Abstract
Despite progress made in tuberculosis control worldwide, the disease burden and treatment outcome of multidrug-resistant tuberculosis (MDR-TB) patients have remained virtually unchanged. In 2016, the World Health Organization released new guidelines for the management of MDR-TB. The guidelines are intended to improve detection rate and treatment outcome for MDR-TB through novel, rapid molecular testing and shorter treatment regimens. Key changes include the introduction of a new, shorter MDR-TB treatment regimen, a new classification of medicines and updated recommendations for the conventional MDR-TB regimen. This paper will review these key changes and discuss the potential issues with regard to the implementation of these guidelines in South Korea.
Drug-resistant tuberculosis (TB) is still a major threat to global TB control. In 2015, there were approximately 480,000 new cases of multidrug-resistant TB (MDR-TB), an additional 100,000 cases of rifampicin-resistant TB (RR-TB), and approximately 250,000 deaths from MDR/RR-TB1. Successful treatment was achieved in only 52% of MDR/RR-TB patients in the 2013 cohort1. Despite progressive TB control worldwide, the disease burden and treatment outcomes of MDR-TB patients have remained virtually unchanged.
In South Korea, the rate of new MDR-TB cases increased from 1.6% in 1994 to 2.7% in 2004, according to the nationwide surveillance of drug resistance2, and to 2.9% in 2008, according to data from the Health Insurance Review and Assessment Service3. In 2016, a total of 852 MDR-TB, and 59 extensively drug-resistant TB cases were notified4. Until 2011, the published successful treatment rate of MDR-TB patients in South Korea varied from 37.1% to 66.0%567891011. However, the largest retrospective multicenter study (n=1,407 MDR-TB patients) showed a treatment success rate of 45.3% and a default rate of 32.3%9. In 2015, two single-institution retrospective cohort studies suggested treatment outcomes were progressively improving, largely owing to the use of later generation fluoroquinolones and linezolid1213. In 2016, a prospective multicenter study reported an 82.1% of treatment success rate in patients with quinolone-susceptible MDR-TB14.
Recently, there has been improved progress in MDR-TB treatment with the introduction of rapid molecular drug susceptibility testing (DST), new anti-TB drugs (bedaquiline and delamanid), and repurposed drugs (linezolid and clofazimine). Furthermore, a shorter MDR-TB treatment regimen was demonstrated to be effective in several cohorts.
In consideration of these advances, the World Health Organization (WHO) released new guidelines for the management of MDR-TB in May 201615. The guidelines included the introduction of a new, shorter MDR-TB treatment regimen, a new classification of medicines, and updated recommendations for the existing conventional regimen. Until 2016, only one universal strategy had been recommended for MDR-TB. Now, we may choose between two very different strategies; the new, shorter regimen or the conventional, longer regimen.
This paper will review these key changes and discuss the potential issues with the implementation of these guidelines in South Korea.
Programmatic management of drug-resistant tuberculosis (PMDT) is a comprehensive set of strategies and activities including prevention, case detection, care and treatment, surveillance, drug management, and monitoring and evaluation of program performance. These activities should be coordinated by national TB control programs. The WHO has provided guidelines for PMDT since 200616, with updates in 200817 and 201118. The Korean guidelines have been revised in line with the update of the WHO guidelines1920.
The 2016 guideline is specifically focused on the clinical aspects of MDR-TB treatment and does not cover other aspects of policy guidance. The key changes in the 2016 recommendations are as follows.
(1) The recommendation for the use of rapid diagnostics for rifampicin resistance was changed from a conditional recommendation with very low quality evidence (2011) to a strong recommendation with high evidential certainty (2016).
(2) A shorter MDR-TB treatment regimen was newly recommended under specific conditions.
(3) Medicines used in the conventional (longer) MDR-TB treatment regimen were reclassified.
(4) The optimal composition of the conventional MDR-TB treatment regimen was updated.
(5) Evidence-based recommendations on the role of surgery were newly included.
Furthermore, MDR-TB treatment is recommended for all patients with RR-TB, regardless of confirmed isoniazid resistance. Specific recommendations were made for the treatment of children with MDR/RR-TB. However, there was no change in the duration of the conventional MDR-TB regimen or in the role of new drugs (bedaquiline and delamanid).
This paper will focus on the recommendations pertaining to the new classification of anti-TB drugs, the composition of the conventional regimen, and the shorter MDR-TB regimen.
Previous WHO guidelines classified anti-TB drugs into five groups by efficacy, experience of use, safety, and general drug class. The guidelines recommended to choose a drug in a step-down manner, from group 1 to group 5. The five-group classification originated in the 2006 guidelines16. Although minor modifications were made in 200817, 201118, and 201421, the rationale for these classifications has not been changed.
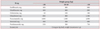
In the 2016 guidelines, medicines used for the conventional MDR-TB regimen were reclassified in a hierarchical order from group A to group D (Table 1)15. Medicines in groups A, B, and C were classified as “core second-line agents,” while medicines in group D were classified as “add-on agents” that were not part of the core second-line agents.
Some changes were made within each classification as follows.
(1) The rankings of fluoroquinolones and second-line injectable drugs were swapped.
Fluoroquinolones are the backbone of MDR-TB treatment regimens, with bactericidal and sterilizing properties, as well as a good safety profile. Many studies have demonstrated that use of fluoroquinolones was the top predictor of favorable treatment outcome of MDR-TB patients22232425. In contrast, the injectable drugs have only bactericidal properties and their safety profile is lower. For these reasons, fluoroquinolones were placed in group A and the injectable drugs in group B.
(2) Linezolid and clofazimine were reclassified as core second-line agents in group C, and p-aminosalicylic acid (PAS) was reclassified as an add-on agent in group D. Linezolid has demonstrated its efficacy on MDR-TB in several meta-analyses2627 and two randomized controlled trials282930. Clofazimine is a core drug in the shorter MDR-TB regimen and likely contributes to the sterilizing function of MDR-TB regimens, where pyrazinamide is not effective15. Although, consistent evidence was not found in three meta-analysis studies of the efficacy of clofazimine in MDR-TB treatment313233, a single randomized controlled trial demonstrated treatment benefits associated with clofazimine34. Based on the growing evidences for anti-TB efficacy, linezolid and clofazimine were placed in group C. PAS has been downgraded to group D3 because its safety and tolerability is worse compare to other drugs in group 4.
(3) Clarithromycin and other macrolides are no longer recommended for MDR-TB treatment. Mycobacterium tuberculosis is intrinsically resistant to the macrolide class of antibiotics, whose efficacy in MDR-TB treatment was not demonstrated in clinical studies. Furthermore, there is a risk of QT prolongation if given in combination with other drugs such as moxifloxacin, clofazimine, bedaquiline, or delamanid. Therefore, the WHO recommended that clarithromycin and azithromycin not be included in the MDR-TB regimens.
(4) Bedaquiline and delamanid were classified in a unique group, D2. Considering the importance of treating intractable MDR-TB, both drugs were granted accelerated approval primarily based on the evidences from phase II clinical trials. Therefore, the level of evidence for efficacy and safety of both drugs remains very limited to date. In the 2016 guideline, the WHO recommended to maintain the previous interim guidance on the use of these medicines3536 until complete phase III data were available. Both drugs have been recommended when an effective and reasonably well-tolerated MDR-TB regimen could not be composed with conventional second-line drugs.
The classification of anti-TB drugs provides a crucial clue for determining the priority of drug selection. There are some concerns about adopting the new WHO drug classifications in South Korea. The primary concern is the rankings of two repurposed drugs (linezolid and clofazimine) in group C and two new drugs (bedaquiline and delamanid) in group D2. According to the new classification, linezolid and clofazimine should be selected prior to bedaquiline and delamanid. However, until now, there has been limited clinical evidence that compares the effectiveness and safety of those agents. Some experts proposed rankings that differ from the WHO guidelines37. The proposed rankings indicate that linezolid, bedaquiline, and delamanid are placed in group 2, and clofazimine in group 5. The recently published endTB guidelines also suggest maintaining the existing classification of drugs until the WHO's interim guidance on bedaquiline and delamanid is revised38.
Despite the relatively excellent anti-TB effect, linezolid causes serious adverse effects, such as peripheral neuropathy and bone marrow suppression. Clofazimine is still doubtful as an anti-TB drug and may cause skin hyperpigmentation that can occur in almost Korean patients. Furthermore, both linezolid and clofazimine are not yet approved as anti-TB drugs in South Korea; drug cost, accessibility, and the availability of both drugs could be another barrier. Although bedaquiline and delamanid are still classified as additional agents, their priorities are likely to be changed with accumulating evidences and experiences. For these reasons, the new Korean guideline, which is published in May 2017, maintains the previous five-group classification of anti-TB drugs until more evidences are available39.
The WHO also updated its recommendations on the optimal composition of the conventional regimen. The WHO recommends that the MDR-TB regimen should be composed of at least five drugs that are likely to be effective during the intensive phase, including pyrazinamide and four core secondline drugs. Core second-line drugs are added to the regimen in the following order: first a fluoroquinolone (group A), followed by a second-line injectable drug (group B), and at least two drugs from group C. If an effective regimen cannot be composed from groups A, B, and C, a drug from group D2 or D3 may be added to the regimen to bring the total number of drugs to five.
Compared to the 2011 recommendations, there are notable changes to the number of effective drugs and counting pyrazinamide based on the likely effectiveness. In 2011, the WHO recommended a regimen of at least four second-line drugs that are likely to be effective, as well as pyrazinamide (irrespective of its likely effectiveness). This recommendation was based on an individual patient meta-analysis of 9,153 cases with MDR-TB; treatment was most successful when four effective drugs were used in the intensive phase in patients with MDR-TB who were not previously treated with second-line drugs24.
Since the 2011 guidelines were published, there have been several cohort studies that examined the impact of number of effective drugs and pyrazinamide susceptibility on the outcome of MDR-TB. A 2012 retrospective study in Hong Kong demonstrated that pyrazinamide users with documented pyrazinamide susceptibility were more likely to have treatment success compared to non-pyrazinamide users and pyrazinamide users with pyrazinamide-resistant organisms40. In Peru, a 2015 retrospective study demonstrated that there was no benefit of pyrazinamide when the drug was unlikely to be effective41. Several studies demonstrated better outcomes with respect to mortality rates, treatment success, recurrent TB, and rates of sputum conversion in patients who received at least five likely effective drugs compared to four likely effective drugs4243444546.
Given these findings, the WHO updated the number of likely effective drugs in the intensive phase from four to five. When pyrazinamide resistance is documented, pyrazinamide may be discontinued and additional drugs, from group C or D, may be added to bring the total to five.
The new Korean guideline updates the number of effective drugs in intensive phase in accordance with the 2016 WHO guideline, but maintains previous recommendation on the composition of MDR-TB regimen 39. The new Korean guideline recommends that the MDR-TB regimen should be composed of at least five anti-TB drugs that are likely to be effective during the intensive phase. The MDR-TB regimen should include at least pyrazinamide, a fluoroquinolone, an injectable anti-TB drug, prothionamide and either cycloserine or PAS.
shorter MDR-TB treatment regimen, called the Bangladeshi regimen, demonstrated promising results in an observational cohort study in Bangladesh. The relapse-free cure rate was 87.9% in a cohort of 206 MDR-TB patients47 and 84.4% in an expanded cohort of 515 MDR-TB patients48. To verify the reproducibility and generalizability of the Bangladeshi regimen, the WHO and International Union Against Tuberculosis and Lung Disease conducted two approaches in parallel. The first is conducting prospective cohort studies in Africa and Asia. The second is conducting a prospective randomized study, STREAM 1. Recruitment to STREAM 1 was completed in 2015 and results are expected early in 2018. Pilot studies in Niger49 and Cameroon50, with minor modification of the Bangladeshi regimen, also demonstrated consistently high cure rates. The WHO proceeded with the evidentiary assessment, given the results from Africa and Asia. Overall treatment success in patients treated with the shorter MDR-TB regimen (>1,100 patients) was 90.3% compared to 78.3% in patients (>5,800) treated with conventional regimens15. Based on this analysis, the WHO now recommends the shorter MDR-TB regimen as a general strategy for MDR-TB treatment.
The shorter MDR-TB regimen recommended by the WHO consists of a 4–6-month intensive phase with kanamycin, moxifloxacin, ethionamide, clofazimine, pyrazinamide, high-dose isoniazid, ethambutol, and a 5-month continuation phase with moxifloxacin, clofazimine, pyrazinamide, and ethambutol. This differs slightly from the Bangladeshi regimen because gatifloxacin has been replaced by moxifloxacin. Notably, the dose of moxifloxacin is higher than the standard dose. The recommended drug dosages for the shorter MDRTB regimen are shown in Table 251.
4–6 Km-Mfx-Pto-Cfz-Z-Hhigh-dose-E / 5 Mfx-Cfz-Z-E
There is a risk for acquiring further drug-resistance if the shorter regimen is used on patients who are already resistant to the core second-line drugs. To avoid this, the WHO provided strict eligibility criteria for the shorter MDR-TB regimen52. The shorter regimen is recommended for patients with RR-TB or MDR-TB who were not previously treated with secondline drugs and do not have resistance to fluoroquinolones and second-line injectable drugs. The WHO also recommends the use of a novel molecular test (MTBDRsl test) for eligibility screening52, which detects resistance to fluoroquinolones and second-line injectable drugs. However, in the absence of novel molecular testing, patients who are highly unlikely to be infected with resistant strains based on their history of exposure and recent representative surveillance data may also be eligible for the shorter MDR-TB regimen.
There are several concerns about the effectiveness of the shorter regimen in South Korea. One major concern is that the additional drug resistance rate in MDR-TB patients is high in South Korea. High levels of drug resistance in South Korea have been reported in several retrospective MDR-TB cohort studies. Additional resistance to pyrazinamide, ofloxacin, and kanamycin was 26.2%–59%, 16.6%–47.5%, and 13.3%–25%, respectively3891011. A recent regional survey of drug resistance in South Korea demonstrated that strains from MDR-TB patients had additional resistance to pyrazinamide (35.7%), fluoroquinolones (26.2%), and second-line injectable drugs (19.3%)53. Rapid DSTs detecting fluoroquinolone and injectable drug resistance, such as MTBDRsl test, is a prerequisite for identifying patients with MDR-TB eligible for the shorter treatment regimen. Its efficacy was demonstrated in small number of patients in South Korea52, but it has not yet been available in routine practice. Considering the high levels of additional drug resistance, the shorter MDR-TB treatment regimen may not be feasible; instead, an individually tailored regimen based on the results of molecular54 and phenotypic DST55 and, if possible, therapeutic drug monitoring56 may be more appropriate in MDR-TB patients in South Korea. There are recent reports with similar concerns in Europe and Latin America5758. It may be challenging to implement the shorter MDR-TB regimen in the countries with high levels of drug resistance.
Favorable treatment outcomes with the shorter MDR-TB regimen were observed in the studies within operational research conditions. However, directly observed therapy is not implemented and the patient management system is still weak in South Korea. In a large retrospective MDR-TB cohort study in 2008, the default rate was 32%9. The number of drugs in the shorter regimen is more than that of conventional regimen. A man weighing ≥50 kg would take 23 tablets and 1 injectable drug each day. Skin pigmentation, an expected side effect of clofazimine, could be occurred in almost all Korean patients. A large number of pills and expected side effect may cause intolerance and subsequently poor treatment adherence. Although the shorter regimen is a tolerable, safe, and patient-friendly regimen in other settings, there are concerns about tolerance and adherence due to the weak patient management system in South Korea. For these reasons, the new Korean guideline suggests that the shorter regimen is not a general strategy for MDR-TB treatment in South Korea but can be used in selected patients39.
Previously, diagnosis of MDR-TB was largely dependent upon phenotypic, culture-based methods and the majority of MDR-TB patients received the conventional regimen for a minimum of 20 months. The 2016 WHO guidelines suggest that a paradigm shift is underway and we are at a turning point in MDR-TB management. This shift has centered largely on rapid diagnosis and effective treatment through the use of novel rapid diagnostic tests and a shorter treatment regimen. These changes are welcome, but there are some controversial challenges to adopting the 2016 WHO guidelines in South Korea. The key concerns are the applicability of the new classifications of anti-TB drugs and the shorter MDR-TB regimen in South Korea. Current controversies regarding the 2016 WHO guidelines could be resolved with further evidence from ongoing and future studies.
Figures and Tables
Table 1

*Medicines in groups A and C are shown by decreasing order of usual preference for use. †Streptomycin may substitute other injectable agents when the other three cannot be used. ‡Carbapenems and clavulanate are meant to be used together; clavulanate is only available in formulations combined with amoxicillin.
Table 2
Drug dosages for the shorter MDR-TB treatment regimen51
References
1. World Health Organization. Global tuberculosis report 2016. WHO/HTM/TB/2016.13 [Internet]. Geneva: World Health Organization;2016. cited 2017 May 1. Available from: http://www.who.int/tb/publications/global_report/en.
2. Bai GH, Park YK, Choi YW, Bai JI, Kim HJ, Chang CL, et al. Trend of anti-tuberculosis drug resistance in Korea, 1994–2004. Int J Tuberc Lung Dis. 2007; 11:571–576.
3. Park YS, Hong SJ, Boo YK, Hwang ES, Kim HJ, Cho SH, et al. The national status of tuberculosis using nationwide medical records survey of patients with tuberculosis in Korea. Tuberc Respir Dis. 2012; 73:48–55.
4. Korea Centers for Disease Control & Prevention. Annual report on the notified tuberculosis patients in Korea 2016 [Internet]. Cheongju: Korea Centers for Disease Control & Prevention;2017. cited 2017 May 1. Available from: http://tbzero.cdc.go.kr.
5. Kim HJ, Hong YP, Kim SJ, Lew WJ, Lee EG. Ambulatory treatment of multidrug-resistant pulmonary tuberculosis patients at a chest clinic. Int J Tuberc Lung Dis. 2001; 5:1129–1136.
6. Park SK, Lee WC, Lee DH, Mitnick CD, Han L, Seung KJ. Self-administered, standardized regimens for multidrug-resistant tuberculosis in South Korea. Int J Tuberc Lung Dis. 2004; 8:361–368.
7. Kim HR, Hwang SS, Kim HJ, Lee SM, Yoo CG, Kim YW, et al. Impact of extensive drug resistance on treatment outcomes in non-HIV-infected patients with multidrug-resistant tuberculosis. Clin Infect Dis. 2007; 45:1290–1295.
8. Kwon YS, Kim YH, Suh GY, Chung MP, Kim H, Kwon OJ, et al. Treatment outcomes for HIV-uninfected patients with multidrug-resistant and extensively drug-resistant tuberculosis. Clin Infect Dis. 2008; 47:496–502.
9. Kim DH, Kim HJ, Park SK, Kong SJ, Kim YS, Kim TH, et al. Treatment outcomes and long-term survival in patients with extensively drug-resistant tuberculosis. Am J Respir Crit Care Med. 2008; 178:1075–1082.
10. Park JK, Koh WJ, Kim DK, Kim EK, Kim YI, Kim HJ, et al. Treatment outcomes and prognostic factors in patients with multidrug-resistant tuberculosis in Korean private hospitals. Tuberc Respir Dis. 2010; 69:95–102.
11. Jeon DS, Shin DO, Park SK, Seo JE, Seo HS, Cho YS, et al. Treatment outcome and mortality among patients with multidrug-resistant tuberculosis in tuberculosis hospitals of the public sector. J Korean Med Sci. 2011; 26:33–41.
12. Kwak N, Kim HR, Yoo CG, Kim YW, Han SK, Yim JJ. Changes in treatment outcomes of multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2015; 19:525–530.
13. Jeong BH, Jeon K, Park HY, Kwon OJ, Lee KS, Kim HK, et al. Outcomes of pulmonary MDR-TB: impacts of fluoroquinolone resistance and linezolid treatment. J Antimicrob Chemother. 2015; 70:3127–3133.
14. Kang YA, Shim TS, Koh WJ, Lee SH, Lee CH, Choi JC, et al. Choice between levofloxacin and moxifloxacin and multidrug-resistant tuberculosis treatment outcomes. Ann Am Thorac Soc. 2016; 13:364–370.
15. World Health Organization. WHO treatment guidelines for drug-resistant tuberculosis, 2016 update. WHO/HTM/TB/2016.04 [Internet]. Geneva: World Health Organization;2016. cited 2017 May 1. Available from: http://www.who.int/tb/areas-of-work/drug-resistant-tb/treatment/resources/en/.
16. World Health Organization. Guidelines for the programmatic management of drug-resistant tuberculosis. WHO/HTM/TB/2006.361 [Internet]. Geneva: World Health Organization;2016. cited 2017 May 1. Available from: http://www.who.int/tb/areas-of-work/drug-resistant-tb/programmatic_guidelines_for_mdrtb/en/.
17. World Health Organization. Guidelines for the programmatic management of drug-resistant tuberculosis, emergency update 2008. WHO/HTM/TB/2008.402 [Internet]. Geneva: World Health Organization;2008. cited 2017 May 1. Available from: http://www.who.int/tb/publications/tb-drugresistance-guideline/en/.
18. World Health Organization. Guidelines for the programmatic management of drug-resistant tuberculosis: 2011 update. WHO/HTM/TB/2011.6 [Internet]. Geneva: World Health Organization;2011. cited 2017 May 1. Available from: http://www.who.int/tb/areas-of-work/drug-resistant-tb/programmatic_guidelines_for_mdrtb/en/.
19. Jeon D. Medical management of drug-resistant tuberculosis. Tuberc Respir Dis. 2015; 78:168–174.
20. Park JS. Issues related to the updated 2014 Korean guidelines for tuberculosis. Tuberc Respir Dis. 2016; 79:1–4.
21. World Health Organization. Companion handbook to the WHO guidelines for the programmatic management of drug-resistant tuberculosis. WHO/HTM/TB/2014.11 [Internet]. Geneva: World Health Organization;2014. cited 2017 May 1. Available from: http://www.who.int/tb/publications/pmdt_companionhandbook/en/.
22. Johnston JC, Shahidi NC, Sadatsafavi M, Fitzgerald JM. Treatment outcomes of multidrug-resistant tuberculosis: a systematic review and meta-analysis. PLoS One. 2009; 4:e6914.
23. Kim DH, Kim HJ, Park SK, Kong SJ, Kim YS, Kim TH, et al. Treatment outcomes and survival based on drug resistance patterns in multidrug-resistant tuberculosis. Am J Respir Crit Care Med. 2010; 182:113–119.
24. Ahuja SD, Ashkin D, Avendano M, Banerjee R, Bauer M, Bayona JN, et al. Multidrug resistant pulmonary tuberculosis treatment regimens and patient outcomes: an individual patient data meta-analysis of 9,153 patients. PLoS Med. 2012; 9:e1001300.
25. Falzon D, Gandhi N, Migliori GB, Sotgiu G, Cox HS, Holtz TH, et al. Resistance to fluoroquinolones and second-line injectable drugs: impact on multidrug-resistant TB outcomes. Eur Respir J. 2013; 42:156–168.
26. Cox H, Ford N. Linezolid for the treatment of complicated drug-resistant tuberculosis: a systematic review and meta-analysis. Int J Tuberc Lung Dis. 2012; 16:447–454.
27. Sotgiu G, Centis R, D’Ambrosio L, Alffenaar JW, Anger HA, Caminero JA, et al. Efficacy, safety and tolerability of linezolid containing regimens in treating MDR-TB and XDR-TB: systematic review and meta-analysis. Eur Respir J. 2012; 40:1430–1442.
28. Lee M, Lee J, Carroll MW, Choi H, Min S, Song T, et al. Linezolid for treatment of chronic extensively drug-resistant tuberculosis. N Engl J Med. 2012; 367:1508–1518.
29. Lee M, Cho SN, Barry CE 3rd, Song T, Kim Y, Jeong I. Linezolid for XDR-TB: final study outcomes. N Engl J Med. 2015; 373:290–291.
30. Tang S, Yao L, Hao X, Zhang X, Liu G, Liu X, et al. Efficacy, safety and tolerability of linezolid for the treatment of XDR-TB: a study in China. Eur Respir J. 2015; 45:161–170.
31. Dey T, Brigden G, Cox H, Shubber Z, Cooke G, Ford N. Outcomes of clofazimine for the treatment of drug-resistant tuberculosis: a systematic review and meta-analysis. J Antimicrob Chemother. 2013; 68:284–293.
32. Gopal M, Padayatchi N, Metcalfe JZ, O’Donnell MR. Systematic review of clofazimine for the treatment of drug-resistant tuberculosis. Int J Tuberc Lung Dis. 2013; 17:1001–1007.
33. Chang KC, Yew WW, Tam CM, Leung CC. WHO group 5 drugs and difficult multidrug-resistant tuberculosis: a systematic review with cohort analysis and meta-analysis. Antimicrob Agents Chemother. 2013; 57:4097–4104.
34. Tang S, Yao L, Hao X, Liu Y, Zeng L, Liu G, et al. Clofazimine for the treatment of multidrug-resistant tuberculosis: prospective, multicenter, randomized controlled study in China. Clin Infect Dis. 2015; 60:1361–1367.
35. World Health Organization. The use of bedaquiline in the treatment of multidrug-resistant tuberculosis: interim policy guidance. WHO/HTM/TB/2013.6 [Internet]. Geneva: World Health Organization;2013. cited 2017 May 1. Available from: http://www.who.int/tb/publications/tb-drugresistance-guideline/en/.
36. World Health Organization. The use of delamanid in the treatment of multidrug-resistant tuberculosis: interim policy guidance. WHO/HTM/TB/2014.23 [Internet]. Geneva: World Health Organization;2014. cited 2017 May 1. Available from: http://www.who.int/tb/publications/tb-drugresistance-guideline/en/.
37. Caminero JA, Scardigli A. Classification of antituberculosis drugs: a new proposal based on the most recent evidence. Eur Respir J. 2015; 46:887–893.
38. endTB clinical and programmatic guide for patient management with new TB drugs. Version 3.3, 24/10/2016 [Internet]. endTB;2016. cited 2017 May 1. Available from: http://www.endtb.org/resources/endtb-clinical-guide-v33.
39. Joint Committee for the Revision of Korean Guidelines for Tuberculosis, Korean Centers for Disease Control and Prevention. Korean guidelines for tuberculosis. 3rd ed. Seoul and Cheongwon: Joint Committee for the Revision of Korean Guidelines for Tuberculosis, Korea Centers for Disease Control and Prevention;2017.
40. Chang KC, Leung CC, Yew WW, Leung EC, Leung WM, Tam CM, et al. Pyrazinamide may improve fluoroquinolone-based treatment of multidrug-resistant tuberculosis. Antimicrob Agents Chemother. 2012; 56:5465–5475.
41. Franke MF, Becerra MC, Tierney DB, Rich ML, Bonilla C, Bayona J, et al. Counting pyrazinamide in regimens for multidrug-resistant tuberculosis. Ann Am Thorac Soc. 2015; 12:674–679.
42. Mitnick CD, Franke MF, Rich ML, Alcantara Viru FA, Appleton SC, Atwood SS, et al. Aggressive regimens for multidrug-resistant tuberculosis decrease all-cause mortality. PLoS One. 2013; 8:e58664.
43. Franke MF, Appleton SC, Mitnick CD, Furin JJ, Bayona J, Chalco K, et al. Aggressive regimens for multidrug-resistant tuberculosis reduce recurrence. Clin Infect Dis. 2013; 56:770–776.
44. Velasquez GE, Becerra MC, Gelmanova IY, Pasechnikov AD, Yedilbayev A, Shin SS, et al. Improving outcomes for multidrug-resistant tuberculosis: aggressive regimens prevent treatment failure and death. Clin Infect Dis. 2014; 59:9–15.
45. Yuen CM, Kurbatova EV, Tupasi T, Caoili JC, Van Der Walt M, Kvasnovsky C, et al. Association between regimen composition and treatment response in patients with multidrug-resistant tuberculosis: a prospective cohort study. PLoS Med. 2015; 12:e1001932.
46. Ahmad Khan F, Gelmanova IY, Franke MF, Atwood S, Zemlyanaya NA, Unakova IA, et al. Aggressive regimens reduce risk of recurrence after successful treatment of MDR-TB. Clin Infect Dis. 2016; 63:214–220.
47. Van Deun A, Maug AK, Salim MA, Das PK, Sarker MR, Daru P, et al. Short, highly effective, and inexpensive standardized treatment of multidrug-resistant tuberculosis. Am J Respir Crit Care Med. 2010; 182:684–692.
48. Aung KJ, Van Deun A, Declercq E, Sarker MR, Das PK, Hossain MA, et al. Successful ‘9-month Bangladesh regimen’ for multidrug-resistant tuberculosis among over 500 consecutive patients. Int J Tuberc Lung Dis. 2014; 18:1180–1187.
49. Piubello A, Harouna SH, Souleymane MB, Boukary I, Morou S, Daouda M, et al. High cure rate with standardised short-course multidrug-resistant tuberculosis treatment in Niger: no relapses. Int J Tuberc Lung Dis. 2014; 18:1188–1194.
50. Kuaban C, Noeske J, Rieder HL, Ait-Khaled N, Abena Foe JL, Trebucq A. High effectiveness of a 12-month regimen for MDR-TB patients in Cameroon. Int J Tuberc Lung Dis. 2015; 19:517–524.
51. World Health Organization. Frequently asked questions about the implementation of the new WHO recommendation on the use of the shorter MDR-TB regimen under programmatic conditions. Version: 20 December 2016 [Internet]. Geneva: World Health Organization;2016. cited 2017 May 1. Available from: http://www.who.int/tb/areas-of-work/drug-resistant-tb/treatment/resources/en/.
52. World Health Organization. Policy guidance on the molecular second-line line-probe assay. WHO/HTM/TB/2016.07 [Internet]. Geneva: World Health Organization;2016. cited 2017 May 1. Available from: http://www.who.int/tb/areas-of-work/drug-resistant-tb/treatment/resources/en/.
53. Mok JH, Kang BH, Lee T, Lee HK, Jang HJ, Cho YJ, et al. Additional drug resistance patterns among multidrug-resistant tuberculosis patients in Korea: implications for regimen design. J Korean Med Sci. 2017; 32:636–641.
54. Jeong HY, Kim H, Kwon S, Ryoo S. Evaluation of the GenoType(R) MTBDRsl assay in Korean patients with MDR or XDR tuberculosis. Infect Dis (Lond). 2016; 48:361–366.
55. Kim SC, Jeon BY, Kim JS, Choi IH, Kim J, Woo J, et al. Performance of the BacT Alert 3D System versus solid media for recovery and drug susceptibility testing of Mycobacterium tuberculosis in a tertiary hospital in Korea. Tuberc Respir Dis. 2016; 79:282–288.
56. Heysell SK, Moore JL, Peloquin CA, Ashkin D, Houpt ER. Outcomes and use of therapeutic drug monitoring in multidrug-resistant tuberculosis patients treated in virginia, 2009–2014. Tuberc Respir Dis. 2015; 78:78–84.
57. Sotgiu G, Tiberi S, D’Ambrosio L, Centis R, Alffenaar JW, Caminero JA, et al. Faster for less: the new “shorter” regimen for multidrug-resistant tuberculosis. Eur Respir J. 2016; 48:1503–1507.
58. Lange C, Duarte R, Frechet-Jachym M, Guenther G, Guglielmetti L, Olaru ID, et al. Limited benefit of the new shorter multidrug-resistant tuberculosis regimen in Europe. Am J Respir Crit Care Med. 2016; 194:1029–1031.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download