1. Mullon JJ, Burkart KM, Silvestri G, Hogarth DK, Almeida F, Berkowitz D, et al. Interventional pulmonology fellowship accreditation standards: executive summary of the Multisociety Interventional Pulmonology Fellowship Accreditation Committee. Chest. 2017; 151:1114–1121. PMID:
28132754.
2. Colt H. Drainage techniques. In : Light RW, Gary Lee YC, editors. Textbook of pleural diseases. 3rd ed. Boca Raton: CRC Press;2016. p. 534–552.
3. Colt HG, Mathur PN. Manual of pleural procedures. Philadelphia: Lippincott Williams & Wilkins;1999.
4. Pathak V, Allender JE, Grant MW. Management of anticoagulant and antiplatelet therapy in patients undergoing interventional pulmonary procedures. Eur Respir Rev. 2017; 26:170020. PMID:
28724563.

5. Kiefer T. Chest drains in clinical practice. Cham: Springer;2017.
6. Venuta F, Diso D, Anile M, Rendina EA, Onorati I. Chest tubes: generalities. Thorac Surg Clin. 2017; 27:1–5. PMID:
27865321.
7. Mahmood K, Wahidi MM. Straightening out chest tubes: what size, what type, and when. Clin Chest Med. 2013; 34:63–71. PMID:
23411057.
8. Cooke DT, David EA. Large-bore and small-bore chest tubes: types, function, and placement. Thorac Surg Clin. 2013; 23:17–24. PMID:
23206714.
9. Davies HE, Davies RJ, Davies CW. BTS Pleural Disease Guideline Group. Management of pleural infection in adults: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010; 65(Suppl 2):ii41–ii53. PMID:
20696693.

10. Roberts ME, Neville E, Berrisford RG, Antunes G, Ali NJ;. Management of a malignant pleural effusion: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010; 65(Suppl 2):ii32–ii40. PMID:
20696691.

11. MacDuff A, Arnold A, Harvey J;. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010; 65(Suppl 2):ii18–ii31. PMID:
20696690.

12. Rahman NM, Pepperell J, Rehal S, Saba T, Tang A, Ali N, et al. Effect of opioids vs NSAIDs and larger vs smaller chest tube size on pain control and pleurodesis efficacy among patients with malignant pleural effusion: the TIME1 randomized clinical trial. JAMA. 2015; 314:2641–2653. PMID:
26720026.
13. Light RW. Pleural diseases. 6th ed. Philadelphia: Lippincott Williams & Wilkins;2013.
14. McElnay PJ, Lim E. Modern techniques to insert chest drains. Thorac Surg Clin. 2017; 27:29–34. PMID:
27865324.

15. John M, Razi S, Sainathan S, Stavropoulos C. Is the trocar technique for tube thoracostomy safe in the current era? Interact Cardiovasc Thorac Surg. 2014; 19:125–128. PMID:
24648468.
16. Bosman A, de Jong MB, Debeij J, van den Broek PJ, Schipper IB. Systematic review and meta-analysis of antibiotic prophylaxis to prevent infections from chest drains in blunt and penetrating thoracic injuries. Br J Surg. 2012; 99:506–513. PMID:
22139619.

17. Adlakha S, Roberts M, Ali N. Chest tube insertion. Eur Respir Monogr. 2016; 74:229–239.

18. Porcel JM. Pleural ultrasound for clinicians. Rev Clin Esp. 2016; 216:427–435. PMID:
27282205.

19. Porcel JM, Brieva L, Antoni Schoenenberger J. Acute transient ataxia caused by local lidocaine injection during insertion of a pleural catheter. Arch Bronconeumol. 2009; 45:472–473. PMID:
19403227.

20. Havelock T, Teoh R, Laws D, Gleeson F. BTS Pleural Disease Guideline Group. Pleural procedures and thoracic ultrasound: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010; 65(Suppl 2):ii61–ii76. PMID:
20696688.

21. Jones WD, Davies HE. Indwelling pleural catheters. Curr Pulmonol Rep. 2015; 4:1–9.

22. Alraiyes AH, Harris K, Gildea TR. When should an indwelling pleural catheter be considered for malignant pleural effusion? Cleve Clin J Med. 2016; 83:891–894. PMID:
27938513.

23. Bibby AC, Maskell NA. Pleural procedures: intercostal chest drains and indwelling pleural catheters. Br J Hosp Med (Lond). 2011; 72:331–335. PMID:
21727812.

24. Gogakos A, Barbetakis N, Lazaridis G, Papaiwannou A, Karavergou A, Lampaki S, et al. Heimlich valve and pneumothorax. Ann Transl Med. 2015; 3:54. PMID:
25861609.
25. George RS, Papagiannopoulos K. Advances in chest drain management in thoracic disease. J Thorac Dis. 2016; 8(Suppl 1):S55–S64. PMID:
26941971.
26. Porcel JM, Lui MM, Lerner AD, Davies HE, Feller-Kopman D, Lee YC. Comparing approaches to the management of malignant pleural effusions. Expert Rev Respir Med. 2017; 11:273–284. PMID:
28271728.

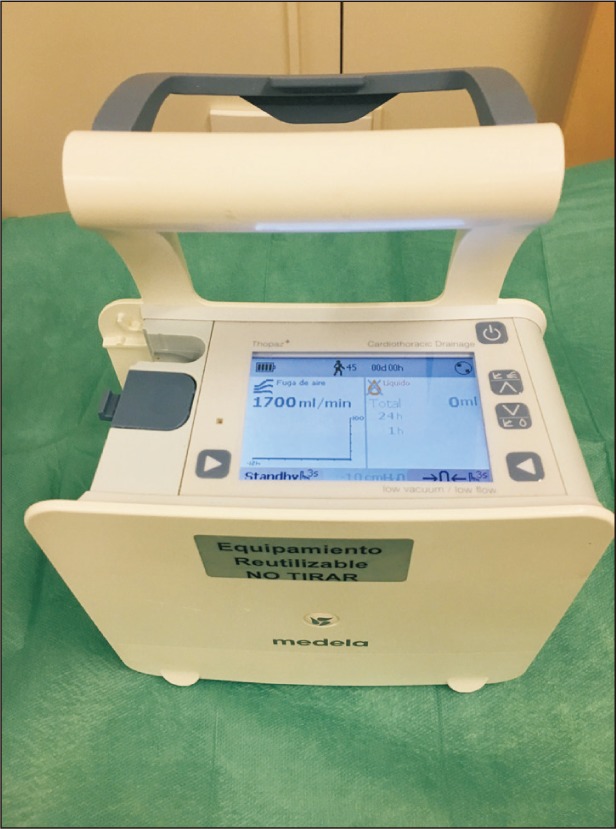
27. Arai H, Tajiri M, Kameda Y, Shiino K, Ando K, Okudela K, et al. Evaluation of a digital drainage system (Thopaz) in over 250 cases at a single site: a retrospective case-control study. Clin Respir J. 2017; 8. 04. DOI:
10.1111/crj.12683. [Epub].

28. Gillen J, Lau C. Permanent indwelling catheters in the management of pleural effusions. Thorac Surg Clin. 2013; 23:63–71. PMID:
23206718.

29. Wahidi MM, Reddy C, Yarmus L, Feller-Kopman D, Musani A, Shepherd RW, et al. Randomized trial of pleural fluid drainage frequency in patients with malignant pleural effusions. The ASAP Trial. Am J Respir Crit Care Med. 2017; 195:1050–1057. PMID:
27898215.

30. Novoa NM, Jimenez MF, Varela G. When to remove a chest tube. Thorac Surg Clin. 2017; 27:41–46. PMID:
27865326.

31. Dugan KC, Laxmanan B, Murgu S, Hogarth DK. Management of persistent air leaks. Chest. 2017; 152:417–423. PMID:
28267436.

32. Davies HE, Gary Lee YC. Pleurodesis. In : Light RW, Gary Lee YC, editors. Textbook of pleural diseases. 3rd ed. Boca Raton: CRC Press;2016. p. 553–569.
33. Kesieme EB, Dongo A, Ezemba N, Irekpita E, Jebbin N, Kesieme C. Tube thoracostomy: complications and its management. Pulm Med. 2012; 2012:256878. PMID:
22028963.

34. Mao M, Hughes R, Papadimos TJ, Stawicki SP. Complications of chest tubes: a focused clinical synopsis. Curr Opin Pulm Med. 2015; 21:376–386. PMID:
26016583.
35. Filosso PL, Guerrera F, Sandri A, Roffinella M, Solidoro P, Ruffini E, et al. Errors and complications in chest tube placement. Thorac Surg Clin. 2017; 27:57–67. PMID:
27865328.

36. Hooper C, Maskell N. BTS Audit Team. British Thoracic Society national pleural procedures audit 2010. Thorax. 2011; 66:636–637. PMID:
21474495.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download