Abstract
For patients with systemic diseases who face difficulties visiting dental clinics, wearing fixed partial denture in the anterior region on the same day of tooth extraction can reduce the total period of treatment and the number of visits, as well as post-treatment psychological effect on the patient.
Patients with missing teeth present with a loss of aesthetic and functional outcomes. In particular, in case of anterior teeth, there is a great impairment in social activities. Therefore, these patients are in need of immediate prosthodontic restoration after tooth extraction.1 As a usual method, they can wear a provisional removable appliance like a flipper for the lost tooth area, but this may cause a noticeable change in the periodontal structure around the area with resorption of alveolar bone.2 Particularly for patients with severe periodontal disease, wearing a flipper can cause damage to or tilting of nearby teeth, which can cause further loss of teeth and deleterious changes on the periodontal structure. Maintaining the size and form of alveolar socket after tooth extraction similar to pre-extraction condition is an important for esthetic restoration.3
As a solution to such problem, Hopkins was the first to suggest immediate restoration of resin bonded bridge at the moment of extraction.4 Since then, immediate restoration with resin bonded bridge has been a widely studied field. Because it is an anterior region that requires esthetics, a pontic is produced as an ovate type.
The greatest factor to consider after extraction is the space between gingiva and the cervical region of pontic, along with the resorption of alveolar bone. It was reported that when 21 immediate resin bonded bridges were restored, the amount of resorption after extraction was relatively small and the extraction had a low influence in aesthetic outcomes, which may be partially attributed to the severity of periodontal disease before the extraction.5
However, the immediate resin bonded bridge has not been conducted in the missing area more than a single tooth, and such study has not been reported, because of loss of retention, leading to debonding of prosthesis. With reference to the techniques of immediate resin bonded bridge, this case report tried an immediate fixed partial denture in the missing area more than a single tooth. The successful treatment outcomes can be obtained through an appropriate selection of patients and a sufficient analysis at the time of diagnosis in a clinical setting. The current case report discusses matters that should be considered for using an immediate fixed partial denture.
The patient was a 72 year-old woman who had been restricted in movements as a result of a tumor surgery for ovarian cancer and was on a wheelchair. She took medicines including aspirin due to hypertension and diabetes.
The chief complaint was the loss of prosthetic restoration in the maxillary incisors and the mobility in the mandibular incisors. The patient could not smile freely because of the unnatural shape of the incisors. This made her depressed. In her initial dental examination, she was detected with a failure of Maryland bridge in the anterior region along with the upper right lateralis crown fracture, and serious mobility of both lower centralis (Fig. 1).
On radiographs, the left and right mandibular central incisors had destructive bone loss extending to the apical 1/3 of the roots, for which the tooth extraction was unavoidable. Around the left and right mandibular lateral incisors, there was a bone loss extending to the apical 1/2 of the roots (Fig. 2). This was not accompanied by the tooth mobility, and the probing depth was approximately 3 mm. Therefore, the lateral incisors were determined to serve as abutments.
The patient wanted to finish her treatment within 2 visits to the clinic, as it was difficult for her to visit without a caregiver. Therefore, her final treatment goals was to achieve an immediate recovery of aesthetics and function through a synchronous prosthetic restoration immediately after the extraction of hopeless incisors. The immediate restoration was expected to restore psychological condition of the patient with systemic disease as well as the functional one.
On the day of visit, after conducting one visit endodontic treatment of her upper right lateralis and periodontal treatment of the area, a 4-unit prosthesis was designed with the upper right canine, upper right lateralis, and upper left centralis as abutment teeth. When examining the oral cavity, because the gingival biotype was a thick biotype, the amount of gingival recession was predicted to be relatively low. For the lower anterior region, a 4-unit prosthesis with both lower lateralis as abutment teeth was planned to be installed immediately after extracting both lower centralis.
When extraction of the anterior teeth was necessary due to the patient's periodontal disease, many factors had to be considered in order to reduce her number of visits while accounting for the curing of the soft tissues. Because there was a tooth rotation, a change in tooth alignment was required, and it was very important to conduct tooth preparation in the exact, needed amount by accurately predicting the appearance of tooth after treatment. Through diagnostic wax up, the post-treatment appearance was predicted. The diagnostic wax up was copied through Putty (Express STD Putty, 3M ESPE, St. Paul, MN, USA), which was made as an index standard. The next day, the exact amount of the teeth was deleted (Fig. 3). With consideration of gingival recession, the margin was determined to be 1 mm below the gingiva. The tooth preparation of nearby abutment teeth was conducted, and after obtaining final impression using polyvinylsiloxane (Imprint II Garant, 3M ESPE, St. Paul, MN, USA), two temporary single crowns were installed. The thickness of the soft tissue superior to the alveolar crest was directly measured through osseous sounding using a periodontal probe; it was measured as approximately 5 mm. 3-5 mm of soft tissue coverage was ideal for ovate pontic design.6 Because she was taking aspirin, she could not extract her tooth on the day of her visit.
For laboratory work, the lower centralis planned to be extracted were removed from the master model. The removed area was shaped with the approximate outline and predetermined tissue depth. The final prosthesis was designed to form a natural soft-tissue outlook by extending pontic area by 3-4 mm to the extraction socket (Fig. 4). This adaptive design to the pontic site was intended to prevent food impaction and for esthetic and functional result.
On the second day, the final sterilized prosthesis was installed after extraction, and it was checked if it was properly extended to the extraction socket and had a hemostasis effect (Fig. 5). For the abutment tooth, in order to prevent post operative hypersensitivity, desensitizer was applied. After checking the degree of hemostasis effect, setting was done with a RMGI cement (GC FujiCEM II, GC, Tokyo, Japan). The patient was satisfied with installing immediate aesthetic prosthesis at the time of tooth extraction (Fig. 6).
Healing and stabilization of the soft tissue took approximately 2 months. On the follow-up photograph taken 2 months later, there were no findings suggestive of gingival recession (Fig. 7). The patient was much satisfied with the aesthetic outcomes. Moreover, there was stability in the treatment outcome without discomfort or other notable findings during the follow-up period.
A prognosis of the prosthesis in patients undergoing prosthetic restoration after tooth extraction for periodontal disease is associated with the degree of motives for oral hygiene prior to the treatment.7 In this case, the patient was instructed to perform oral hygiene after receiving periodontal treatment prior to prosthodontic therapy. This was helpful for obtaining more predictable outcomes.
Through appropriate periodontal therapy and oral hygiene program, the recurrence of periodontitis and the progression of periodontal tissue disruption can be prevented. It has also been reported that the periodontal therapy is effective for patients undergoing a bridge restoration.8 Therefore, the maintenance of periodontal health through the active oral hygiene and patient education can be helpful for preventing gingival recession. Moreover, the patient in this case was treated to prevent the secondary caries through a regular fluoridation on a periodical visit at a 3-month interval.
Unfortunately, the patient died of the recurrence of disease after the delivery of prosthesis, and the soft tissue changes could not be evaluated after 2 months. Further long-term follow-up studies are needed to examine the stabilization of the soft tissue and the gingival recession.
The total number of visits was reduced, the treatment period was greatly shortened, the patient's hesitation about the extraction process was lessened because the facial structure stayed nearly unchanged, and the patient was able to live without having any negative impact on her social life. The patient gained a huge satisfaction by putting on the immediate aesthetic prosthesis at the time of tooth extraction. There may be some problems such as gingival recession in case of thin gingival biotype, but with thorough consideration of the patient's gingival biotype, prediction of post treatment appearance through diagnostic wax up, and accurate tooth preparation using putty index, the treatment can be a highly predictable one.
Figures and Tables
Fig. 1
Pre-treatment state. Note the failure of Maryland bridge in the maxillary anterior region and severe mobility of both lower centralis. A patient needed both lower centralis extracted.

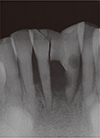
Fig. 2
Initial periapical radiographic image. Note severe bone resorption in the mandibular incisors, and the interproximal resin for periodontal splinting was broken due to tooth mobility.
References
1. Monya Y, Matsumura H, Atsuta M. A two-stage resin-bonded fixed partial denture seated in conjunction with postextraction healing of the alveolar socket: a clinical report. J Prosthet Dent. 1998; 80:4–8.
2. Saunders WP. Resin bonded bridgework: a review. J Dent. 1989; 17:255–265.
3. Hawkins CH, Sterrett JD, Murphy HJ, Thomas JC. Ridge contour related to esthetics and function. J Prosthet Dent. 1991; 66:165–168.
4. Hopkins C. An immediate cantilever Rochette bridge. Br Dent J. 1981; 151:292–295.
5. Al-Wahadni AM, Al-Omari WM. Immediate resin-bonded bridgework: results of a medium-term clinical follow-up study. J Oral Rehabil. 2004; 31:90–94.
6. Korman RP. Enhancing esthetics with a fixed prosthesis utilizing an innovative pontic design and periodontal plastic surgery. J Esthet Restor Dent. 2015; 27:13–28.
7. Valderhaug J. Periodontal conditions and carious lesions following the insertion of fixed prostheses: a 10-year follow-up study. Int Dent J. 1980; 30:296–304.
8. Nyman S, Lindhe J. A longitudinal study of combined periodontal and prosthetic treatment of patients with advanced periodontal disease. J Periodontol. 1979; 50:163–169.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download