Abstract
Objective
The aims of this study were to evaluate the relationship between the detachment force and bonding resin surface are and to determine the resin bonding surface area that would provide adequate bonding strength with minimum resin volume.
Methods
One hundred and sixty human premolars were randomly divided into 4 groups of 40 teeth each. The diameter of the resin surface area in each group was as follows: group 1, 1.5 mm; group 2, 2.5 mm; group 3, 3.5 mm; and group 4, 4.5 mm. Respond Dead Soft straight (length 0.0175 inch) was used to fabricate the retainers, and Transbond™ XT was used to fix the retainers to the tooth surfaces. A pair of teeth was embedded in acrylic blocks for each specimen. Thus, each group comprised 20 samples. Fixed retainers were bonded to the teeth, and vertical force was applied at the middle of wire. The force was measured using a universal testing machine.
Relapse after orthodontic treatment is a frequent, yet unpredictable, occurence.1-3 A previous study reported that relapse occurs most commonly after treatment of the lower anterior teeth.4 Many orthodontists have worked towards achieving complete stability and long-term retention after treatment.5 Some studies have recommended the lingual bonded fixed retainer as the most effective and esthetic method for maintaining the dental arch after orthodontic treatment.6,7
The lingual bonded fixed retainer has been applied for a long time in orthodontics. Therefore, several studies have been performed to identify methods to increase bonding strength. Bearn et al.8 studied the effect of type of wire and type of composite and composite blocks. A few in vitro studies have compared the bonding strengths of lingual retainers with different combinations of wires and resins.9,10 Cooke and Sherriff9 performed an in vitro evaluation of the vertical force necessary for debonding lingual retainers constructed of different kinds of wires. Moreover, Baysal et al.10 evaluated the detachment force, amount of deformation, fracture mode, and pull-out force of 3 different wires used in the fabrication of bonded lingual retainers.
Many studies regarding fixed lingual retainers were focused on the effect of wires and resin types. Little is known regarding the effect of the surface area of resin on detachment force. Therefore, the aims of this study were to evaluate the relationship between the detachment force and bonding resin surface area and to determine the adequate amount of resin bonding surface area for lingual bonded fixed retainers.
One hundred and sixty human premolars that were extracted during orthodontic treatment were used in this study. The premolars were stored in saline at room temperature. The extracted teeth were randomly divided into 4 groups, comprising 40 premolars each. For this study, the teeth were first washed with distilled water. To mimic the human dentition, 2 teeth were matched with each other to form a contact area (Figure 1A). Next, autopolymerizing resin was placed in plastic molds, and the lingual half of the root and crown was embedded in the resin. The remaining buccal side of the root was covered with the same resin. The resin blocks of the specimens were randomly divided into 4 groups, with 40 teeth in each group. The diameter of the resin blocks in each group was as follows: group 1, 1.5 mm; group 2, 2.5 mm; group 3, 3.5 mm; and group 4, 4.5 mm.
In this study, Respond Dead Soft straight (length 0.0175 inch; Ormco, Glendora, CA, USA) was used to fabricate the retainers, and Transbond™ XT (3M Unitek, Monrovia, CA, USA) was used to fix the retainers to the tooth surfaces. The buccal surfaces of the teeth were polished with fluoride-free pumice. The method used to determine the bonding resin surface area was similar to that described in the study by Kang et al.11 Briefly, they used round stickers and nail polish to obtain the bonding resin area. The stickers were attached to the buccal surfaces of each specimen, and the distance between the midpoints of the stickers was standardized at 8 mm (Figure 1B, 1C). Then, the prepared crown surface was entirely covered with nail polish (Figure 2A), which was left to air dry for 30 min; next, the stickers were removed, and a circular restricted area of enamel surface was obtained to bond the resin (Figure 2B). Prior to bonding of the fixed retainer to the tooth surfaces, the prepared enamel surfaces were etched for 30 s with 37% ortho-phosphoric acid (Transbond™ XT etching gel system; 3M Unitek), rinsed with water for 20 s using a three-in-one syringe, and dried for 20 s using an oil-free air source. Then, the etched enamel surfaces were primed with Transbond™ XT primer (3M Unitek). The test wire was cut and placed on the primed tooth surface. The wire was placed parallel to the occlusal plane of the teeth (Figure 2C). The composite was applied and cured for 10 s with a light emitting curing unit (Dr's Light; Good Doctor Co., Ltd., Incheon, Korea). The device was set to Turbo mode, in which the intensity of the light was approximately 1,600 mW/cm2. The applied resin was dome-shaped, simulating the exact shape of lingual fixed retainers bonded to teeth of patients. The height of the dome-shaped resin was standardized as 1.3 mm for all specimens. The resin was applied by a single investigator. An electronic caliper was used to measure the height of the dome-shaped resin. To evaluate any measurement errors, the resin height of 80 randomly selected samples was measured at 2-week intervals by a single examiner.
All specimens were stored in water at room temperature for 24 h, and then the detachment force was evaluated. The samples were secured to a jig attached to the universal testing machine (Instron, Canton, MA, USA) (Figure 3). A chisel-edge plunger was mounted on the movable crosshead of the Instron machine. To simulate a vertical force at the midpoint of the wire, the chisel-edge plunger was aimed at the center of the wire and placed parallel to the tooth surface. The crosshead speed was set to 1.0 mm/min, and the maximum load necessary to detach the wire for the first time was recorded in Newtons (Figure 4).
The fracture mode of the specimens was evaluated using the adhesive remnant index (ARI), as suggested by Artun and Bergland.12 The detached enamel surfaces were examined using an optical stereomicroscope SZ61 (Olympus, Tokyo, Japan) at ×20 magnification by a blinded investigator (Lee IH). The ARI system was used to grade the mode of fracture between 0 and 3, based on the amount of adhesive retained on the tooth surface: 0, no adhesive remaining on the tooth surface; 1, less than 50% of the adhesive remaining on the tooth surface; 2, more than 50% of the adhesive remaining on the surface; 3, all the adhesive remaining on the tooth surface.
Statistical analysis was performed using SPSS 12.0 (SPSS Inc., Chicago, IL, USA). The Kolmogorov-Smirnov normality test and Levene's homogeneity test were used to evaluate the data. The debonding force data was not normally distributed, and the groups did not have homogenous variances. Therefore, the Kruskal-Wallis test was used to evaluate statistical differences between the groups. The Mann-Whitney U test was used to examine the differences between individual groups. Statistical significance was evaluated at p = 0.05. The chi-square test was used to analyze fracture modes.
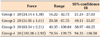
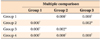
The mean values and standard deviations of detachment forces are presented in Table 1. The Kruskal-Wallis test revealed statistically significant differences in bond strength among the 4 groups. In addition, pairwise comparison of the groups by the Mann-Whitney U test showed statistically significant differences (Table 2). The detachment force was positively correlated to the resin bonding surface area (Figure 5). The mean value of detachment force was the highest for group 4 (102.38 ± 2.92 N), followed by group 3 (63.54 ± 2.21 N), group 2 (51.95 ± 1.61 N), and group 1 (24.14 ± 1.38 N). The ARI scores for all 4 groups are presented in Table 3. The chi-square test revealed statistically significant differences in fracture modes among the 4 groups (χ2 = 77.798, p < 0.001; Table 3).
Bonded retainers have been commonly used to prevent relapse after orthodontic treatment of the lower anterior teeth.13 Patients with fixed retention consistently show better alignment for 5 to 10 years after orthodontic treatment when compared to patients without fixed retention. Furthermore, fixed retainers have no harmful effects on either the teeth or the periodontal tissues.
Various composite and wire combinations have been used for the fabrication of bonded lingual retainers. In this study, Respond Dead Soft straight (length, 0.0175 inch) and Transbond™ XT were used. Furthermore, the buccal surfaces of premolars were selected instead of the lingual surfaces, because of the anatomic variations in crown morphology of the lingual surfaces.
Kwon et al.14 used bovine teeth to compare the shear bonding strength of lingual retainers fabricated using 3 different kinds of resins. Extracted bovine teeth were polished with 600-grit silicon carbide paper to expose a fresh and flat enamel surface. In this study, human premolars, which had various buccal surface contours, were used. It is recommended that the buccal surfaces be polished to obtain a flat enamel surface. However, it was not possible to flatten the enamel surfaces of the specimens in this study because the enamel thickness of human teeth is thinner than that of bovine teeth.
The lingual fixed retainer is usually bonded to 6 anterior teeth or more; however, it was difficult to simulate the exact clinical conditions during this experiment. In this study, the interdental distance between the midpoints of the resin was set as 8 mm, which is impractical in the case of the lower incisors because lower incisors are smaller than premolars. However, to prevent relapse, many orthodontists apply fixed lingual retainers not only on the lower anteriors, but also on the upper anteriors. Moreover, in premolar extraction cases, the fixed lingual retainer is often extended to the premolars in order to maintain tight contacts after the extraction spaces are closed. In other studies, a cantilever type has been used, in which only one end of the wire was embedded into the composite resin, with a force being applied at the free end of the wire.15,16 This procedure simulates teeth where one end of the wire is bonded, usually to the canines or the premolars. Therefore, in order to simulate the clinical conditions to as much as possible, each specimen in this experiment was composed of a pair of teeth, and a vertical force was applied to the interdental wire space.
In an in vitro study by Bearn et al.,8 the wire was embedded into 3-mm wide cylinderic resin blocks with different thickness, and the detachment force was evaluated according to the thickness of the resin. When the overlying resin on the wire was 0.05-mm thick, the result was 24.4 N; 0.55 mm, 71.8 N; 1.05 mm, 151.2 N. They concluded that resin composite 1-mm in thickness provided the optimal combination of maximal strength and minimal bulk. Thus, we attempted to make the composite 1-mm thick; however, the wire thickness did not comply with this suggested optimum thickness. The method error did not exceed 0.1 mm.17 Moreover, no significant mean differences were found between the 2 series of records.
The detachment force for group 3 (diameter, 3.5 mm) was 63.54 N. Irrespective of the similar diameters and thicknesses of the resin, our results differed from those of Bearn et al.8 Several factors such as direction of force, the shape of the bonded resin, and the usage of human teeth seem to be contributing factors for these differences.
Vertical force was applied and measured at the midpoint of the interdental wire, which was bonded to a pair of teeth embedded in a resin block.18 Figure 4 shows that force increases after the first detachment. According to Baysal et al.,10 Respond Dead Soft wires tended to slip through the composite resulting in "V"-shaped deformations (Figure 6). This phenomenon was also observed in this study, implying that bonding failure occurred only partially during the first detachment. Then, the force increased again after first detachment.
The ARI values were significantly different between the 4 groups, indicating that the site of bonding failure differed between the groups. In group 1, most of the bonding failures occurred between the resin and the tooth surface, whereas in groups 2 and 3, the bonding failures took place in a similar manner. As the surface area of bonded resin increased, the amount of residual adhesive also increased. On increasing the applied force, bonding failure first occurred between the resin and the tooth surface. As the resin diameter increased, bonding failures tended to occur between the wire and resin rather than between the resin and tooth surface.
The unit frequently used to measure the shear bonding strength of brackets is Pascals.19,20 In this study, however, Newtons were selected to measure the shear bonding strength. Cooke and Sherriff9 reported that tensile, shear, and torsion forces may occur simultaneously when vertical force is applied to a bonded wire. Therefore, Newtons (unit of force) were considered the appropriate unit to express detachment force as opposed to Pascals (unit of pressure), because the unit Pascal implies that the applied force is evenly distributed throughout the bonding surface area.9
The force required to detach the wire from the bonding resin increased as the diameter of resin increased. The mean values of detachment force were as follows: group 1, 24.14 N; group 2, 51.95 N; group 3, 63.54 N; and group 4, 102.38 N. These results indicate that a wide resin bonding surface area enhances the detachment force of lingual fixed retainers. Despite various studies on the bonding strength of fixed retainers, the exact magnitude of bonding strength sufficient for lingual fixed retainers remains unknown. Tavas and Watts21 suggested that a bracket debonding force of 58 N was suitable for clinical use. Taking this finding into consideration, a resin bonding surface area with a diameter of 3.5 mm (group 3, 63.54 ± 2.21 N) is suggested to render adequate bonding strength.
Only vertical force was applied and measured in this study. Radlanski and Zain16 also compared shear bonding strength and tensile bonding strength. The result of this study showed that for bonding failure, the shear force at the bond site (64.3 N) should be greater than the tensile force (10 N). Bearn et al.8 also reported that the mean tensile force for detaching a wire from different types of composite resins ranged from 11.2 N to 24.4 N. However, these results are still smaller than those found in this study, which means that the lingual fixed retainer is more resistant to vertical forces than to tensile forces.
The bonding surface area is not the only parameter that affects the bond strength of lingual retainers. Bearn et al.8 suggested that the surface characteristics of the wire might have an effect on the retention of the wire to the bonding resin. They also reported that a wire with a larger diameter would have greater bonding surface area and require significantly greater force for removal of the fixed retainer. Thus, the increased bonding surface area between the bonding resin and wire may have affected the bond strength.
Although increasing the amount of resin may help to enhance the bond strength, there are several side effects, such as the tongue discomfort caused by bulky resin and increased vulnerability to periodontal diseases due to calculus and plaque deposition. The wires for retainers should be flexible enough to allow some degree of physiologic movement of the retained teeth. This will help to maintain periodontal health and reduce the concentration of stress on the bonding resin. However, increasing the amount of resin induces a decrease in the wire distance between adjacent teeth. Furthermore, physiologic movement of the retained teeth will be limited due to reduced flexibility of the wire.
Since this was an in vitro study, care should be taken when applying the results of this study to clinical practice. The intraoral environment is affected by multiple factors, including masticatory force, saliva, diet, and oral habits. Strong forces may be intermittently exerted upon occlusal contacts during mastication.8 This study was performed under ideal, or at least, well-controlled, circumstances, i.e., the enamel surfaces were clean before bonding, and no saliva, calculus, or plaque contamination occurred during the bonding procedure. Therefore, it would be inappropriate to expect the same results in vivo. Notably, Murray and Hobson22 measured shear bonding strength of brackets in vivo and in vitro in the 4th, 8th, and 12th weeks. During the first 4 weeks, the average strength was significantly different between in vitro (14.34 MPa) and in vivo (9.78 MPa) conditions. This indicates that etiologic factors are responsible for the failure of fixed retainers in vivo. Therefore, an experimental design that simulates intraoral conditions is necessary to test the bonding strength of bonded fixed retainers. Bearn23 and Zachrisson6 concluded that composite abrasion and detachment between the wire and composite were mainly responsible for the failure of lingual fixed retainers. Moreover, according to a study conducted by Artun and Urbye,24 50% of patients who received orthodontic realignment experienced failure of lingual fixed retainers. According to their study, failure mostly occurred between the wire and resin, and in only one case, wire fracture occurred due to fatigue.
This study showed that the bonding strength of lingual fixed retainers was significantly affected as the resin bonding surface area increased. Considering the minimum bonding strength of brackets, the minimum diameter of 3.5 mm of a bonding resin surface is expected to provide adequate bonding strength.
Figures and Tables
Figure 1
The experimental sample. A, One pair of teeth embedded in a resin block. B, A sticker attached to the buccal surfaces of the sample teeth. C, The distance between the midpoints of 2 stickers (8 mm).

Figure 2
The preparation of the resin bonding surface. A, The surfaces of the teeth were covered by stickers and surrounded by nail polish. B, The resin bonding surface after removal of the sticker. C, A wire is attached to the tooth surfaces with bonding resin.

Figure 3
The universal testing machine. The chisel-edge plunger was aimed at the center of the wire and was parallel to the long axis of the teeth.

Figure 4
The relationship between the force applied to the wire and displacement of the wire. The detachment force was measured when the force perimeter dropped rapidly.

Figure 5
Means and standard deviations of the detachment forces for each group. Group 1, resin surface diameter = 1.5 mm; Group 2, 2.5 mm; Group 3, 3.5 mm; Group 4, 4.5 mm.

References
1. Little RM, Riedel RA, Artun J. An evaluation of changes in mandibular anterior alignment from 10 to 20 years postretention. Am J Orthod Dentofacial Orthop. 1988; 93:423–428.

2. Little RM, Riedel RA, Engst ED. Serial extraction of first premolars-postretention evaluation of stability and relapse. Angle Orthod. 1990; 60:255–262.
3. Little RM, Wallen TR, Riedel RA. Stability and relapse of mandibular anterior alignment-first premolar extraction cases treated by traditional edgewise orthodontics. Am J Orthod. 1981; 80:349–365.

4. Littlewood SJ, Millett DT, Doubleday B, Bearn DR, Worthington HV. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst Rev. 2006; (1):CD002283.

5. Nanda RS, Nanda SK. Considerations of dentofacial growth in long-term retention and stability: is active retention needed? Am J Orthod Dentofacial Orthop. 1992; 101:297–302.

6. Zachrisson BU. Clinical experience with direct-bonded orthodontic retainers. Am J Orthod. 1977; 71:440–448.

7. Zachrisson BU. Adults retention, a new approach in orthdontics. In : Graber LW, Graber TM, editors. Orthodontics, state of the art, essence of the science. St. Louis: Mosby;1986.
8. Bearn DR, McCabe JF, Gordon PH, Aird JC. Bonded orthodontic retainers: the wire-composite interface. Am J Orthod Dentofacial Orthop. 1997; 111:67–74.

9. Cooke ME, Sherriff M. Debonding force and deformation of two multi-stranded lingual retainer wires bonded to incisor enamel: an in vitro study. Eur J Orthod. 2010; 32:741–746.

10. Baysal A, Uysal T, Gul N, Alan MB, Ramoglu SI. Comparison of three different orthodontic wires for bonded lingual retainer fabrication. Korean J Orthod. 2012; 42:39–46.

11. Kang DK, Son WS, Kim HI. Bond strength of bonded lingual retainer with flowable composite resin. J Korea Res Soc Dent Mater. 2004; 31:283–290.
12. Artun J, Bergland S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am J Orthod. 1984; 85:333–340.

13. Al Yami EA, Kuijpers-Jagtman AM, van't Hof MA. Stability of orthodontic treatment outcome: follow-up until 10 years postretention. Am J Orthod Dentofacial Orthop. 1999; 115:300–304.

14. Kwon TY, Meina H, Antoszewska J, Park HS. Direct and indirect bonding of wire retainers to bovine enamel using three resin systems: shear bond strength comparisons. Korean J Orthod. 2011; 41:447–453.

15. Oesterle LJ, Shellhart WC, Henderson S. Enhancing wire-composite bond strength of bonded retainers with wire surface treatment. Am J Orthod Dentofacial Orthop. 2001; 119:625–631.

16. Radlanski RJ, Zain ND. Stability of the bonded lingual wire retainer-a study of the initial bond strength. J Orofac Orthop. 2004; 65:321–335.

17. Dahlberg G. Statistical methods for medical and biological students. London: George Allen & Unwin;1940.
18. Lee HC, Son WS. A study of shear bond strength of bonded retainer according to the bonding method and type of wires. Korean J Orthod. 2002; 32:143–153.
19. Scougall Vilchis RJ, Yamamoto S, Kitai N, Yamamoto K. Shear bond strength of orthodontic brackets bonded with different self-etching adhesives. Am J Orthod Dentofacial Orthop. 2009; 136:425–430.

20. Hajrassie MK, Khier SE. In-vivo and in-vitro comparison of bond strengths of orthodontic brackets bonded to enamel and debonded at various times. Am J Orthod Dentofacial Orthop. 2007; 131:384–390.

21. Tavas MA, Watts DC. A visible light-activated direct bonding material: an in vitro comparative study. Br J Orthod. 1984; 11:33–37.

22. Murray SD, Hobson RS. Comparison of in vivo and in vitro shear bond strength. Am J Orthod Dentofacial Orthop. 2003; 123:2–9.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download