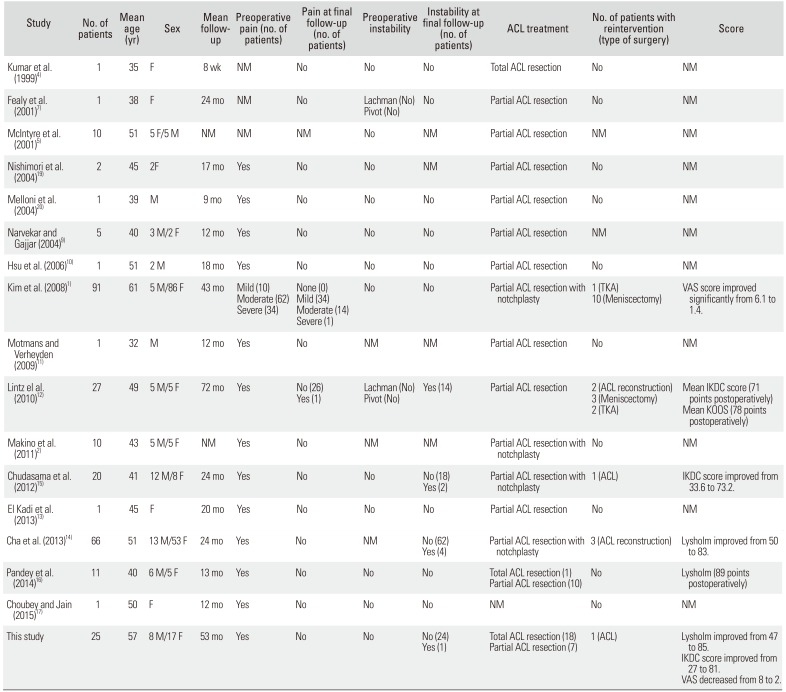
A review of the literature on the subject reveals many clinical cases and short heterogeneous series (Table 4).12457910111213141516171920) As noted in previous reports, clinical symptoms of MD of the ACL include nonspecific knee pain with limitation of the range movement and ligament stability.79181920) None of our patients knew precisely when their symptoms started, but all had persistent knee pain in terminal flexion for at least 12 months, which was distinct from acute extension pain caused by meniscus bucket-handle tears. The fact that our patients did not have a trauma prior to the onset of knee pain and their symptoms did not respond to nonsteroidal anti-inflammatory drugs and physiotherapy helped us to suspect MD of the ACL. MRI and arthroscopic findings in our patients also agree with previous studies.16)
Arthroscopic total and partial excision of MD of the ACL, combined with or without notchplasty, has been found to result in pain relief and improve in the range of motion of the knee. In our study, we performed 18 complete resections and seven partial resections of the ACL. After surgery, we noticed that flexion deficits improved during the postoperative period. The mean knee motion increased by 23.32°. Though all patients regained full flexion after debulking of the mucinous ACL, some of them continued to experience mild pain while walking or climbing stairs. This could be explained probably by the presence of concomitant lesions, such as cartilage damage or meniscal tears. Kwee et al.21) demonstrated a strong association between ACL MD and cartilage damage, especially in patients > 50 years. Some authors also reported that associated meniscal tears and chondral damage suggest that MC of the ACL may be part of an overall degenerative process.22) In our study, we performed meniscectomy in eight patients. Although they were not pain-free at the final follow-up, we found decreases in pain score (VAS score decreased by a mean of 6 points) improvement in clinical scores (IKDC improved by a mean of 54 points and Lysholm improved by a mean of 38 points). These values are important because most of the studies have not included clinical scores in the postoperative evaluation. To our knowledge, only two studies have evaluated pre- and postoperative values.1415)
Our study differs from other studies because in most of the studies MD was treated by partial debridement of the ACL, whereas in our study only 28% of the cases were treated by partial debridement.1114) The issue of instability after ACL resection is subject to debate; only one study published used a systematic Lachman test and Telos dynamic radiographs postoperatively to assess ACL function after MD resection. In that study, 93% of patients had a postoperative anterior laxity and two patients needed a subsequent ACL reconstruction.12) Unfortunately, the authors did not clarify whether these two patients had developed instability due to chronic stretching after partial resection or due to subtotal or total resection of the mucoid ACL. Most authors believe that debridement of mucinous substance with partial ACL debulking is the safest therapeutic option.1114) However, at first, we agreed with Kumar et al.4) who suggested that total removal of the ACL is a safe treatment option that would not result in instability. We performed 18 complete ACL resections, of whom only one young patient complained of instability and underwent an ACL reconstruction 2 years after primary surgery. This may also be due to the higher mean age of our patients than that in previous series reported. Filbay et al.23) in their meta-analysis identified no significant differences in knee-related quality of life (QOL) between ACL-deficient and ACL-reconstructed groups. They also identified that the average health-related QOL scores in ACL-deficient people were similar to those reported in a general population but impaired compared to more active populations. We consider that if a total removal of the ACL is done in a young active patient, an ACL reconstruction should be done at the same time.619) Nowadays, although we performed 18 complete ACL resections and obtained good results, we agree with the current literature that recommends debulking of the lesion without compromising the integrity of the ACL.18)
An additional notchplasty is considered essential by some authors. Nevertheless, Motmans and Verheyden11) specifically mentioned that notchplasty is not required because thorough debridement of the ACL by itself resolves impingement and thereby the pathology. In our study, we did not perform any notchplasty. Lintz et al.612) performed two notchplasties out of 29 patients but not routinely. We performed a resection or meticulous debridement of the mucoid ACL with the aim of reducing the volume, achieving removal of the mucoid mass and decompression of the bulky pathological ACL. We believe that notchplasty may be needed in some cases where notch is quite stenotic and impinged by osteophytes especially in elderly patients. However, it may not be needed in middle-aged patients where notch is free of osteophytes.
One of the limitations of this study is the small sample size; however, the minimum follow-up was 3 years. In comparison, in a study of Kim et al.1) that included the largest cohort of patients with this pathology (91 cases), the inclusion criterion was only based on clinical and MRI findings without histological pathology, and the follow-up period was only 2 years. Moreover, in others studies, biopsy was not done in all patients.1415) In our study, we included relatively less patients because we only analyzed patients in whom diagnosis was made based on clinical, MRI, arthroscopic, and histological findings. Also, patients with MRI performed in other hospital were excluded. Another limitation is the lack of comparison between groups. Although we performed both partial and total debridements of the ACL because of the small size of the sample, we were unable to determine statistical significance. A multicenter long-term follow-up of patients will determine whether judicious debulking of the ACL is safe and sufficient or there is a need for complete removal of the ACL with or without reconstruction.
In summary, MD should be considered in the differential diagnosis of chronic nonspecific knee pain and stiffness of non-specific etiology. Our study provides further evidence that arthroscopic total or partial excision of the ACL is a safe and effective treatment for MD of the ACL, improving patient satisfaction and function without causing clinical instability in daily activities. However, young patients should be forewarned about this risk and ACL reconstruction may be necessary.
ACKNOWLEDGEMENTS
We would like to thank Rosa Dominguez-Oronoz, Department of Radiology, University Hospital of Vall d'Hebron, Barcelona, Spain. She is the radiologist who analyzed all knee magnetic resonance images of the patients included in our study.
References
1. Kim TH, Lee DH, Lee SH, Kim JM, Kim CW, Bin SI. Arthroscopic treatment of mucoid hypertrophy of the anterior cruciate ligament. Arthroscopy. 2008; 24(6):642–649. PMID: 18514107.

2. Makino A, Pascual-Garrido C, Rolon A, Isola M, Muscolo DL. Mucoid degeneration of the anterior cruciate ligament: MRI, clinical, intraoperative, and histological findings. Knee Surg Sports Traumatol Arthrosc. 2011; 19(3):408–411. PMID: 20811733.

3. Bergin D, Morrison WB, Carrino JA, Nallamshetty SN, Bartolozzi AR. Anterior cruciate ligament ganglia and mucoid degeneration: coexistence and clinical correlation. AJR Am J Roentgenol. 2004; 182(5):1283–1287. PMID: 15100133.
4. Kumar A, Bickerstaff DR, Grimwood JS, Suvarna SK. Mucoid cystic degeneration of the cruciate ligament. J Bone Joint Surg Br. 1999; 81(2):304–305. PMID: 10204939.

5. McIntyre J, Moelleken S, Tirman P. Mucoid degeneration of the anterior cruciate ligament mistaken for ligamentous tears. Skeletal Radiol. 2001; 30(6):312–315. PMID: 11465770.

6. Lintz F, Pujol N, Boisrenoult P, Bargoin K, Beaufils P, Dejour D. Anterior cruciate ligament mucoid degeneration: a review of the literature and management guidelines. Knee Surg Sports Traumatol Arthrosc. 2011; 19(8):1326–1333. PMID: 21331652.

7. Fealy S, Kenter K, Dines JS, Warren RF. Mucoid degeneration of the anterior cruciate ligament. Arthroscopy. 2001; 17(9):E37. PMID: 11694941.

8. Lancaster TF, Kirby AB, Beall DP, Wolff JD, Wu DH. Mucoid degeneration of the anterior cruciate ligament: a case report. J Okla State Med Assoc. 2004; 97(8):326–328. PMID: 15490857.
9. Narvekar A, Gajjar S. Mucoid degeneration of the anterior cruciate ligament. Arthroscopy. 2004; 20(2):141–146. PMID: 14760345.

10. Hsu CJ, Wang SC, Fong YC, Huang CY, Chiang IP, Hsu HC. Mucoid degeneration of the anterior cruciate ligament. J Chin Med Assoc. 2006; 69(9):449–452. PMID: 17051758.

11. Motmans R, Verheyden F. Mucoid degeneration of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2009; 17(7):737–740. PMID: 19089409.

12. Lintz F, Pujol N, Dejour D, Boisrenoult P, Beaufils P. Anterior cruciate ligament mucoid degeneration: selecting the best treatment option. Orthop Traumatol Surg Res. 2010; 96(4):400–406. PMID: 20452850.

13. el Kadi KI, Marcaillou F, Blanc S, Salloum B, Dimontagliari C, Boutayeb F. Mucoid degeneration of the anterior cruciate ligament: a case report. Pan Afr Med J. 2013; 15:59. PMID: 24147185.

14. Cha JR, Lee CC, Cho SD, Youm YS, Jung KH. Symptomatic mucoid degeneration of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2013; 21(3):658–663. PMID: 22527411.

15. Chudasama CH, Chudasama VC, Prabhakar MM. Arthroscopic management of mucoid degeneration of anterior cruciate ligament. Indian J Orthop. 2012; 46(5):561–565. PMID: 23162150.
16. Pandey V, Suman C, Sharma S, Rao SP, Kiran Acharya K, Sambaji C. Mucoid degeneration of the anterior cruciate ligament: management and outcome. Indian J Orthop. 2014; 48(2):197–202. PMID: 24741143.

17. Choubey R, Jain A. Mucoid degeneration of the anterior cruciate ligament: a case report and review of literature. J Orthop Case Rep. 2015; 5(3):87–89. PMID: 27299081.
18. Vaishya R, Esin Issa A, Agarwal AK, Vijay V. Anterior cruciate ligament ganglion cyst and mucoid degeneration: a review. Cureus. 2017; 9(9):e1682. PMID: 29152439.

19. Nishimori M, Sumen Y, Sakaridani K. Mucoid degeneration of the anterior cruciate ligament: a report of two cases. Magn Reson Imaging. 2004; 22(9):1325–1328. PMID: 15607106.
20. Melloni P, Valls R, Yuguero M, Saez A. Mucoid degeneration of the anterior cruciate ligament with erosion of the lateral femoral condyle. Skeletal Radiol. 2004; 33(6):359–362. PMID: 14997351.

21. Kwee RM, Ahlawat S, Kompel AJ, et al. Association of mucoid degeneration of anterior cruciate ligament with knee meniscal and cartilage damage. Osteoarthritis Cartilage. 2015; 23(9):1543–1550. PMID: 25907861.

22. Fernandes JL, Viana SL, Mendonca JL, et al. Mucoid degeneration of the anterior cruciate ligament: magnetic resonance imaging findings of an underdiagnosed entity. Acta Radiol. 2008; 49(1):75–79. PMID: 18210315.

23. Filbay SR, Culvenor AG, Ackerman IN, Russell TG, Crossley KM. Quality of life in anterior cruciate ligament-deficient individuals: a systematic review and meta-analysis. Br J Sports Med. 2015; 49(16):1033–1041. PMID: 26224582.

Fig. 1
Preoperative magnetic resonance imaging (MRI) scan. Sagittal T2-weighted MRI view showing intact anterior cruciate ligament fibers with mucoid degeneration.
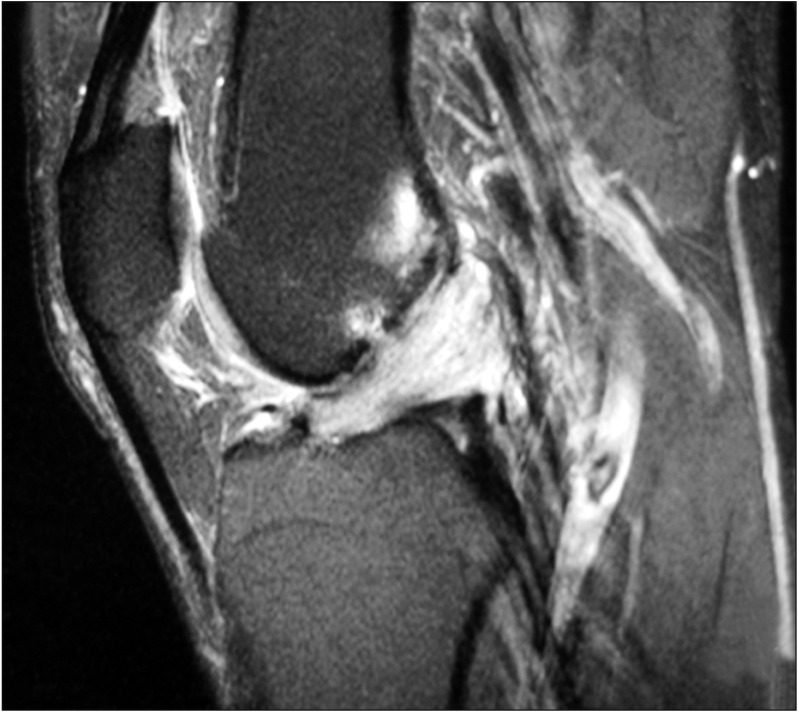
Fig. 2
Arthroscopic findings. (A) Bulging of the hypertrophied anterior cruciate ligament. (B) Partial resection (anteromedial bundle) of the anterior cruciate ligament.

Table 1
MRI and Arthroscopic Criteria for the Diagnosis of Mucoid Degeneration of the ACL
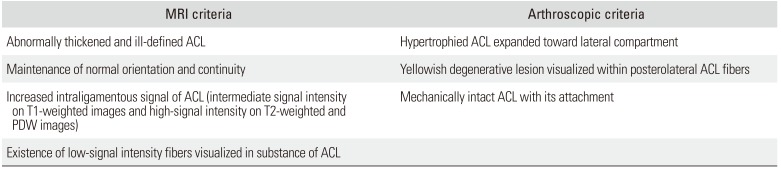
Table 2
Lesions Associated with Anterior Cruciate Ligament MD Observed on Arthroscopy and MRI
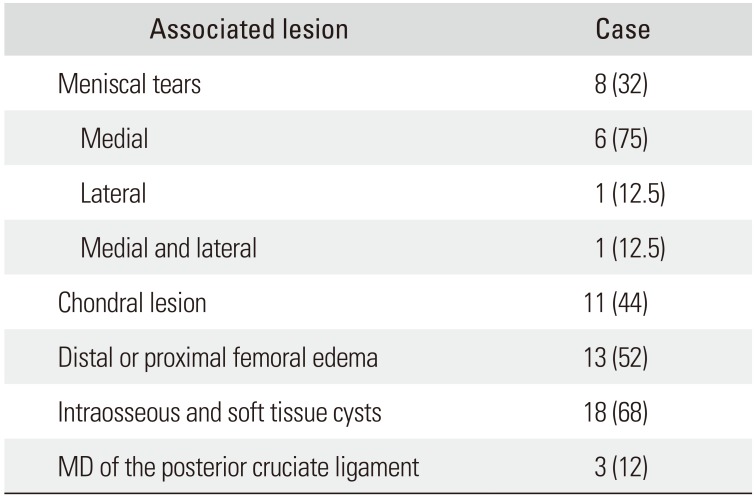
Table 3
Preoperative and Final Follow-up Outcome Scores
| Variable | Preoperative | Final follow-up | p-value |
|---|---|---|---|
| Tegner Lysholm Knee score | 47 (30–53) | 85 (65–99)* | 0.01 |
| IKDC score | 27 (21–37) | 81 (56–87)* | 0.01 |
| VAS score | 8 (6–10) | 2 (0–3) | 0.01 |
Table 4
Summary of Patients with Arthroscopic Treatment of Mucoid Degeneration of the ACL
| Study | No. of patients | Mean age (yr) | Sex | Mean follow-up | Preoperative pain (no. of patients) | Pain at final follow-up (no. of patients) | Preoperative instability | Instability at final follow-up (no. of patients) | ACL treatment | No. of patients with reintervention (type of surgery) | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Kumar et al. (1999)4) | 1 | 35 | F | 8 wk | NM | No | No | No | Total ACL resection | No | NM |
| Fealy et al. (2001)7) | 1 | 38 | F | 24 mo | NM | No |
Lachman (No) Pivot (No) |
No | Partial ACL resection | No | NM |
| McIntyre et al. (2001)5) | 10 | 51 | 5 F/5 M | NM | NM | NM | No | NM | Partial ACL resection | NM | NM |
| Nishimori et al. (2004)19) | 2 | 45 | 2F | 17 mo | Yes | No | No | NM | Partial ACL resection | No | NM |
| Melloni et al. (2004)20) | 1 | 39 | M | 9 mo | Yes | No | No | No | Partial ACL resection | No | NM |
| Narvekar and Gajjar (2004)9) | 5 | 40 | 3 M/2 F | 12 mo | Yes | No | No | No | Partial ACL resection | NM | NM |
| Hsu et al. (2006)10) | 1 | 51 | 2 M | 18 mo | Yes | No | No | No | Partial ACL resection | No | NM |
| Kim et al. (2008)1) | 91 | 61 | 5 M/86 F | 1 |
Mild (10) Moderate (62) Severe (34) |
None (0) Mild (34) Moderate (14) Severe (1) |
No | No | Partial ACL resection with notchplasty |
1 (TKA) 10 (Meniscectomy) |
VAS score improved significantly from 6.1 to 1.4. |
| Motmans and Verheyden (2009)11) | 1 | 32 | M | 12 mo | Yes | No | NM | NM | Partial ACL resection | No | NM |
| Lintz el al. (2010)12) | 27 | 49 | 5 M/5 F | 72 mo | Yes |
No (26) Yes (1) |
Lachman (No) Pivot (No) |
Yes (14) | Partial ACL resection |
2 (ACL reconstruction) 3 (Meniscectomy) 2 (TKA) |
Mean IKDC score (71 points postoperatively) Mean KOOS (78 points postoperatively) |
| Makino et al. (2011)2) | 10 | 43 | 5 M/5 F | NM | Yes | No | NM | NM | Partial ACL resection with notchplasty | No | NM |
| Chudasama et al. (2012)15) | 20 | 41 | 12 M/8 F | 24 mo | Yes | No | No |
No (18) Yes (2) |
Partial ACL resection with notchplasty | 1 (ACL) | IKDC score improved from 33.6 to 73.2. |
| El Kadi et al. (2013)13) | 1 | 45 | F | 20 mo | Yes | No | No | No | Partial ACL resection | No | NM |
| Cha et al. (2013)14) | 66 | 51 | 13 M/53 F | 24 mo | Yes | No | NM |
No (62) Yes (4) |
Partial ACL resection with notchplasty | 3 (ACL reconstruction) | Lysholm improved from 50 to 83. |
| Pandey et al. (2014)16) | 11 | 40 | 6 M/5 F | 13 mo | Yes | No | No | No |
Total ACL resection (1) Partial ACL resection (10) |
No | Lysholm (89 points postoperatively) |
| Choubey and Jain (2015)17) | 1 | 50 | F | 12 mo | Yes | No | No | No | NM | No | NM |
| This study | 25 | 57 | 8 M/17 F | 53 mo | Yes | No | No |
No (24) Yes (1) |
Total ACL resection (18) Partial ACL resection (7) |
1 (ACL) |
Lysholm improved from 47 to 85. IKDC score improved from 27 to 81. VAS decreased from 8 to 2. |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download