Abstract
PURPOSE
The purpose of this in vitro study was to investigate the flexural properties of a recently introduced urethane dimethacrylate denture base material (Eclipse) after being repaired with two different materials.
MATERIALS AND METHODS
Two repair groups and a control group consisting of 10 specimens each were generated. The ES group was repaired with auto-polymerizing polymer. The EE group was repaired with the Eclipse. The E group was left intact as a control group. A 3-point bending test device which was set to travel at a crosshead speed of 5 mm/min was used. Specimens were loaded until fracture occurred and the mean displacement, maximum load, flexural modulus and flexural strength values and standard deviations were calculated for each group and the data were statistically analyzed. The results were assessed at a significance level of P<.05.
RESULTS
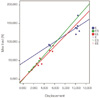
The mean "displacement", "maximum load before fracture", "flexural strength" and "flexural modulus" rates of Group E were statistically significant higher than those of Groups ES and EE, but no significant difference (P>.05) was found between the mean values of Group ES and EE. There was a statistically significant positive relation (P<.01) between the displacement and maximum load of Group ES (99.5%), Group EE (94.3%) and Group E (84.4%).
An ultimate denture base material should acquire several key properties such as biocompatibility, good esthetics, high bond strength with artificial teeth, radiopacity, ease of repair, and should possess adequate physical and mechanical properties.1,2 Polymethyl methacrylate (PMMA) which is believed to fulfill most of these properties is the most frequently used denture base material for conventional as well as implant-retained removable dentures.3 The rationale for this extensive handling is low water sorption, solubility and cost; construction of denture bases by simple processing techniques with adequate strength.4 Despite these favorable properties, a growing number of patients are presenting with hypersensitive reactions to PMMA. Therefore, PMMA should be replaced with hypoallergenic materials in these patients. Allergic reactions may be induced by the residual methyl methacrylate monomer (MMA).5 Therefore, presumably hypoallergenic resins such as urethane dimethacrylate, polyurethane, polyethylenterephthalate, and polybutylenterephthalate have been developed to replace MMA or the content of the residual monomer has been reduced.3,5,6
The fracture of an acrylic resin prostheses can frequently be encountered in dental practice, resulting from fatigue of the base material during function and mastication and weakening of the base material due to water sorption in the oral environment.5,7-9 Furthermore, the adaptation of the prosthesis deteriorates over time due to resorption of the alveolar ridge.8,10-12 In addition, since these prostheses are removable, shock induced fracture resistance due to patient abuse is desirable.2 Therefore, most manufacturers of PMMA denture resins add cross-linking agents such as glycol dimethacrylate and rubber or fibers to modify mechanical properties to improve impact resistance, and to prevent crack propagation.13-15
Light-activated urethane dimethacrylate resins were developed as a substitute for PMMA to eliminate contact allergies and long flasking procedures.16 Additionally, the long aliphatic polyether segment in the repeated unit provides improved chain flexibility, and improves the toughness of urethane dimethacrylate resins.17
More recently, a new light activated denture base material was introduced (Eclipse, Dentsply, York, PA, USA).16 This system is made of three types of resins available in four shades; baseplate resin, setup resin and contour resin. The denture record base is fabricated from the baseplate resin and, after light polymerization; it becomes the permanent denture base of the final denture. The denture teeth are attached to the baseplate resin using the setup resin and finally the contour resin is overlaid over the baseplate resin and light-polymerized.16 It has been shown that Eclipse exhibited significantly higher flexural and impact strengths as compared with high impact PMMA denture bases.16,18
The goal of denture repair is to restore the denture to its original strength.8,19,20 There are previous studies showing that the repair strength of various repair resins exhibit a dramatic decrease compared to the original strength of the denture.7,8,19,21,22 Final repair strength of the denture depends on several factors such as the laboratory procedures (width of gap, beveling of the fractured surfaces) as well as the characteristics of the denture repair resin used (cohesive strength and adhesive strength to the denture base material).23 The resistance of the repaired denture base materials to fracture is not only influenced by the fracture strength but also by the fracture toughness.24-26
Removable dentures fabricated with Eclipse may also fracture. However, it is not possible to repair the denture bases with the same material especially when the patient experiences these problems abroad. Therefore, it is important to investigate the flexural properties of Eclipse after being repaired with the most common repair material which is PMMA. This study was conducted to examine the flexural properties of Eclipse denture base system after being repaired with two different methods, compare with the original intact denture base and draw clinical conclusions. The null hypothesis of this study was that there would be no statistically significant difference in the transverse strength of the two tested materials for repair.
A total of 30 specimens were prepared in a dimension of 65 mm × 10 mm × 3 mm according to ISO 1567:1999.27 A teflon mold with a transparent plexyglass lid was designed to prepare the urethane dimethacrylate (Eclipse, Dentsply, York, PA, USA, Lot No.:720213) specimens. The urethane dimethacrylate dough was sandwiched in this mold and cured in its specific unit (Enterra VLC Curing Unit; Degu Dent GmbH, Hanau, Germany) using the recommended 15 minute polymerization cycle (Fig. 1). After completion of the polymerization, the excess materials were removed by trimming with tungsten carbide burs using a handpiece at low speed. Both sides of the specimens were polished under running water with #320, 400, and 600 grit silicon carbide papers respectively. 20 specimens were sectioned in half for creating two repair groups and remaining 10 specimens were considered as a control group. Repair groups were sectioned in to two pieces from the center with a diamond disc using a handpiece at low speed. The first group was repaired with auto-polymerizing polymer according to the manufacturer's instructions and left on the bench for final polymerization (Paladent RR, Heraeus Kulzer GmbH, Hanau, Germany, Lot No.:012166) and called Group ES. The second group was repaired with the urethane dimethacrylate resin which is a light cured polymer (Eclipse, Dentsply, York, PA, USA) according the manufacturer's instructions and called Group EE. The third group was left intact as a control group and called Group E. Repairs were made in the mould where the specimens were manufactured before. All repair pieces were positioned in the mold with a 2 mm rounded joint gap. All joint surfaces were pumiced before repair for eliminating bonding errors. All repaired specimens were trimmed and polished after repair procedures. Before the fracture transverse strength test all specimens were immersed in distilled water at room temperature (25 ± 2℃) for 15 days.
A 3-point bending test device (MTS Mini-Bionics, model 858, MTS Corporation, Eden Prairie, MN, USA) was used to determine the flexural strengths and flexural moduli. The device consisted of a loading wedge and a pair of adjustable supporting wedges placed 50 mm apart. The specimens were centered on the supporting wedges and the loading wedge was set to travel at a crosshead speed of 5 mm/min engaged at the center of the upper surface of the specimens. Specimens were loaded until fracture occurred. Transverse strengths were calculated using the following equation:
Where: S = transverse strength (N/mm2), P = load at fracture (N), I = distance between the supporting wedges (mm), b = width of the specimen (mm), and d = thickness of the specimen (mm).
The mean displacement, maximum load, flexural modulus and flexural strength values and standard deviations were calculated for each group, and the data were statistically analyzed by the NCSS 2007&PASS 2008 Statistical Software (Kaysville, UT, USA). For the comparison of the parameters of the groups the one way ANOVA test and for the detection of the group engendering the difference the Post Hoc Tukey HDS test was used. The relation between the parameters was evaluated by the Pearson correlation analysis. The results were assessed at 95% confidence interval, at a significance level of P=.05.
There was a statistically significant difference between the mean "displacement", "maximum load before fracture", "flexural strength" and "flexural modulus" values of the three groups (Table 1). The mean values of Group E were statistically significant higher than those of Groups ES and EE, whereas no statistically significant difference was detected between the mean values of Group ES and EE (Table 1).
Since the first introduction of PMMA, additional polymers have been evaluated for denture base applications, but none has proven superior to PMMA.28-30 The residual monomer problem as well as rise in the number of hypersensitivity reactions has made the search and development of hypoallergenic denture base materials necessary. In a previous study, it was reported that Triad VLC denture base material, which is a light cured polymer, exhibited superior transverse strength properties (125.23-14.71 MPa) compared to conventional acrylic resins (97.67-8.83 MPa).31 On the other hand, Machado et al.16 found that PMMA resins showed a higher transverse strength than Triad VLC. This finding might be explained by the presence of the large number of porosities in the Triad VLC material,32 which might also explain why it was reported that the Triad material showed greater staining in tea solution compared to other acrylic resin denture base materials.31
The use of light-polymerized denture base resins is popular, since not only for exhibiting acceptable strength and dimensional stability, but also for relatively complete polymerization without free monomer release. The fracture resistance of denture base polymers has been the subject of many investigations. Various methods have been suggested to test the flexural properties of denture bases.32-36 Testing of the flexural strength and flexural modulus of denture base materials according to ISO 1567 is well accepted.27
Eclipse is a newer hypoallergenic light-polymerized denture base material which helps manipulation of artificial teeth at the evaluation appointment, before final polymerization of the dentures16 and it has been shown that Eclipse exhibited significantly higher flexural and impact strengths as compared to PMMA denture base materials.16,18
The fracture of a resin based prostheses can frequently be encountered in dental practice, caused by fatigue of the base material during function and weakening because of water sorption in the oral environment.5,7-9 Additionally, accidentallydropped or damaged dentures while cleaning is frequently observed especially in the geriatric population where neuromuscular incoordination is present. Therefore, the patients are usually advised to brush the dentures over a filled basin or face cloth to protect them against damage if dropped. Fracture of the denture base, whether for a conventional or implant prosthesis, can be a problematic complication for elderly patients, as they are generally unable to wear the dentures until repaired.37 A broken or cracked denture can be embarrassing and may happen at the most inconvenient times. Therefore, it is very important to repair the dentures as quickly as possible and rescue the patients from this situation.
The goal of the present study was to assess the displacement, maximum load before fracture, flexural strength and modulus of the Eclipse denture base material after being repaired with auto polymerizing acrylic resin or with urethane dimethacrylate polymer and compare with the original control group. The null hypothesis in this study (that there would be no statistical difference when comparing the transverse strengths of the two tested denture base materials for repair) was accepted. Based on the results, it can be stated that both repair materials have failed to restore the displacement, maximum load before fracture, flexural strength and flexural modulus of the original material. It should be pointed out that the repair of the hypoallergenic denture base by the use of auto polymerizing acrylic polymer ends in flexural values as low as one fifth to one sixth of the original strength and moduli. It was also shown that the respective manufacturer-recommended repair is slightly more suitable for the repair of hypoallergenic denture base materials.
The finding of reduced flexural strength and flexural modulus after repair of the denture base in the present study is in agreement with several studies.7,8,19,21-23 It has to be pointed out that the strength of the repaired base is always significantly lower than the intact base as shown previously.38-41 There are several studies showing that flexural strengths of repaired denture base materials had been reduced to percentages such as 22-58%,19 72-91% or 36-65%10 of the intact materials. This finding was in agreement with the maximum estimated repair strength of 75-85% reported in previous studies.8,20-22,42 Therefore, it was pointed out that the repair strengths of the hypoallergenic base materials achieved the level of repaired conventional denture base materials, except for Puran HC, Alldent Sinomer, and Thermo Free.
Polyzois et al.8 reported greater repair strengths for auto polymerizing acrylic resin compared to heat-polymerizing acrylic resin. Although, Dar-Odeh et al.7 reported similar values in transverse strength for auto polymerizing, heat polymerized and light-polymerized resin materials after repair and the results of another study showed even lower flexural properties for light-polymerized repair materials compared to those of auto polymerizing resin,19 no significant differences between the 2 repair groups (repair according to manufacturer's instructions or repair with Versyo. com) were found with respect to the flexural properties in another study.38 The superior repair material was found to be the light polymerizing polymer. The other light-polymerizing material, Microbase repair material, presented a flexural strength and flexural modulus that did not differ significantly from the control group, whereas both autopolymerizing repair materials, Puran CC and Alldent Sinomer N, demonstrated significantly lower flexural strengths and flexural moduli compared to the control group. These findings were in congruence of the results of the present study.
Another factor influencing the success of the repair procedure according to several studies is the width of the gap and the preparation of the fractured surfaces.22,23 In the present investigation, the fracture gap, with a distance of 3 mm between the 2 fragments and a 45 degree bevel of the fractured surfaces of both fragments was prepared, as recommended in other studies.22,23 Ward et al. for example had advised a 45 degree bevel or rounded joint rather than a butt joint of the repair surfaces to improve the fracture strength.22
Eclipse may be a biocompatible material for denture base fabrication. However, it should be emphasized that not every technical lab or dental clinic has the infrastructure for repair with the same material. Although the results of the present study indicate a slightly better but not significant resistance of the light-polymerized repair, the more economic self curing acrylic resin can be recommended as an alternative repair material, keeping in mind the difficulty to find the relevant equipment for light polymerization. However it should be pointed out that in order to reduce a potential allergic reaction induced by the residual monomer of PMMA, repair procedures should be used with same material when possible.
Although in vitro tests may not always reflect intraoral conditions and be predictive of clinical performance, they are valuable and can be applicable to clinical situations.43 The present study involved a limited analysis of mechanical properties for the denture base materials used. Further investigations regarding other properties of these materials are mandatory. To overcome the limitations of the in vitro tests repaired denture base materials must be evaluated intraorally.
Transverse strengths of PMMA and Eclipse denture base materials for the repair of Eclipse denture bases show no differences. However, compared to the intact base any repaired denture base shows lower flexural properties. Therefore, it can be recommended that the more economic self-curing acrylic resin can be used as an alternative repair material for Eclipse denture bases.
References
1. Diwan R. Materials Prescribed in the Management of Edentulous Patients. In : Zarb G, Bolender CL, Eckert SE, editors. Prosthodontic treatment for edentulous Patients: complete dentures and implant-supported prostheses. 12th ed. St. Louis: CV. Mosby;2004. p. 190–207.
2. Meng TR Jr, Latta MA. Physical properties of four acrylic denture base resins. J Contemp Dent Pract. 2005; 6:93–100.
3. Murray MD, Darvell BW. The evolution of the complete denture base. Theories of complete denture retention-a review. Part 1. Aust Dent J. 1993; 38:216–219.
4. Parvizi A, Lindquist T, Schneider R, Williamson D, Boyer D, Dawson DV. Comparison of the dimensional accuracy of injection-molded denture base materials to that of conventional pressure-pack acrylic resin. J Prosthodont. 2004; 13:83–89.
5. Pfeiffer P, Rosenbauer EU. Residual methyl methacrylate monomer, water sorption, and water solubility of hypoallergenic denture base materials. J Prosthet Dent. 2004; 92:72–78.
6. Price CA. A history of dental polymers. Aust Prosthodont J. 1994; 8:47–54.
7. Dar-Odeh NS, Harrison A, Abu-Hammad O. An evaluation of self-cured and visible light-cured denture base materials when used as a denture base repair material. J Oral Rehabil. 1997; 24:755–760.
8. Polyzois GL, Tarantili PA, Frangou MJ, Andreopoulos AG. Fracture force, deflection at fracture, and toughness of repaired denture resin subjected to microwave polymerization or reinforced with wire or glass fiber. J Prosthet Dent. 2001; 86:613–619.
9. Vallittu PK, Lassila VP, Lappalainen R. Evaluation of damage to removable dentures in two cities in Finland. Acta Odontol Scand. 1993; 51:363–369.
10. Beyli MS, von Fraunhofer JA. An analysis of causes of fracture of acrylic resin dentures. J Prosthet Dent. 1981; 46:238–241.
11. Darbar UR, Huggett R, Harrison A. Denture fracture-a survey. Br Dent J. 1994; 176:342–345.
12. McCabe JF, Carrick TE, Chadwick RG, Walls AW. Alternative approaches to evaluating the fatigue characteristics of materials. Dent Mater. 1990; 6:24–28.
13. Diaz-Arnold AM, Vargas MA, Shaull KL, Laffoon JE, Qian F. Flexural and fatigue strengths of denture base resin. J Prosthet Dent. 2008; 100:47–51.
14. Rodford RA. Further development and evaluation of high impact strength denture base materials. J Dent. 1990; 18:151–157.
15. Rodford RA, Braden M. Further observations on high impact strength denture-base materials. Biomaterials. 1992; 13:726–728.
16. Machado C, Sanchez E, Azer SS, Uribe JM. Comparative study of the transverse strength of three denture base materials. J Dent. 2007; 35:930–933.
17. Radzi Z, Abu Kasim NH, Yahya NA, Gan SN. Impact strength of an experimental polyurethane-based polymer. Annal Dent Univ Malaya. 2007; 14:46–51.
18. Machado AL, Puckett AD, Breeding LC, Wady AF, Vergani CE. Effect of thermocycling on the flexural and impact strength of urethane-based and high-impact denture base resins. Gerodontology. 2012; 29:e318–e323.
19. Andreopoulos AG, Polyzois GL. Repair of denture base resins using visible light-cured materials. J Prosthet Dent. 1994; 72:462–468.
20. Thean HP, Chew CL, Goh KI, Norman RD. An evaluation of bond strengths of denture repair resins by a torsional method. Aust Dent J. 1998; 43:5–8.
21. Beyli MS, von Fraunhofer JA. Repair of fractured acrylic resin. J Prosthet Dent. 1980; 44:497–503.
22. Ward JE, Moon PC, Levine RA, Behrendt CL. Effect of repair surface design, repair material, and processing method on the transverse strength of repaired acrylic denture resin. J Prosthet Dent. 1992; 67:815–820.
23. Vallittu PK, Lassila VP, Lappalainen R. Wetting the repair surface with methyl methacrylate affects the transverse strength of repaired heat-polymerized resin. J Prosthet Dent. 1994; 72:639–643.
24. Zappini G, Kammann A, Wachter W. Comparison of fracture tests of denture base materials. J Prosthet Dent. 2003; 90:578–585.
25. Uzun G, Hersek N. Comparison of the fracture resistance of six denture base acrylic resins. J Biomater Appl. 2002; 17:19–29.
26. Phoenix RD, Mansueto MA, Ackerman NA, Jones RE. Evaluation of mechanical and thermal properties of commonly used denture base resins. J Prosthodont. 2004; 13:17–27.
27. Tirapelli C, Ravagnani C, Panzeri Fde C, Panzeric H. Fiber-reinforced composites: effect of fiber position, fiber framework, and wetting agent on flexural strength. Int J Prosthodont. 2005; 18:201–202.
28. Ogle RE, Sorensen SE, Lewis EA. A new visible light-cured resin system applied to removable prosthodontics. J Prosthet Dent. 1986; 56:497–506.
29. Fellman S. Visible light-cured denture base resin used in making dentures with conventional teeth. J Prosthet Dent. 1989; 62:356–359.
30. Khan Z, Haeberle CB. One-appointment construction of an immediate transitional complete denture using visible light-cured resin. J Prosthet Dent. 1992; 68:500–502.
31. Khan Z, von Fraunhofer JA, Razavi R. The staining characteristics, transverse strength, and microhardness of a visible light-cured denture base material. J Prosthet Dent. 1987; 57:384–386.
32. Tan HK, Brudvik JS, Nicholls JI, Smith DE. Adaptation of a visible light-cured denture base material. J Prosthet Dent. 1989; 61:326–331.
33. Nishigawa G, Maruo Y, Oka M, Okamoto M, Minagi S, Irie M, Suzuki K. Effect of plasma treatment on adhesion of self-curing repair resin to acrylic denture base. Dent Mater J. 2004; 23:545–549.
34. Yunus N, Rashid AA, Azmi LL, Abu-Hassan MI. Some flexural properties of a nylon denture base polymer. J Oral Rehabil. 2005; 32:65–71.
35. Hedzelek W, Gajdus P. Comparison of mechanical strength of palatal denture bases made from various plastic materials. Int J Prosthodont. 2006; 19:193–194.
36. Nakamura M, Takahashi H, Hayakawa I. Reinforcement of denture base resin with short-rod glass fiber. Dent Mater J. 2007; 26:733–738.
37. Gonda T, Maeda Y, Walton JN, MacEntee MI. Fracture incidence in mandibular overdentures retained by one or two implants. J Prosthet Dent. 2010; 103:178–181.
38. Pfeiffer P, An N, Schmage P. Repair strength of hypoallergenic denture base materials. J Prosthet Dent. 2008; 100:292–301.
39. Kostoulas I, Kavoura VT, Frangou MJ, Polyzois GL. Fracture force, deflection, and toughness of acrylic denture repairs involving glass fiber reinforcement. J Prosthodont. 2008; 17:257–261.
40. Faot F, da Silva WJ, da Rosa RS, Del Bel Cury AA, Garcia RC. Strength of denture base resins repaired with auto-and visible light-polymerized materials. J Prosthodont. 2009; 18:496–502.
41. Rached RN, Powers JM, Del Bel Cury AA. Repair strength of autopolymerizing, microwave, and conventional heat-polymerized acrylic resins. J Prosthet Dent. 2004; 92:79–82.
42. Minami H, Suzuki S, Kurashige H, Minesaki Y, Tanaka T. Flexural strengths of denture base resin repaired with autopolymerizing resin and reinforcements after thermocycle stressing. J Prosthodont. 2005; 14:12–18.
43. Johnston EP, Nicholls JI, Smith DE. Flexure fatigue of 10 commonly used denture base resins. J Prosthet Dent. 1981; 46:478–483.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download