Abstract
Purpose
The axillary reverse mapping (ARM) technique to identify and preserve arm nodes during sentinel lymph node biopsy (SLNB) or axillary lymph node dissection (ALND) was developed to prevent lymphedema. The purpose of this study was to investigate the location and metastatic rate of the arm node, and to evaluate the short term incidence of lymphedema after arm node preserving surgery.
Methods
From January 2009 to October 2010, 97 breast cancer patients who underwent ARM were included. Blue-dye (2.5 mL) was injected into the ipsilateral upper-inner arm. At least 20 minutes after injection, SLNB or ALND was performed and blue-stained arm nodes and/or lymphatics were identified. Patients were divided into two groups, an arm node preserved group (70 patients had ALND, 10 patients had SLNB) and an unpreserved group (13 patients had ALND, 4 patients had SLNB). The difference in arm circumference between preoperative and postoperative time points was checked in both groups.
Results
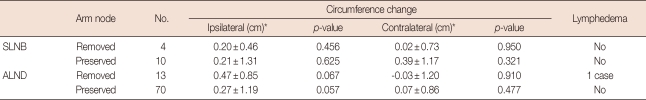
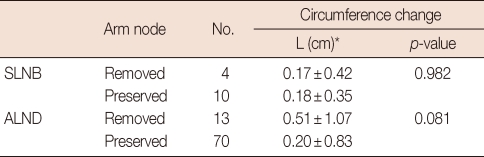
The mean number of identified blue stained arm nodes was 1.4±0.6. In the majority of patients (92%), arm nodes were located between the lower level of the axillary vein and just below the second intercostobrachial nerve. In the arm node unpreserved group, 2 patients had metastasis in their arm node. Among ALND patients, in the arm node preserved group, the difference in arm circumference between preoperative and postoperative time points in ipsilateral and contralateral arms was 0.27 cm and 0.07 cm, respectively, whereas it was 0.47 cm and -0.03 cm in the unpreserved group; one case of lymphedema was found after 6 months. No difference was found between arm node preserved and unpreserved group among SLNB patients.
Sentinel lymph node biopsy (SLNB) has reduced, but not eliminated, surgical complications in those patients who avoid axillary lymph node dissection (ALND). The incidence of lymphedema after ALND has ranged from 6% to 30% [1-3]. However, recent short term studies demonstrated that lymphedema develops in 2-7% of patients with SLNB alone [4-6].
Recently, two articles regarding the preservation of arm nodes in breast cancer patients during ALND or SLNB were published. Both authors concluded that the axillary reverse mapping (ARM) technique is feasible and the detection rate of blue lymphatics and/or nodes is 61-71% [7,8].
The ARM procedure is based on the hypothesis that the lymphatics from the arm are not involved in metastasis of breast cancer. However, several recent articles reported that the sentinel node was the same as the arm node in a small number of patients [9,10]. Another problem is that the identification rate of the arm node by blue dye is relatively low compared to the identification rate of the sentinel lymph node (SLN) [7,8]. The last issue is that the arm node may be involved with metastatic foci in patients with axillary lymph node metastasis [10,11].
In our preliminary study, we confirmed that the arm node can be involved in metastasis from breast cancer through the common lymphatic channel; however, in non-concordant cases, the arm node can be safely preserved except for patients with high N stage [10]. But the location of the arm node and the practical efficacy after arm node preserving surgery remained uncertain.
The aim of this study was to investigate the location of the arm node and the metastatic rate of the arm node, and to evaluate the short term incidence of lymphedema after arm node preserving surgery.
From January 2009 to October 2010, a study was performed using ARM with combined isotope and blue dye identification at Yeungnam University Hospital. If a metastatic sentinel node was identified, ALND was performed. During this period, in the first 3 months, patients who received SLNB only or ALND followed by SLNB were included. Thereafter, patients who received ALND followed by SLNB were included. Patients whose arm nodes were not identified and who had bilateral breast cancer were excluded. Therefore, a total of 97 patients with clinically determined N0-N2 breast cancers were included.
For SLNB procedures, patients were injected with 0.5-1 mCi of 99mTc-human serum albumin (HSA) or 99mTc-phytate diluted with 0.1-0.2 mL of normal saline at the subareolar plexus, 30 minutes to 3 hours prior to surgery. After injection, lymphangiography was performed to identify the number and the location of SLNs. Before incision, radioactivity counts of the injection site, axilla and background were recorded using a hand-held gamma probe (Neoprobe, Dublin, USA) and hot SLN were defined by radioactivity >10% higher than background.
After general anesthesia, 2.5-3.0 mL of blue dye (methylene-blue) was injected subcutaneously in the medial intermuscular groove of the ipsilateral upper arm using a 22-gauge injection needle. After injection, the arm was elevated above the heart level and massaged for 5 minutes to facilitate lymphatic drainage. After at least 20 minutes, SLNB or ALND was performed in the usual manner. We noted blue nodes and/or blue lymphatics during dissection through the axillary fascia. To find the arm node, the first important step was the identification of the second intercostobrachial nerve (Figure 1).
When an arm node looked suspicious for metastasis because of its size or hardness, it was concordant with the SLN, or it was juxtaposed to a SLN that could not be separated from the SLN, the arm node was removed. When the decision as to whether to preserve the arm node or not was difficult, fine needle aspiration or frozen biopsy of a partial resection of the suspicious arm node was performed. Cross-over meant that the SLN and the arm lymph node have common lymphatic channels.
Arm circumference was measured at 10 cm proximal to the medial epicondyle before surgery and every 3 months after surgery. We did a comparison between arm circumference change at the last follow-up point of the ipsilateral upper-extremity and contralateral upper-extremity circumference in each group. A comparison between arm circumference in the ipsilateral upper-extremity of the arm node preserved group and unpreserved group was made, too. These changes in ipsilateral upper-extremity circumference, corrected for any change in the contralateral upper-extremity, were calculated using the following formula, which was introduced by McLaughlin et al. [12]. We defined lymphedema as measurement changes of >2 cm during the follow-up period.
Resected hot or blue lymph nodes that were >5 mm in size were sectioned at 2-mm intervals along the long axis, and those nodes <5 mm in size were sectioned at the largest diameter. Routine hematoxylin and eosin staining was done. The diagnostic criterion for lymph node metastasis was a cluster of >0.2 mm in size in the lymph node according to the 6th American Joint Committee on Cancer.
Data on arm circumference of the ipsilateral upper arm, the location of the arm node, the crossover rate of the arm node, and the metastatic rate of the arm node were collected from all patients. All analyses were done in SPSS for Windows version 17.0 (SPSS Inc., Chicago, USA). The effect of arm node preserving surgery on lymphedema was analyzed by paired t-test (in a comparison between arm circumference changes at the last follow-up point of the ipsilateral upper-extremity and contralateral upper-extremity circumference in each group) and by an independent t-test (in a comparison between arm circumference in the ipsilateral upper-extremity of the arm node preserved group and unpreserved group). A p-value <0.05 was considered significant.
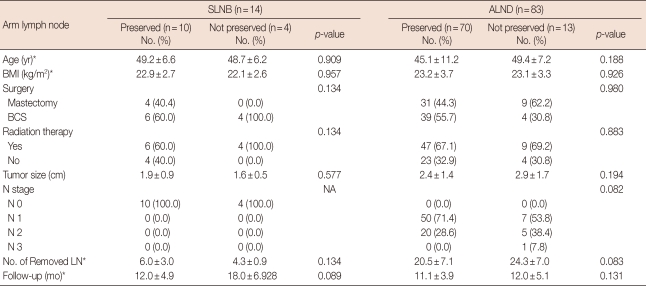
From January 2009 to October 2010, 97 patients with clinically determined N0-N2 breast cancers were studied. The mean age of the study population was 46.2±10.4 years (range, 22-77 years) and the mean body mass index was 23.2±3.5 kg/m2 (range, 16.2-32.9 kg/m2). SLNB was done in all patients and ALND was done in 83 patients (85.6%). Stained arm lymph nodes were removed in 17 patients (17.5%): 4 patients in the SLNB only group and 13 patients in the ALND group. There were no significant differences in the mean tumor size, N stage, operative procedure, the number of removed lymph nodes, or follow-up periods between the arm lymph node preserved group and the unpreserved group (Table 1).
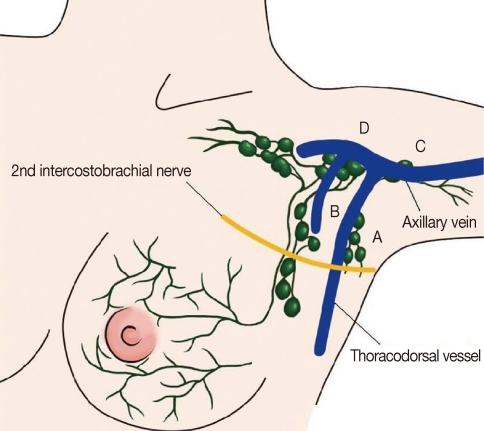
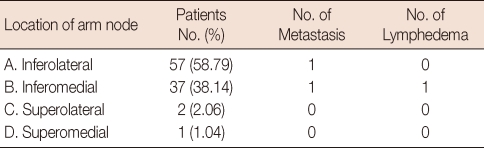
The mean number of identified blue stained arm nodes was 1.4±0.6 (range, 1-4). Average time to detection for arm nodes was 19.2±13.5 minutes. The location of the arm node was the inferolateral side of axillary and thoracodorsal vessels in 57 patients (58.76%), the inferomedial side in 37 patients (38.14%), the superolateral side in 2 patients (2.06%), and the superomedial side in 1 patient (1.04%) (Table 2, Figure 2). Arm nodes were located between the lower level of the axillary vein and just below the second intercostobrachial nerve in the majority of our patients (92%). Metastatic arm nodes were found in inferomedial and inferolateral sides, and the arm node of the patient who developed lymphedema was found in the inferomedial side (Table 2). Among ALND patients, a stained arm lymph node was preserved in 70 patients and removed in 13 patients. Among SLNB only patients, a stained arm lymph node was preserved in 10 patients and removed in 4 patients. Seven patients had high radioactivity in the blue arm lymph node, so a cross-over node was identified in 7 of 97 cases (7.2%). Arm nodes were removed in 17 patients because of adhesion with SLNs (1 case), grossly enlarged arm nodes (5 cases), high surgical N stage (4 cases), and common lymphatic channel (7 cases).
Two patients had metastasis in the arm node. The first patient had a common lymphatic channel between the arm node and the SLN. She had stage IIIA (T3, N2, M0) breast cancer; the histologic grade was 3 with lymphatic invasions and triple negative markers (estrogen receptor [ER] negative, progesterone receptor [PR] negative, human epidermal growth factor 2 [HER2] negative). The metastatic arm node of the second patient was not a common lymphatic channel, but rather an extranodal extension with N3 metastasis. She had stage IIIC (T1, N3, M0); the histologic grade was 3 with lymphovascular invasion, and markers for ER, PR, and HER2 were all negative. The arm node of this patient was removed and she had lymphedema after 6 months.
The mean follow-up period was 9.6±4.3 months (range, 3-24 months): 8.8 months in the ALND group and 13.7 months in the SLNB only group. When comparing between arm circumference changes at the last follow-up point of the ipsilateral upper-extremity and the contralateral upper-extremity circumference, among the ALND group, the change in arm circumference of the ipsilateral upper-extremity after surgery was 0.27±1.19 cm in the arm lymph node preserved group and 0.47±0.85 cm in the unpreserved group. In the SLNB only group, the change in arm circumference after surgery was 0.21±1.31 cm in the arm lymph node preserved group and 0.20±0.46 cm in the unpreserved group (Table 3). When comparing between arm circumferences in ipsilateral upper-extremity of the arm node preserved group and unpreserved group, in the SLNB group and ALND group, there was no significant difference. But in the ALND group, the arm circumference changes of the arm node unpreserved group were bigger than that of the preserved group (0.51±1.07 vs. 0.20±0.83, p=0.081) (Table 4). There were no lymphedema cases among the arm node preserved cases (70 cases), but one lymphedema developed in the unpreserved cases (7.7%), as stated above.
The ARM procedure was first introduced by Thompson et al. [7] and Nos et al. [8] in attempts to identify a separate drainage pathway of arm lymphatics from the sentinel lymphatic pathway to reduce the incidence of lymphedema by preserving the arm lymphatic pathways. The technique of arm node preservation was based on the concept that the arm lymphatic pathway does not communicate with the sentinel lymphatic pathway. Since then, various reports have been introduced [8,11,13-16], but there are some key issues that need to be resolved in arm node preservation. First, the rate of arm node identification by blue dye staining is somewhat insufficient. Second, there are reports of metastasis in arm lymph nodes or in the lymphatic pathway. This raises problems regarding the safety of arm node preservation surgery. Third, common lymphatic channels are found between SLNs and arm lymph nodes. When a common channel exists, even SLNB can cause lymphedema. Fourth, the stained blue arm node may be juxtaposed to the metastatic lymph node, which could result in direct invasion of the carcinoma and make it difficult to save the arm node.
With the use of blue dye in arm lymph node detection, the detection rate has been 61-78.3% [7,8,13,16-18]. This low detection rate is associated with a short interval between dye injection and surgery, and a deeper location of the arm node than the SLN, which makes it hard to identify the arm node in the surgical field, and a lower detection rate of blue dye compared with radioisotope. In recent reports, the use of radioisotopes or fluorescence has increased the detection rate to 88-100% [9,11,14].
In our preliminary study, the identification rate of arm nodes was 78%. In this study, the identification rate of arm nodes was not included in the original design of this study and not investigated because of the possibility of causing lymphatic injury by dissection beyond the SLNB field while searching for the arm node. We included only patients whose arm node was identified. Therefore, patients who had ALND were more frequently included than those who had only SLNB. Average time to detection for the arm node was 19.2±13.5 minutes. During the operation, about 10 minutes after blue dye injection, we could find hardly any blue-stained arm nodes. When injected intravenously, the plasma half-life of methylene-blue dye has been reported as 5-6.5 hours [19,20]. However, the pharmacokinetics of methylene-blue dye in the lymphatic system and lymph nodes has not been well studied. In our study, although time to detection for the arm node was >40 minutes in some cases, it did not seem to affect washing out of blue dye. Further studies are needed for determination of optimal time to detection of arm nodes.
Metastasis of the arm node develops in 0-43% of patients [7,10,11,13,14]. Thompson et al. [7] and Nos et al. [8] reported that none of the arm nodes contained metastasis in the initial study. Later, Nos et al. [11] reported that ARM nodes showed metastatic involvement in 3 of 21 patients with N1-3 (14%). Similarly, in a study by Noguchi et al. [14], the metastatic rate for arm nodes was 3 of 7 patients (43%) with a clinically positive node or positive SLN, and all were pN3. According to the study of Bedrosian et al. [13], the metastatic rate of arm nodes was 18%, including patients who received neoadjuvant chemotherapy. When we summarized these results, arm node preserving surgery was contraindicated in patients who had a high N stage (N3).
In our study, two patients had metastasis in arm lymph nodes. Possible explanations for such metastasis in an arm lymph node are a common lymphatic pathway, lymphatic interconnections or direct invasion from juxtaposed sites of metastasis. So, locally advanced breast cancer and N3 lymphatic invasion should be contraindications for ARM and arm node preserving procedures. In our cases, one patient had a common lymphatic pathway and the other patient had extensive nodal metastasis with N3 disease without common lymphatic pathways, suggesting direct invasion or lymphatic interconnections from metastatic nodes.
In a recent article, the cross-over rate was 2.8-21%, depending on the methods, and included patients' characteristics [9,10,14,18]. Indeed, if a cross-over node was identified among SLNs, their preservation could be impossible. So when a crossover node is removed at SLNB, lymphedema could occur even after SLNB. In our study, the cross-over rate between arm and SLNs was 7.2%; a few previous reports have identified crossover rates of 13.3% and 18.9% [9,10].
All arm nodes cannot be preserved. When a surgeon suspects that the arm node may involve metastasis in an operation field, preservation of the arm nodes mainly depends on the surgeon's experience. So we used fine needle aspiration or frozen biopsy of partial resection of suspicious arm nodes during the operation. The number of patients from whom arm nodes were removed was 17; 7 patients had common lymphatic pathways with SLNs, 4 patients had grossly enlarged arm nodes, 4 patients had high surgical N stage, 1 patient had adhesions with a SLN, and 1 patient had a metastatic arm node on frozen biopsy.
Boneti et al. [21] demonstrated 5 anatomic variations in arm drainage including the traditional teaching of lymphatics from the arm running juxtaposed to the axillary vein either above or below, slung low in the axilla, lateral apron, or medial apron (lateral and medial aprons usual consist of multiple blue nodes), or an entwined cord of lymphatics. The arm node was localized in the lateral pillar of the axilla, and it was always found above or at the level of the second intercostobrachial nerve [11]. In our study, 97% of nodes were located between the lower level of the axillary vein and the second intercostobrachial nerve. To identify the arm node, an important landmark in the operative field is the axillary vein and the second intercostobrachial nerve. The metastatic arm nodes were found in the inferomedial and inferolateral sides, one by each side, and the arm node of the patient who developed lymphedema was found in the inferomedial side. If more patients were included, statistical analysis would be possible, and the relationship between the location and metastasis of arm nodes would be identified.
Boneti et al. [18] reported that there were no cases of lymphedema in those who had an arm node preserved at 6 months follow-up. In 51 patients with arm node preserving surgery, the incidence of lymphedema in those who had an arm node resected was 2 of 15 patients (13%). Casabona et al. [16] similarly reported that there was no lymphedema at 9 months follow-up in 72 patients with arm node preserving surgery. In our study, average follow-up periods were 9.4 months. Of course, in the arm node preserved group, there was no lymphedema.
For assessment of lymphedema, there are many methods such as measurement of arm circumference, water displacement, self-assessment, bioimpedance spectroscopy and perometry [12,22-26]. Measurement of arm circumference, used in our study, is simple and inexpensive, so it is routinely used in many studies as the method. In the ALND group, the absolute change in arm circumference before and after the operation was 0.27±1.19 cm in the arm lymph node preserved group and 0.47±0.85 cm in the unpreserved group; the difference was not statistically significant. However, the arm lymph node preserved group showed a tendency towards less change in arm circumference than the unpreserved group. When making comparisons between arm circumferences in the ipsilateral upper-extremity of the arm node preserved group and unpreserved group, according to the formula introduced by McLaughlin et al. [12], there was no significant difference. But in the ALND group, the arm circumferences changes of the arm node unpreserved group were bigger than the preserved group (0.51±1.07 vs. 0.20±0.83, p=0.081). There were no cases of lymphedema in 70 patients in whom the arm node was preserved during ALND, but there was 1 case of lymphedema in 13 patients in whom the arm node was resected during ALND. To verify the efficacy of arm lymph node preservation in preventing lymphedema, more patients should be included and longer follow-up periods are needed. We defined lymphedema as a measurement change of >2 cm during the follow-up period, but, self-assessed symptoms are also important. Although measurement change was less than 2 cm, if the patient feels discomforts, she may have lymphedema. In a future study, we should check patient's subjective symptoms. There was no significant change in arm circumference in the SLNB only group, and it was difficult to determine the efficacy of arm lymph node preservation because of the small number of patients. There was no axillary recurrence during the follow-up period in patients who underwent arm node preserving surgery. But, oncologic safety should be observed, always. Further studies about actual regional recurrence in preserved arm nodes are needed. In practical terms, arm node preserving surgery gives no advantage to patients with a cross-over node or N0, but does benefit patients with N1 and N2. Standard SLNB is not indicated in patients with N1 or N2, but SLNB should be done to preserve the arm nodes in these patients.
In conclusion, arm node preserving surgery may prevent lymphedema in SLNB and/or ALND in patients with clinically determined N1 or N2 breast cancer.
Notes
References
1. Petrek JA, Senie RT, Peters M, Rosen PP. Lymphedema in a cohort of breast carcinoma survivors 20 years after diagnosis. Cancer. 2001; 92:1368–1377. PMID: 11745212.

2. Ivens D, Hoe AL, Podd TJ, Hamilton CR, Taylor I, Royle GT. Assessment of morbidity from complete axillary dissection. Br J Cancer. 1992; 66:136–138. PMID: 1637663.

3. Newman ML, Brennan M, Passik S. Lymphedema complicated by pain and psychological distress: a case with complex treatment needs. J Pain Symptom Manage. 1996; 12:376–379. PMID: 8973048.

4. Schrenk P, Rieger R, Shamiyeh A, Wayand W. Morbidity following sentinel lymph node biopsy versus axillary lymph node dissection for patients with breast carcinoma. Cancer. 2000; 88:608–614. PMID: 10649254.

5. Sener SF, Winchester DJ, Martz CH, Feldman JL, Cavanaugh JA, Winchester DP, et al. Lymphedema after sentinel lymphadenectomy for breast carcinoma. Cancer. 2001; 92:748–752. PMID: 11550143.

6. Wilke LG, McCall LM, Posther KE, Whitworth PW, Reintgen DS, Leitch AM, et al. Surgical complications associated with sentinel lymph node biopsy: results from a prospective international cooperative group trial. Ann Surg Oncol. 2006; 13:491–500. PMID: 16514477.

7. Thompson M, Korourian S, Henry-Tillman R, Adkins L, Mumford S, Westbrook KC, et al. Axillary reverse mapping (ARM): a new concept to identify and enhance lymphatic preservation. Ann Surg Oncol. 2007; 14:1890–1895. PMID: 17479341.

8. Nos C, Lesieur B, Clough KB, Lecuru F. Blue dye injection in the arm in order to conserve the lymphatic drainage of the arm in breast cancer patients requiring an axillary dissection. Ann Surg Oncol. 2007; 14:2490–2496. PMID: 17549570.

9. Britton TB, Solanki CK, Pinder SE, Mortimer PS, Peters AM, Purushotham AD. Lymphatic drainage pathways of the breast and the upper limb. Nucl Med Commun. 2009; 30:427–430. PMID: 19319006.

10. Choi JE, Jeon YS, Kang SH, Lee SJ. Preservation of lymphatic drainage of arm during axillary procedure in breast cancer patients. J Breast Cancer. 2009; 12:179–185.

11. Nos C, Kaufmann G, Clough KB, Collignon MA, Zerbib E, Cusumano P, et al. Combined axillary reverse mapping (ARM) technique for breast cancer patients requiring axillary dissection. Ann Surg Oncol. 2008; 15:2550–2555. PMID: 18618185.

12. McLaughlin SA, Wright MJ, Morris KT, Giron GL, Sampson MR, Brockway JP, et al. Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: objective measurements. J Clin Oncol. 2008; 26:5213–5219. PMID: 18838709.

13. Bedrosian I, Babiera GV, Mittendorf EA, Kuerer HM, Pantoja L, Hunt KK, et al. A phase I study to assess the feasibility and oncologic safety of axillary reverse mapping in breast cancer patients. Cancer. 2010; 116:2543–2548. PMID: 20336790.

14. Noguchi M, Yokoi M, Nakano Y. Axillary reverse mapping with indocyanine fluorescence imaging in patients with breast cancer. J Surg Oncol. 2010; 101:217–221. PMID: 20063370.

15. Noguchi M. Axillary reverse mapping for breast cancer. Breast Cancer Res Treat. 2010; 119:529–535. PMID: 19842033.

16. Casabona F, Bogliolo S, Valenzano Menada M, Sala P, Villa G, Ferrero S. Feasibility of axillary reverse mapping during sentinel lymph node biopsy in breast cancer patients. Ann Surg Oncol. 2009; 16:2459–2463. PMID: 19506954.

17. Ponzone R, Mininanni P, Cassina E, Sismondi P. Axillary reverse mapping in breast cancer: can we spare what we find? Ann Surg Oncol. 2008; 15:390–391. PMID: 17990039.

18. Boneti C, Korourian S, Diaz Z, Santiago C, Mumford S, Adkins L, et al. Scientific Impact Award: axillary reverse mapping (ARM) to identify and protect lymphatics draining the arm during axillary lymphadenectomy. Am J Surg. 2009; 198:482–487. PMID: 19800452.

19. Peter C, Hongwan D, Küpfer A, Lauterburg BH. Pharmacokinetics and organ distribution of intravenous and oral methylene blue. Eur J Clin Pharmacol. 2000; 56:247–250. PMID: 10952480.

20. Walter-Sack I, Rengelshausen J, Oberwittler H, Burhenne J, Mueller O, Meissner P, et al. High absolute bioavailability of methylene blue given as an aqueous oral formulation. Eur J Clin Pharmacol. 2009; 65:179–189. PMID: 18810398.

21. Boneti C, Korourian S, Bland K, Cox K, Adkins LL, Henry-Tillman RS, et al. Axillary reverse mapping: mapping and preserving arm lymphatics may be important in preventing lymphedema during sentinel lymph node biopsy. J Am Coll Surg. 2008; 206:1038–1042. PMID: 18471751.

22. Deutsch M, Land S, Begovic M, Sharif S. The incidence of arm edema in women with breast cancer randomized on the National Surgical Adjuvant Breast and Bowel Project study B-04 to radical mastectomy versus total mastectomy and radiotherapy versus total mastectomy alone. Int J Radiat Oncol Biol Phys. 2008; 70:1020–1024. PMID: 18029105.

23. Gartner R, Jensen MB, Kronborg L, Ewertz M, Kehlet H, Kroman N. Self-reported arm-lymphedema and functional impairment after breast cancer treatment: a nationwide study of prevalence and associated factors. Breast. 2010; 19:506–515. PMID: 20561790.
24. Ward LC. Bioelectrical impedance analysis: proven utility in lymphedema risk assessment and therapeutic monitoring. Lymphat Res Biol. 2006; 4:51–56. PMID: 16569209.

25. Stanton AW, Northfield JW, Holroyd B, Mortimer PS, Levick JR. Validation of an optoelectronic limb volumeter (Perometer). Lymphology. 1997; 30:77–97. PMID: 9215977.
26. Shah C, Vicini FA. Breast cancer-related arm lymphedema: incidence rates, diagnostic techniques, optimal management and risk reduction strategies. Int J Radiat Oncol Biol Phys. 2011; 81:907–914. PMID: 21945108.

Figure 1
Arm node. The arm node is usually located between the lower level of axillary vein and above or at the level of the second intercostobrachial nerve.
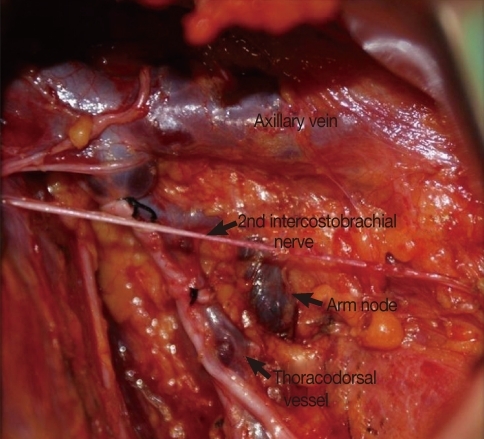
Figure 2
Location of arm node. According to the axillary vein and thoracodorsal vessels, we divided the region into four quadrants.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download