1. Grabenbauer GG. Internal mammary nodes in invasive breast carcinoma. To treat or not to treat? Strahlenther Onkol. 2004. 180:690–694.

2. Arriagada R, Lê MG, Mouriesse H, Fontaine F, Dewar J, Rochard F, et al. Long-term effect of internal mammary chain treatment. Results of a multivariate analysis of 1,195 patients with operable breast cancer and positive axillary nodes. Radiother Oncol. 1988. 11:213–222.

3. Overgaard M, Hansen PS, Overgaard J, Rose C, Andersson M, Bach F, et al. Danish Breast Cancer Cooperative Group 82b Trial. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. N Engl J Med. 1997. 337:949–955.

4. Overgaard M, Jensen MB, Overgaard J, Hansen PS, Rose C, Andersson M, et al. Postoperative radiotherapy in high-risk postmenopausal breast-cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomised trial. Lancet. 1999. 353:1641–1648.

5. Chargari C, Castadot P, Macdermed D, Vandekerkhove C, Bourgois N, Van Houtte P, et al. Internal mammary lymph node irradiation contributes to heart dose in breast cancer. Med Dosim. 2010. 35:163–168.

6. Taghian A, Jagsi R, Makris A, Goldberg S, Ceilley E, Grignon L, et al. Results of a survey regarding irradiation of internal mammary chain in patients with breast cancer: practice is culture driven rather than evidence based. Int J Radiat Oncol Biol Phys. 2004. 60:706–714.

7. Keum KC, Shim SJ, Lee IJ, Park W, Lee SW, Shin HS, et al. The 1998, 1999 patterns of care study for breast irradiation after mastectomy in Korea. J Korean Soc Ther Radiol Oncol. 2007. 25:7–15.

8. Poortmans P, Kouloulias VE, Venselaar JL, Struikmans H, Davis JB, Huyskens D, et al. Quality assurance of EORTC trial 22922/10925 investigating the role of internal mammary: medial supraclavicular irradiation in stage I-III breast cancer: the individual case review. Eur J Cancer. 2003. 39:2035–2042.

9. Olivotto IA, Chua B, Elliott EA, Parda DS, Pierce LJ, Shepherd L, et al. A clinical trial of breast radiation therapy versus breast plus regional radiation therapy in early-stage breast cancer: the MA20 trial. Clin Breast Cancer. 2003. 4:361–363.

10. Whelan TJ, Oivotto I, Ackerman I, Chapman JW, Chua B, Nabid A, et al. NCIC-CTG MA. 20: an intergroup trial of regional nodal irradiation in early breast cancer. 2011. 29:In : 2011 American Society Clinical Oncology Annual Meeting; Abstract #LBA1003.

11. Matzinger O, Heimsoth I, Poortmans P, Collette L, Struikmans H, Van Den Bogaert W, et al. Toxicity at three years with and without irradiation of the internal mammary and medial supraclavicular lymph node chain in stage I to III breast cancer (EORTC trial 22922/10925). Acta Oncol. 2010. 49:24–34.

12. Hurkmans CW, Saarnak AE, Pieters BR, Borger JH, Bruinvis IA. An improved technique for breast cancer irradiation including the locoregional lymph nodes. Int J Radiat Oncol Biol Phys. 2000. 47:1421–1429.

13. Arthur DW, Arnfield MR, Warwicke LA, Morris MM, Zwicker RD. Internal mammary node coverage: an investigation of presently accepted techniques. Int J Radiat Oncol Biol Phys. 2000. 48:139–146.
14. Pierce LJ, Butler JB, Martel MK, Normolle DP, Koelling T, Marsh RB, et al. Postmastectomy radiotherapy of the chest wall: dosimetric comparison of common techniques. Int J Radiat Oncol Biol Phys. 2002. 52:1220–1230.
15. Allen SJ, Klein EE, Michaletz-Lorenz M, Jin JY. Comparison of two treatment techniques for breast irradiation including internal mammary nodes. Med Dosim. 2004. 29:124–127.
16. Sonnik D, Selvaraj RN, Faul C, Gerszten K, Heron DE, King GC. Treatment techniques for 3D conformal radiation to breast and chest wall including the internal mammary chain. Med Dosim. 2007. 32:7–12.
17. Koshy M, Zhang B, Naqvi S, Liu B, Mohiuddin MM. A novel technique for post-mastectomy breast irradiation utilising non-coplanar intensity-modulated radiation therapy. Br J Radiol. 2010. 83:874–881.

18. Marks LB, Hebert ME, Bentel G, Spencer DP, Sherouse GW, Prosnitz LR. To treat or not to treat the internal mammary nodes: a possible compromise. Int J Radiat Oncol Biol Phys. 1994. 29:903–909.

19. Jeong K, Shim SJ, You SH, Kim YB, Keum KC, Kim JD, et al. A study of the radiotherapy techniques for the breast including internal mammary lymph nodes. J Korean Soc Ther Radiol Oncol. 2009. 27:35–41.

20. Mehta V. Radiation pneumonitis and pulmonary fibrosis in non-small-cell lung cancer: pulmonary function, prediction, and prevention. Int J Radiat Oncol Biol Phys. 2005. 63:5–24.

21. Kwa SL, Lebesque JV, Theuws JC, Marks LB, Munley MT, Bentel G, et al. Radiation pneumonitis as a function of mean lung dose: an analysis of pooled data of 540 patients. Int J Radiat Oncol Biol Phys. 1998. 42:1–9.

22. Sautter-Bihl ML, Hültenschmidt B, Melcher U, Ulmer HU. Radiotherapy of internal mammary lymph nodes in breast cancer. Principle considerations on the basis of dosimetric data. Strahlenther Onkol. 2002. 178:18–24.

23. Kim JY, Lee IJ, Keum KC, Kim YB, Shim SJ, Jeong K, et al. Internal mammary lymph node irradiation after breast conservation surgery: radiation pneumonitis versus dose? Volume histogram parameters. J Korean Soc Ther Radiol Oncol. 2007. 25:261–267.

24. Burman C, Kutcher GJ, Emami B, Goitein M. Fitting of normal tissue tolerance data to an analytic function. Int J Radiat Oncol Biol Phys. 1991. 21:123–135.

25. Lingos TI, Recht A, Vicini F, Abner A, Silver B, Harris JR. Radiation pneumonitis in breast cancer patients treated with conservative surgery and radiation therapy. Int J Radiat Oncol Biol Phys. 1991. 21:355–360.

26. Fowble BL, Solin LJ, Schultz DJ, Goodman RL. Ten year results of conservative surgery and irradiation for stage I and II breast cancer. Int J Radiat Oncol Biol Phys. 1991. 21:269–277.

27. Kubo A, Osaki K, Kawanaka T, Furutani S, Ikushima H, Nishitani H. Risk factors for radiation pneumonitis caused by whole breast irradiation following breast-conserving surgery. J Med Invest. 2009. 56:99–110.

28. Kim HJ, Jang WI, Kim TJ, Kim JH, Kim SW, Moon SH, et al. Radiation-induced pulmonary toxicity and related risk factors in breast cancer. J Breast Cancer. 2009. 12:67–72.

29. Krengli M, Sacco M, Loi G, Masini L, Ferrante D, Gambaro G, et al. Pulmonary changes after radiotherapy for conservative treatment of breast cancer: a prospective study. Int J Radiat Oncol Biol Phys. 2008. 70:1460–1467.

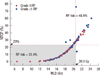
30. Lind PA, Wennberg B, Gagliardi G, Rosfors S, Blom-Goldman U, Lideståhl A, et al. ROC curves and evaluation of radiation-induced pulmonary toxicity in breast cancer. Int J Radiat Oncol Biol Phys. 2006. 64:765–770.








 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download