Abstract
Curcumin, which is extracted from the plant Curcuma longa, has been used in the therapeutic arsenal for clinical oncology. Curcumin has chemopreventive and antitumoral activities against some aggressive and recurrent cancers. The expressions and activities of various proteins, such as inflammatory cytokines and enzymes, transcription factors, and gene-products linked with cell survivals and proliferation, can be modified by curcumin. Moreover, curcumin decreases the toxic effect of mitomycin C. Though curcumin has shown highly cytotoxic to some cancer cell lines, curcumin is insoluble and instable in water. The solubility of curcumin could be enhanced by utilizing the solubilizing properties of rubusoside. In addition, the selective delivery of synthetic analogs or nanotechnology-based formulations of curcumin to tumors may improve the chemopreventive and chemotherapeutic effects. The focus of this short review is to describe how curcumin participates in antitumor processes in breast cancer cells.
It is known that breast cancer is the most common cancer for women worldwide, and accounts for approximately 25% of all female malignancies with a higher prevalence in developed countries. Breast cancer is the second leading cause of cancer-related death among females in the world [1]. Curcumin (1,7-bis(4-hydroxy-3-methoxyphenyl)-1,6-heptadiene-3,5-dione) (Figure 1), which is extracted from the plant Curcuma longa, is an antioxidant that exerts antiproliferative and apoptotic effects. The expressions and activities of various proteins, such as inflammatory cytokines and enzymes, transcription factors, and gene-products linked with cell survivals and proliferation, can be modified by curcumin [2]. Since curcumin possesses anti-inflammatory, antioxidant, and antitumoral effects, it has been studied vigorously as a chemopreventative agent in some cancer models and used in the therapeutic arsenal in clinical oncology. However, curcumin is insoluble and instable in water. The solubility of curcumin could be enhanced by utilizing the solubilizing properties of rubusoside. In addition, the selective delivery of synthetic analogs or nanotechnology-based formulations of curcumin to tumors may improve the chemopreventive and chemotherapeutic effects. The focus of this short review is to describe how curcumin participates in the regulation of oncogene protein expression in breast cancer cells.
Curcumin inhibits the proliferation of various tumor cells in culture and prevents carcinogen-induced cancers in rodents. In xenotransplant or orthotransplant animal models, the growth of human tumors was inhibited by curcumin alone or in combination with chemotherapeutic agents or radiation [2]. Banerjee et al. [3] reported that curcumin induced G2/M arrest and apoptosis, inhibited cell proliferation by inhibiting the assembly dynamics of microtubules, and further activated the mitotic checkpoint in MCF-7 cells. Furthermore, cells were accumulated in the G(1) phase of the cell cycle, and curcumin suppressed the expression of zeste homolog 2 (EZH2) gene via the stimulation of three major members of the mitogen-activated protein kinase (MAPK) pathway: c-Jun NH2-terminal kinase (JNK), extracellular signal-regulated kinase (ERK), and p38 kinase (Figure 2) [4].
The apoptosis is involved in the curcumin-induced inhibition of tumor cell growth. It was found that curcumin inhibited the expression of Ki-67, proiferating cell nuclear antigen (PCNA), and p53 mRNAs in breast cancer cells, and induced Bax mRNA expression with the down-regulation of p21 mRNA in the human mammary epithelial cell line (Figure 2) [5]. The development of breast cancer is associated with the abnormal activation of the Wnt/β-catenin signaling pathway, and curcumin inhibits the expression of β-catenin, cyclin D1, and slug in both MCF-7 and MDA-MB-231 cells (Figure 2) [6].
Maspin is a serine protease inhibitor, which suppresses tumor growth and metastasis in vivo and tumor cell motility and invasion in vitro. The results of Prasad et al. [7] indicated that the maspin gene expression was increased by curcumin in MCF-7 cells with the up-regulation of p53 protein and down-regulation of Bcl-2 (Figure 2). Another report indicated that curcumin reduced the expression of Bcl-2 by up-regulating the expression of miR-15a and miR-16 in MCF-7 cells (Figure 2) [8]. However, the data of Chiu and Su [9] showed that curcumin inhibited the proliferation of MDA-MB-231 cells either through up-regulating p21 expression or up-regulating the Bax to Bcl-2 ratio. Moreover, the AIP-1/Alix protein, which is an inhibitor protein of paraptosis, was progressively down-regulated in curcumin-treated malignant breast cancer cells (Figure 2) [10]. In curcumin-induced paraptosis, mitochondrial superoxide acted as a critical early signal and proteasomal dysfunction was mainly responsible for the paraptotic changes associated with estrogen receptor (ER) dilation [10]. It was also found that curcumin inhibited breast cancer cell motility and invasion by directly inhibiting the function of α6β4 integrin [11].
Most anticancer agents activate nuclear factor-κB (NF-κB), which mediates cell survival, proliferation, and metastasis. It has been found that curcumin inhibits the migratory activity of breast cancer cells, proliferative rate, adhesion, and invasion through down-regulating the expression of NF-κBp65 [9,12-14]. Human epidermal growth factor 2 (HER2) is an important oncoprotein, which is overexpressed in about 15% to 25% of breast cancers. Curcumin decreased HER2 oncoprotein, phosphorylation of Akt, MAPK, and the expression of NF-κB in both BT-474 and SK-BR-3-hr cells (Figure 3) [15]. Furthermore, curcumin enhanced the efficacy of chemotherapy by tailoring p65NF-κB-p300 cross-talk in favor of p53-p300 for breast cancer [16]. Curcumin also shows a potential therapeutic role in blocking recepteur d'origine nantais (RON) tyrosine kinase-mediated invasion of carcinoma cells by affecting p65 protein expression and transcriptional activity via NF-κB (Figure 3) [17].
Curcumin may provide a clinically useful tool for the suppression of the elaboration of vascular endothelial growth factor (VEGF) in tumor cells (Figure 3). It has been found that curcumin suppressed breast tumor angiogenesis by abrogating osteopontin or medroxyprogesterone acetate induced VEGF expression [18,19]. Curcumin inhibited α6β4 signaling and functions by altering intracellular localization of α6β4, and prevented its association with signaling receptors such as the epidermal growth factor receptor (EGFR) and Akt [20,21]. In addition, the combination of epigallocatechin gallate (EGCG) and curcumin is efficacious in both in vitro and in vivo models of ERα-breast cancer. In this processes, the regulation of VEGFR-1 may play a key role in the antitumor activities [21].
Curcumin has been studied vigorously as a chemopreventative in several cancer models. Since cleaved poly (ADP-ribose) polymerase 1 (PARP-1) plays a significant role on cellular protection against radiation and estrogen-induced DNA damage mediated by curcumin, targeting PARP-1 may provide an effective way of maximizing the therapeutic value of antioxidants for cancer prevention (Figure 3) [22]. On the other hand, the F-box protein S-phase kinase-associated protein 2 (Skp2), which acts as an oncogene through targeting p27 for degradation, is overexpressed in many different human cancers. Because curcumin induces p27 expression and growth arrest through the inhibition of Skp2 in MDA-MB-231 cells, the therapeutic strategies designed to reduce Skp2 may therefore play an important clinical role in treatment of ER/HER2 negative breast cancers (Figure 3) [23]. In addition, phosphatase of regenerating liver-3 (PRL-3) was also treated as a potential target for anticancer drugs based on its involvement in tumor metastasis. It was found that curcumin inhibited the phosphorylation of Src and stat3 partly through PRL-3 down-regulation, raising its possibilities in therapeutic regimen against malignant tumor (Figure 3) [24].
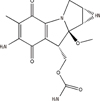
Mitomycin C (MMC) (Figure 4), a potent DNA cross-linker and antineoplastic agent, is usually used to fight various cancers. However, the use of MMC is limited because the prolonged use of MMC will result in permanent kidney or bone marrow damage and secondary tumors in normal cells. It has been found that curcumin improves MMC-based chemotherapy by simultaneously sensitizing cancer cells to MMC and reducing MMC-associated side-effects, increasing cell viability, and further decreasing lipid peroxidation and DNA damage [25,26]. The combination treatment of MMC and curcumin reduces the toxic effect of MMC by inhibiting glucose regulatory protein (GRP58)-mediated DNA cross-linking through the ERK/p38 MAPK pathway (Figure 5) [27]. Another report indicated that curcumin enhanced antiproliferative effect of MMC in human breast cancer MCF-7 cells via the p38 MAPK pathway [25]. The cell cycle arrest was associated with the inhibition of cyclin D1, cyclin E, cyclin A, cyclin-dependent kinase 2 (CDK2), and CDK4. But the cell cycle inhibitors p21 and p27 were induced in MCF-7 cells and MCF-7 xenografts (Figure 5) [25].
Though curcumin has been indicated as highly cytotoxic towards various cancer cell lines, its insolubility and instability in water contributes to low bioavailability. On the other hand, photodegradation and low bioavailability are major hurdles for the therapeutic use of curcumin. However, the solubility of curcumin could be enhanced by utilizing the solubilizing properties of rubusoside, and the rubusoside-solubilized curcumin successfully inhibited cell viability in human colon, breast, and pancreatic cancer cell lines [28]. In order to increase curcumin photostability and enhance its anticancer activity against MCF-7 breast cancer cells, Mulik et al. [29] formulated the transferrin-mediated solid lipid nanoparticles (Tf-C-SLN), which enhances the anticancer effect of curcumin in breast cancer cells in vitro. Moreover, it was found that curcumin conjugated with phosphatidylcholine increased curcumin bioavailability five-fold compared to original curcumin [30]. The prodrugs, which are produced by mono-PEGylation of curcumin, are stable in buffer at physiological pH and released curcumin readily in human plasma [31].
The polycurcumins have high drug loading efficiency and can be used as backbone-type conjugates. The polycurcumins could fix drug loading contents, stabilize curcumin in their backbones, and tailor water-solubility. Tang et al. [32] made the high molecular weight curcumin polymers (polycurcumins) through condensation polymerization of curcumin. It was found that the polyacetal-based polycurcumin was not only highly cytotoxic to MCF-7 breast cancer cell lines but also showed significant antitumor activities in SKOV-3 intraperitoneal xenograft tumor models [32].
Recently, the potential effect of curcumin on cancer cells has been recognized by the scientific community in the world, and the molecular biological approaches help to elucidate the underlying mechanisms of actions on curcumin in tumor cells. However, the molecular mechanisms underlying the antitumor activity of curcumin have not been very clear until now. Another thing is that the molecular mechanism of curcumin on tumor cells was usually studied with tumor cell lines in vitro, and the molecular mechanisms in vivo need to be further investigated. More sophisticated technologies will have to be applied in conjunction so that curcumin derivatives could be used for rational cancer therapy.
Figures and Tables
 | Figure 2Curcumin inhibits the expression of zeste homologue 2 (EZH2) gene, AIP-1/Alix protein, Ki-67, proiferating cell nuclear antigen (PCNA), Bcl-2, and genes related to Wnt/β-catenin signaling pathway in cancer cells, but induces the expression of maspin and Bax in cancer cells.
JNK=c-Jun NH2-terminal kinase; ERK=extracellular signal-regulated kinase.
|
 | Figure 3Curcumin inhibits the expression of recepteur d'origine nantais (RON), human epidermal growth factor 2 (HER2), Akt, mitogen-activated protein kinase (MAPK), nuclear factor-κB (NF-κB), vascular endothelial growth factor (VEGF) and the phosphorylation of Src and stat3 through PRL-3 down-regulation, but induces the expression of p27 and poly (ADP-ribose) polymerase 1 (PARP-1) in cancer cells. |
Notes
References
1. Park MT, Kim MJ, Kang YH, Choi SY, Lee JH, Choi JA, et al. Phytosphingosine in combination with ionizing radiation enhances apoptotic cell death in radiation-resistant cancer cells through ROS-dependent and -independent AIF release. Blood. 2005; 105:1724–1733.

2. Kunnumakkara AB, Anand P, Aggarwal BB. Curcumin inhibits proliferation, invasion, angiogenesis and metastasis of different cancers through interaction with multiple cell signaling proteins. Cancer Lett. 2008; 269:199–225.

3. Banerjee M, Singh P, Panda D. Curcumin suppresses the dynamic instability of microtubules, activates the mitotic checkpoint and induces apoptosis in MCF-7 cells. FEBS J. 2010; 277:3437–3448.

4. Hua WF, Fu YS, Liao YJ, Xia WJ, Chen YC, Zeng YX, et al. Curcumin induces down-regulation of EZH2 expression through the MAPK pathway in MDA-MB-435 human breast cancer cells. Eur J Pharmacol. 2010; 637:16–21.

5. Ramachandran C, You W. Differential sensitivity of human mammary epithelial and breast carcinoma cell lines to curcumin. Breast Cancer Res Treat. 1999; 54:269–278.

6. Prasad CP, Rath G, Mathur S, Bhatnagar D, Ralhan R. Potent growth suppressive activity of curcumin in human breast cancer cells: Modulation of Wnt/beta-catenin signaling. Chem Biol Interact. 2009; 181:263–271.

7. Prasad CP, Rath G, Mathur S, Bhatnagar D, Ralhan R. Expression analysis of maspin in invasive ductal carcinoma of breast and modulation of its expression by curcumin in breast cancer cell lines. Chem Biol Interact. 2010; 183:455–461.

8. Yang J, Cao Y, Sun J, Zhang Y. Curcumin reduces the expression of Bcl-2 by upregulating miR-15a and miR-16 in MCF-7 cells. Med Oncol. 2010; 27:1114–1118.

9. Chiu TL, Su CC. Curcumin inhibits proliferation and migration by increasing the Bax to Bcl-2 ratio and decreasing NF-kappaBp65 expression in breast cancer MDA-MB-231 cells. Int J Mol Med. 2009; 23:469–475.
10. Yoon MJ, Kim EH, Lim JH, Kwon TK, Choi KS. Superoxide anion and proteasomal dysfunction contribute to curcumin-induced paraptosis of malignant breast cancer cells. Free Radic Biol Med. 2010; 48:713–726.

11. Kim HI, Huang H, Cheepala S, Huang S, Chung J. Curcumin inhibition of integrin (alpha6beta4)-dependent breast cancer cell motility and invasion. Cancer Prev Res (Phila). 2008; 1:385–391.

12. Liu Q, Loo WT, Sze SC, Tong Y. Curcumin inhibits cell proliferation of MDA-MB-231 and BT-483 breast cancer cells mediated by down-regulation of NFkappaB, cyclinD and MMP-1 transcription. Phytomedicine. 2009; 16:916–922.

13. Zong H, Wang F, Fan QX, Wang LX. Curcumin inhibits metastatic progression of breast cancer cell through suppression of urokinase-type plasminogen activator by NF-kappa B signaling pathways. Mol Biol Rep. 2012; 39:4803–4808.

14. Kang HJ, Lee SH, Price JE, Kim LS. Curcumin suppresses the paclitaxel-induced nuclear factor-kappaB in breast cancer cells and potentiates the growth inhibitory effect of paclitaxel in a breast cancer nude mice model. Breast J. 2009; 15:223–229.

15. Lai HW, Chien SY, Kuo SJ, Tseng LM, Lin HY, Chi CW, et al. The potential utility of curcumin in the treatment of HER-2-overexpressed breast cancer: an in vitro and in vivo comparison study with herceptin. Evid Based Complement Alternat Med. 2012; 2012:486568.
16. Sen GS, Mohanty S, Hossain DM, Bhattacharyya S, Banerjee S, Chakraborty J, et al. Curcumin enhances the efficacy of chemotherapy by tailoring p65NFκB-p300 cross-talk in favor of p53-p300 in breast cancer. J Biol Chem. 2011; 286:42232–42247.

17. Narasimhan M, Ammanamanchi S. Curcumin blocks RON tyrosine kinase-mediated invasion of breast carcinoma cells. Cancer Res. 2008; 68:5185–5192.

18. Chakraborty G, Jain S, Kale S, Raja R, Kumar S, Mishra R, et al. Curcumin suppresses breast tumor angiogenesis by abrogating osteopontin-induced VEGF expression. Mol Med Rep. 2008; 1:641–646.

19. Carroll CE, Ellersieck MR, Hyder SM. Curcumin inhibits MPA-induced secretion of VEGF from T47-D human breast cancer cells. Menopause. 2008; 15:570–574.

20. Soung YH, Chung J. Curcumin inhibition of the functional interaction between integrin α6β4 and the epidermal growth factor receptor. Mol Cancer Ther. 2011; 10:883–891.

21. Somers-Edgar TJ, Scandlyn MJ, Stuart EC, Le Nedelec MJ, Valentine SP, Rosengren RJ. The combination of epigallocatechin gallate and curcumin suppresses ER alpha-breast cancer cell growth in vitro and in vivo. Int J Cancer. 2008; 122:1966–1971.

22. Calaf GM, Echiburu-Chau C, Wen G, Balajee AS, Roy D. Effect of curcumin on irradiated and estrogen-transformed human breast cell lines. Int J Oncol. 2012; 40:436–442.

23. Huang HC, Lin CL, Lin JK. 1,2,3,4,6-penta-O-galloyl-β-D-glucose, quercetin, curcumin and lycopene induce cell-cycle arrest in MDA-MB-231 and BT474 cells through downregulation of Skp2 protein. J Agric Food Chem. 2011; 59:6765–6775.

24. Wang L, Shen Y, Song R, Sun Y, Xu J, Xu Q. An anticancer effect of curcumin mediated by down-regulating phosphatase of regenerating liver-3 expression on highly metastatic melanoma cells. Mol Pharmacol. 2009; 76:1238–1245.

25. Zhou QM, Wang XF, Liu XJ, Zhang H, Lu YY, Huang S, et al. Curcumin improves MMC-based chemotherapy by simultaneously sensitising cancer cells to MMC and reducing MMC-associated side-effects. Eur J Cancer. 2011; 47:2240–2247.

26. Siddique YH, Ara G, Beg T, Gupta J, Afzal M. Assessment of cell viability, lipid peroxidation and quantification of DNA fragmentation after the treatment of anticancerous drug mitomycin C and curcumin in cultured human blood lymphocytes. Exp Toxicol Pathol. 2010; 62:503–508.

27. Zhou QM, Zhang H, Lu YY, Wang XF, Su SB. Curcumin reduced the side effects of mitomycin C by inhibiting GRP58-mediated DNA cross-linking in MCF-7 breast cancer xenografts. Cancer Sci. 2009; 100:2040–2045.

28. Zhang F, Koh GY, Jeansonne DP, Hollingsworth J, Russo PS, Vicente G, et al. A novel solubility-enhanced curcumin formulation showing stability and maintenance of anticancer activity. J Pharm Sci. 2011; 100:2778–2789.

29. Mulik RS, Monkkonen J, Juvonen RO, Mahadik KR, Paradkar AR. Transferrin mediated solid lipid nanoparticles containing curcumin: enhanced in vitro anticancer activity by induction of apoptosis. Int J Pharm. 2010; 398:190–203.

30. Ibrahim A, El-Meligy A, Fetaih H, Dessouki A, Stoica G, Barhoumi R. Effect of curcumin and Meriva on the lung metastasis of murine mammary gland adenocarcinoma. In Vivo. 2010; 24:401–408.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download