Abstract
PURPOSE
To compare the accuracy of marginal and internal adaptation of zirconia (Zr) copings fabricated on anatomic (A), semi-anatomic (SA) and non-anatomic (NA) occlusal surface preparations.
MATERIALS AND METHODS
45 extracted bicuspid teeth were prepared for receiving zirconia crowns, with different occlusal preparation designs A=15, SA=15 & NA=15. The Zr copings were fabricated by using CAD4DENT, CAD/CAM. The copings were adjusted, cemented and were cross sectioned centrally from buccal cusp tip to lingual cusp tip into mesial and distal halves. The copings were examined under electron microscope at ×200 magnification and the measurements were recorded at 9 predetermined areas in micrometers.
RESULTS
Overall mean gap values for the three groups was found to be 155.93±33.98 µm with Anatomical Occlusal preparation design having the least gap value of 139.23±30.85 µm showing the best adaptation among the groups. Post Hoc Tukey's test showed a statistically significant difference (P=.007) between the means of gap for A & NA preparation designs. Measurements recorded at 9 predetermined points showed variations for the three groups.
CONCLUSION
Anatomical occlusal preparation designs resulted in better marginal and internal adaptation of Zr copings. There is a considerable variation between the measured marginal and internal gap values for the Zr copings fabricated by the (CAD4DENT-CAD/CAM). This variation may be associated with the lack of standardization of the preparation of teeth, computerized designing of the coping for each tooth, cement used, uniform pressure application during the cementation of the copings, sectioning of the copings and the microscopic measurements.
The use of zirconia (Zr) as a substructure for all ceramic restorations has increased within the last few years because of the excellent esthetic results and oral biocompatibility. The all ceramic restorations survival in the oral cavity is greatly influenced by its mechanical properties, internal adaptation of the restoration onto the prepared tooth, luting cement used and the marginal seal.1,2,3,4 Poor seal of the crown margins can become a source of periodontal diseases, endodontic inflammation and secondary caries of the abutment teeth because of the plaque accumulation and changing the micro flora. All these changes alone or together may lead to the poor prognosis of the prosthodontic treatment.1,2,3,4,5,6,7,8,9 The presence of marginal gaps in the fixed restorations exposes the luting cement to the saliva intraorally. If the gap is large the dissolution of cement in the oral fluids will also be fast.10 Also, the cement layer between the Zr coping and the tooth can be thicker because of poor adaptation. This compromises the retention and resistance form of the prepared teeth, resulting in loss of stability and potential fracture of the all ceramic crowns.1,2
A margin is considered open when it is visually detectable or if there is a catch between the crown margin and tooth with the tip of a sharp explorer. Clinically, it is very difficult to detect an open margin of less than 80 µm.11 Different researchers have considered 100 µm to 150 µm as clinically acceptable range for the open crown margins.12,13,14,15,16,17 The all ceramic crowns will also have tendency to fracture if the internal space between the fitting surface of the crowns and the prepared tooth is greater than 70 µm.18
Two main fit assessment protocols are described in the literature. One is a destructive protocol, where a specimen or replica is sectioned, followed by microscopic analysis; the second is a nondestructive protocol, whereby only external gap measurements are performed. Conventionally, the marginal and internal gaps of restorations are measured two dimensionally by cutting the restorations into different sections. The measurements between the restoration and the prepared teeth or dies are recorded with the electron microscope from 4 to 24 points.9,18,19,20,21
Research studies involving the adaptation of Zr copings are focused on investigating the effects of preparation angles,22 manufacturing processes,18 cement used for cementation,21 preparation depth differences23 and preparation errors.24 Apparently, the effect of occlusal surface preparation design on the fit of Zr copings has not been reported in the literature. The aim of this study was to investigate the effect of anatomical (A), semi anatomical (SA) and non-anatomical (NA) occlusal surface preparation designs on the degree of marginal and internal adaptation for Zr copings. The null hypothesis was that the different occlusal surface preparations does not affect the marginal and internal adaptation of the Zr copings.
A sample size of 45 sound or minimally restored (and not involving the artificial crown preparation finishing lines) extracted maxillary premolar teeth from adult patients at department of maxillofacial surgery were collected and stored in hydroxide-diluted water. Each tooth was embedded in a gypsum stone Type-II (Shera, Werkstoff-Technologie, GmbH, Germany) base (2 cm × 2 cm), exposing the anatomic crown and 2 mm of the coronal root. The sample was divided into three groups (A, B and C) using a random draw method.
The specimens were divided into three groups of 15 teeth each according to the occlusal surface preparation design. For Group A specimens the occlusal surface was prepared along the anatomical contours of the cusps and fossae with cuspal angulation of approximately 30°. Semi anatomic (cuspal angulation b/w 15°-30°) and non-anatomic (flat-0°) occlusal surface preparations were completed for the Group B and Group C, respectively.25,26 Each tooth was prepared by one prosthodontist for receiving an all-ceramic Zr crown, according to current guidelines/recommendations. These included a 1 mm heavy chamfer with a smooth continuous gingival finishing line, a 5 to 10 degrees combined convergence angle, an occlusal reduction of 2 mm, and axial reduction of 1 mm and rounded and smooth line angles.27,28 A silicone putty index (Ivoclar, Vivadent Inc. Schaan, Liechtenstein) of each tooth was recorded before the preparation of the teeth and was used to provide a mesiodistally sectioned index for verifying the cuspal angulations of the occlusal reductions.
The teeth were then scanned digitally with 3D Digital Scanner (7Series from Dental Wings Inc. Montreal, Canada). Copings were designed using software (C&B Wizard from Dental wings Inc. Montreal, Canada). A cement spacer of 0.01 mm was used for all the copings. The copings were Milled (Engine D15, Yenadent, Istanbul, Turkey) and sintered (HTCT 01/16 Nabertherm machine, Lilienthal, Germany) by one expert technician.
All copings were first examined visually for any defects or retained debris and steam cleaned. The copings were placed on their corresponding prepared teeth and the marginal fit was assessed visually and tactically using a sharp explorer. The internal fit of the copings were verified further by using a fit checker (Occlude, Aerosol Indicator Spray, Pascal Company, Inc., Washington, USA) and adjustments were made using a high speed hand piece with a round diamond bur (#BR31, Mani, Inc., Tochigi, Japan) with water irrigation, if required. These procedures were repeated three times, in order to achieve a uniform contact with the abutment teeth. The internal surface of copings was cleaned carefully with Bego Dousrar using 60 psi sandblasting (Korox 110 & 50 um, special corundum blasting material of 99.6% aluminum oxide). The copings were then cemented with a conventional glass-ionomer cement (Fuji-Cem; GC Int., Tokyo, Japan), using finger pressure initially for seating, excess cement removed with an explorer and an axial force of approximately 50 N (average finger force applied during cementation)29 was applied with a finger to the center of the occlusal surface for 10 minutes.4,6,29 The specimens were then stored in distilled water with a pH of 7. Twenty-four hours after cementation, all of the cemented copings were sectioned axially from buccal cusp tip to palatal cusp tip using water-cooled thin diamond discs in a low-speed straight headpiece (KaVo Dental, GmbH, Biberach, Germany).
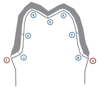
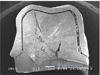
The sectioned specimen halves numbered as a & b were mounted in self cure acrylic resin (Dentsply, Surrey, UK) (Fig. 1) and gold coated (With Fine Coat Ion Sputter JFC-1100, Tokyo, Japan) for placement in a Scanning Electron Microscope (JEOL, JSM-6360LV, Tokyo, Japan), keeping the exposed sectioned surfaces parallel to the base of the microscope (Fig. 2). The copings were examined at 200× magnification by an expert electron microscope technician at 9 predetermined areas (Fig. 3, Table 1). The technician was initially trained for the study with a pilot sample of 3 sectioned copings. The cement thickness between the intaglio surface of the copings and the prepared teeth was measured in micrometers.
3 samples from which the copings were found detached from the teeth on visual and electron microscopic examination were excluded from the study (Fig. 4).
Data was analyzed using SPSS V18.0.1 software package (SPSS, Inc., Chicago, IL, USA). The data was checked for normality and was found satisfactory according to Kolmogorov-Smirnov test (P>.05). The mean of the two halves for each sample tooth was used as the final reading. Analyses included the mean values and Standard deviations for each of the 9 sites and for each group (A, B & C) and comparison of these latter means (95% CIs) across all three independent groups using one-way ANOVA and Tukey's post hoc test. The probability for statistical significance was set at α=.05.
The overall mean gap values for the three groups are presented in Table 2. Group A showed the lowest and the Group C showed the highest mean gap values out of the three groups. Assessment by post hoc Tukey's test showed a statistically significant difference (P=.007) between the A & NA preparation designs (Table 3).
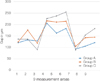
Table 4 shows the mean values for the three groups and overall mean values of the gap thickness at different areas of measurements. The area number 3 (MBAW) and area 7 (MPAW) showed the lowest mean gap values and area number 4 (BCT) and area number 6 (PCT) showed the highest mean gap values measured (Table 4). Results of one way ANOVA showed a statistically significant difference between the three groups for areas number 2 (MBC, P=.011), 3 (MBAW, P=.026), 5 (CG, P=.001), 6 (PCT, P=.000), 8 (MPC, P=.011) and 9 (PMG, P=.004) (Table 4). Comparison of the rest of areas showed a no-significant difference.
Fig. 5 describes the differences in the mean values for the three groups at 9 evaluated regions obtained with electron microscope. The highest difference among the groups was found in the region 6 (PCT) and the least difference was found in the area 1 (BMG).
In the present study the marginal and internal adaptation of the single unit Zr copings manufactured from semi-sintered Zr blocks and cemented on prepared extracted teeth was investigated. To the best of author's knowledge, most of the studies with respect to the adaptation of the Zr copings have been carried out on standardized abutments fabricated from resin or metal alloys such as stainless steel. This study was an attempt to relate the results to the clinical environment using natural teeth instead of using the same sized dies. However, there were some limitations of the study which may have affected the internal and marginal gap such as use of one type of CAD/CAM system, standardization of the preparation of teeth, individual designing of the coping for each tooth, effect of cement used, uniform pressure application during the cementation of the copings, sectioning of the coping with the diamond disk and finally the measurements under the microscope. However, an attempt was made to address to each of the individual issues but this may have affected our results.
There is no universally accepted protocol to access and measure the adaptation of dental restorations. Basically, two different techniques for the preparation of sample for the measurement of the marginal and internal gaps are employed. One of the technique involves the sectioning and destruction of the sample and the other involves measurement without sectioning.4,6,19,21,30,31,32 In the current study bucco lingual sectioning of the sample was done and then measurements for each of the half were recorded and the mean for the sample was obtained. The limitation of using this technique is that it gives a two dimensional view for measuring the thickness of gap in a single section and do not examine 3D (three dimensional) adaptation.20 In a study by Wakabayashi et al.20 the adaptation of the all ceramic crowns was analyzed in a non-destructive technique using mirofocus X-ray CT system. Although he reported several advantages of using the technique the overall mean gap thickness measured (119 ± 7 µm) by this technique was found to be not very significantly different than the other reported studies.1,3,6,21
The data obtained rejects the null hypothesis as the occlusal surface preparations does not affect the marginal and internal adaptation of the Zr copings. The results showed statistically significant difference (P<.05) between the means of gap (at 9 measured regions) for the NA and A occlusal preparations. The mean gap measurement for the non-anatomical preparation 167.32 µm was found to be higher than for the anatomical preparation 139.23 µm and overall mean of gap for the three preparations recorded was 155.93 µm.
Although various studies have reported the fit of Zr copings, the methods of measuring the fit were different hence no direct comparison was possible. The results of all these studies are difficult to interpret and compare with the results of the current study, because of the variations in the sample size and difference in the methods used for the measurements. Several authors have considered a marginal discrepancies between 100 µm to 150 µm to be in a range of clinical acceptance.1,6,14,17,19,21,30,31,32 In the present study, the mean of the buccal marginal gap and lingual marginal gap was found to be 138.16 µm for both, which is slightly higher compared to the results of other studies which are within the range of 120 µm. This variation in the results could be because of the difference in the CAD/CAM system and use of individual teeth for the fabrication of each coping in the present study while other studies utilized standardized dies. With this variation we can also predict that a certain percentage of variation in the fit of zirconia copings exists in clinical cases and is difficult to predict clinically.
The fit of the Zr copings is also affected by the stage it is milled, pre-sintered or post-sintered. In a study by Kohorst et al.19 the post sintered Zr was found to have a better adaptation compared to the pre-sintered. However, Att et al.33 found the pre-sintered Zr to have a better fit compared to the post-sintered.
The milling of post-sintered Zr is difficult compared to the pre-sintered because of its hardness. This can be overcome by designing of the coping with the software in such a way that it compensates for the shrinkage of the pre-sintered Zr after it is sintered.
In the current study, semi-sintered zirconia blocks were used. The semi-sintered block has a chalk-like consistency and is easy to mill in the milling machine. After milling is completed, the substructure is sintered to full density. The size of the milled, pre-sintered coping has to be made larger to compensate for the post sintering shrinkage.
Occlusal surface preparation design influences the retention and resistance form of the crowns and it is recommended that occlusal reduction must be anatomic following the anatomical contours of the cusps and fossae of the occlusal table while preparation of teeth for crowns or abutments for Fixed Partial Dentures.25,26,27,28 The substructure (coping) of a crown should have the same shape so that a standardized layer of ceramic can be applied. The anatomical reduction also represents the removal of less tooth structure with a decreased risk for the dental pulp exposure or injury. However, it is difficult to obtain the correct depth of occlusal preparation following the anatomical contours of the teeth as compared to the flat occlusal reduction despite some specific methodologies to accomplish it. The results of the current study showed that the adaptation of the Zr copings was better on the anatomical occlusal surface preparations compared to the semi anatomic and non-anatomic occlusal preparations. With the results of the current study, it may be hypothesized that with an anatomically correct occlusal reduction the single tooth Zr copings will have satisfactory adaptation with combined features of good retention and resistance form. This may help the clinicians during the preparation of teeth for Zr crowns.
Within the limitations of this study, it was concluded that anatomical occlusal preparation designs results in better marginal and internal adaptation of the Zr copings. No correlation was found between the mean gap values among the anatomic, semi anatomic and non-anatomic occlusal surface preparation designs. There is a considerable variation between the marginal and internal measured gap values for the Zr copings fabricated by the (CAD4DENT-CAD/CAM). This variation may be associated with the effect of standardization of the preparation of teeth, computerized designing of the coping for each tooth, cement used, uniform pressure application during the cementation of the copings, sectioning of the copings and finally the microscopic measurements.
Figures and Tables
Table 1
Details of the 9 areas of measurements for each coping

Table 2
Mean values (standard deviation) of the total gap for the experimental groups measured by the electron microscope (n=42)

Table 3
Comparisons of the means of gap between three types of occlusal preparations by post hoc Tukey test

| Groups | A | B | C |
|---|---|---|---|
| A | 0 | .054 | *.007 |
| B | .054 | 0 | .722 |
| C | .007 | .722 | 0 |
Table 4
Descriptive statistics plus ANOVA results for 9 points of measurements

ACKNOWLEDGEMENTS
The authors would like to acknowledge Mr. Nasr Maflehi for his help in the statistical analysis and College of Dentistry Research Centre / Deanship of Scientific Research at King Saud University for supporting the research project (Reference # IR 0039).
References
1. Abduo J, Lyons K, Swain M. Fit of zirconia fixed partial denture: a systematic review. J Oral Rehabil. 2010; 37:866–876.
2. Beuer F, Aggstaller H, Edelhoff D, Gernet W, Sorensen J. Marginal and internal fits of fixed dental prostheses zirconia retainers. Dent Mater. 2009; 25:94–102.
3. Beuer F, Aggstaller H, Richter J, Edelhoff D, Gernet W. Influence of preparation angle on marginal and internal fit of CAD/CAM-fabricated zirconia crown copings. Quintessence Int. 2009; 40:243–250.
4. Beuer F, Naumann M, Gernet W, Sorensen JA. Precision of fit: zirconia three-unit fixed dental prostheses. Clin Oral Investig. 2009; 13:343–349.
5. Colpani JT, Borba M, Della Bona A. Evaluation of marginal and internal fit of ceramic crown copings. Dent Mater. 2013; 29:174–180.
6. Grenade C, Mainjot A, Vanheusden A. Fit of single tooth zirconia copings: comparison between various manufacturing processes. J Prosthet Dent. 2011; 105:249–255.
7. Wettstein F, Sailer I, Roos M, Hämmerle CH. Clinical study of the internal gaps of zirconia and metal frameworks for fixed partial dentures. Eur J Oral Sci. 2008; 116:272–279.
8. Kohorst P, Junghanns J, Dittmer MP, Borchers L, Stiesch M. Different CAD/CAM-processing routes for zirconia restorations: influence on fitting accuracy. Clin Oral Investig. 2011; 15:527–536.
9. Matta RE, Schmitt J, Wichmann M, Holst S. Circumferential fit assessment of CAD/CAM single crowns-a pilot investigation on a new virtual analytical protocol. Quintessence Int. 2012; 43:801–809.
10. Jacobs MS, Windeler AS. An investigation of dental luting cement solubility as a function of the marginal gap. J Prosthet Dent. 1991; 65:436–442.
11. McLean JW, von Fraunhofer JA. The estimation of cement film thickness by an in vivo technique. Br Dent J. 1971; 131:107–111.
12. Boening KW, Walter MH, Reppel PD. Non-cast titanium restorations in fixed prosthodontics. J Oral Rehabil. 1992; 19:281–287.
13. Fransson B, Oilo G, Gjeitanger R. The fit of metal-ceramic crowns, a clinical study. Dent Mater. 1985; 1:197–199.
14. Kokubo Y, Ohkubo C, Tsumita M, Miyashita A, Vult von Steyern P, Fukushima S. Clinical marginal and internal gaps of Procera AllCeram crowns. J Oral Rehabil. 2005; 32:526–530.
15. Quintas AF, Oliveira F, Bottino MA. Vertical marginal discrepancy of ceramic copings with different ceramic materials, finish lines, and luting agents: an in vitro evaluation. J Prosthet Dent. 2004; 92:250–257.
16. Molin MK, Karlsson SL, Kristiansen MS. Influence of film thickness on joint bend strength of a ceramic/resin composite joint. Dent Mater. 1996; 12:245–249.
17. Tsukada G, Tanaka T, Kajihara T, Torii M, Inoue K. Film thickness and fluidity of various luting cements determined using a trial indentation meter. Dent Mater. 2006; 22:183–188.
18. Moldovan O, Luthardt RG, Corcodel N, Rudolph H. Three-dimensional fit of CAD/CAM-made zirconia copings. Dent Mater. 2011; 27:1273–1278.
19. Kohorst P, Brinkmann H, Li J, Borchers L, Stiesch M. Marginal accuracy of four-unit zirconia fixed dental prostheses fabricated using different computer-aided design/computer-aided manufacturing systems. Eur J Oral Sci. 2009; 117:319–325.
20. Wakabayashi K, Sohmura T, Nakamura T, Kojima T, Kinuta S, Takahashi J, Yatani H. New evaluation method by microfocus radiograph CT for 3D assessment of internal adaptation of all-ceramic crowns. Dent Mater J. 2005; 24:362–367.
21. Gonzalo E, Suárez MJ, Serrano B, Lozano JF. A comparison of the marginal vertical discrepancies of zirconium and metal ceramic posterior fixed dental prostheses before and after cementation. J Prosthet Dent. 2009; 102:378–384.
22. Beuer F, Aggstaller H, Richter J, Edelhoff D, Gernet W. Influence of preparation angle on marginal and internal fit of CAD/CAM-fabricated zirconia crown copings. Quintessence Int. 2009; 40:243–250.
23. Azar MS, Lehmann KM, Dietrich H, Weibrich G, Schmidtmann I, Scheller H. Effect of preparation depth differences on the marginal fit of zirconia crown copings: an in vitro study. Int J Prosthodont. 2011; 24:264–266.
24. Renne W, McGill ST, Forshee KV, DeFee MR, Mennito AS. Predicting marginal fit of CAD/CAM crowns based on the presence or absence of common preparation errors. J Prosthet Dent. 2012; 108:310–315.
25. Oyar P, Ulusoy M, Eskitaşçoğlu G. Finite element analysis of stress distribution in ceramic crowns fabricated with different tooth preparation designs. J Prosthet Dent. 2014; 112:871–877.
26. Motta AB, Pereira LC, Duda FP, Anusavice KJ. Influence of substructure design and occlusal reduction on the stress distribution in metal ceramic complete crowns: 3D finite element analysis. J Prosthodont. 2014; 23:381–389.
27. Shillingburg HT, Sather DA Jr, Wilson EL Jr, Mitchell DL, Blanco LJ, Kessler JC. Fundamentals of fixed prosthodontics. 4th ed. Chicago: Quintessence Pub Co;2012. p. 131–148.
28. Rosenstiel SF, Land MF, Fujimoto J. Tooth preparations for all ceramic restorations. Contemporary Fixed Prosthodontics. St. Louis: Mosby Elsevier;2006. p. 323–330.
29. Black S, Amoore JN. Measurement of forces applied during the clinical cementation of dental crowns. Physiol Meas. 1993; 14:387–392.
30. Quintas AF, Oliveira F, Bottino MA. Vertical marginal discrepancy of ceramic copings with different ceramic materials, finish lines, and luting agents: an in vitro evaluation. J Prosthet Dent. 2004; 92:250–257.
31. Iwai T, Komine F, Kobayashi K, Saito A, Matsumura H. Influence of convergence angle and cement space on adaptation of zirconium dioxide ceramic copings. Acta Odontol Scand. 2008; 66:214–218.
32. Colpani JT, Borba M, Della Bona A. Evaluation of marginal and internal fit of ceramic crown copings. Dent Mater. 2013; 29:174–180.
33. Att W, Komine F, Gerds T, Strub JR. Marginal adaptation of three different zirconium dioxide three-unit fixed dental prostheses. J Prosthet Dent. 2009; 101:239–247.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download