Dear Editor,
Gerstmann's syndrome (GS) involves the combination of agraphia, acalculia, right-left disorientation, and finger agnosia, and is associated with lesions in the left angular and supramarginal gyri. First observed by Gerstmann,1 this entity has been a subject of debate among neurologists, both due to its frequent incomplete presentations and associated aphasia or apraxic features.2 Here we describe a patient with the complete tetrad of GS that resulted from a right parietal lesion.
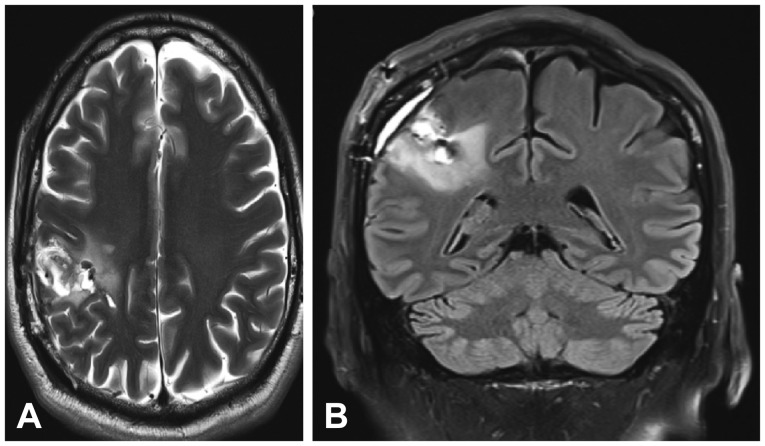
A 57-year-old man was admitted for transient left-arm paresthesia. Brain CT showed intraparenchymal hemorrhage in the frontal centrum semiovale associated with a Spetzler-Martin grade 3 arteriovenous malformation (AVM). Embolization of two aneurysms communicating with the malformation and craniotomy with AVM resection were performed. Brain MRI showed the complete resection of the AVM and postoperative hematic stigmata in the right parietal region (Fig. 1).
The patient was later transferred to our neurorehabilitation division. We observed faciobrachial paresia, as well as complete GS; that is, minor central (surface) agraphia associated with syntaxic errors in number writing, moderate acalculia (for subtractions), a severe right-left disorientation, and mild finger agnosia involving both hands (with left-side predominance: 15/25 correct answers on the left side vs. 20/25 on the right). No significant limb ideomotor apraxia, signs of aphasia, visual field defect, sensory changes, or neglect were observed. However, mild central alexia was noted as well as executive dysfunction for abstract planning tasks in this perfectly ambidextrous patient (Edinburgh Handedness Inventory score=0). The patient was discharged after intensive physiotherapy and occupational therapy. The paresis had improved substantially 3 months later, whereas moderate right-left disorientation was present, and mild finger agnosia persisted. The patient was able to perform basic and instrumental activities of daily living and resume his activity as a consultant for United Nations socioeducation projects.
This patient presented the complete tetrad of GS that resulted from a right parietal lesion. The complete tetrad of GS has rarely been reported, and such cases have been associated with either the left cortical angular gyrus3 or subcortical lesions.4 On the other hand, this syndrome is frequently associated with apraxia or aphasia.25 Josef Gerstmann reported that the common denominators (“Grundstörung”) of finger agnosia, right-left confusion, agraphia, and acalculia represented a disorder of the body schema restricted to the hand and fingers, but several authors have proposed a defect in mental spatial rotations to explain the co-occurrence of these four symptoms.346 In addition, Wingard et al.7 stated that these clinical impairments do not share a common neuronal network and that dominant parietal lesions usually associated with GS could be explained by the anatomical closeness of different neuronal networks implicated in these clinical symptoms. Furthermore, Rusconi et al.58 pointed out that a single cortical lesion could not account for impairment of functioning involving such diverse neuropsychological domains as calculation, writing, finger gnosia, and right-left orientation. Their conjecture was based on 1) the different neuronal networks implicated, 2) electrical stimulation in open brain surgery never eliciting the complete tetrad of GS, and 3) pure GS presentations regularly being caused by subcortical lesions.4 Moreover, functional imaging in healthy subjects did not show parietal cortical overlap during paradigms that activate the four functions of calculation, writing, right-left distinction, and finger gnosia. However, fiber tracking in diffusion-tensor imaging highlighted a common subcortical region (adjacent to the intraparietal sulcus) whose white-matter fibers are connected to all four cortical regions implicated in the GS tetrad.
Here we have described a case presenting with the complete tetrad of GS (with additional central alexia) associated with a right cortico-subcortical parietal hemorrhage in a converted left-handed subject. The lesion shown in Fig. 1 is located opposite the intraparietal sulcus. This illustrates the functional MRI findings obtained by Rusconi et al.8 in an actual patient and provides additional arguments in favor of a disconnection syndrome to explain the tetrad first described by Josef Gerstmann.
References
1. Gerstmann J. Fingeragnosie: eine umschriebene Störung der Orientierung am eigenen Körper. Wien Klin Wochenschr. 1924; 37:1010–1012.
2. Benton AL. Gerstmann's syndrome. Arch Neurol. 1992; 49:445–447. PMID: 1580804.
3. Carota A, Di Pietro M, Ptak R, Poglia D, Schnider A. Defective spatial imagery with pure Gerstmann's syndrome. Eur Neurol. 2004; 52:1–6. PMID: 15218337.

4. Mayer E, Martory MD, Pegna AJ, Landis T, Delavelle J, Annoni JM. A pure case of Gerstmann syndrome with a subangular lesion. Brain. 1999; 122(Pt 6):1107–1120. PMID: 10356063.

5. Rusconi E, Pinel P, Dehaene S, Kleinschmidt A. The enigma of Gerstmann's syndrome revisited: a telling tale of the vicissitudes of neuropsychology. Brain. 2010; 133(Pt 2):320–332. PMID: 19903731.

6. Ardila A. A proposed reinterpretation of Gerstmann's syndrome. Arch Clin Neuropsychol. 2014; 29:828–833. PMID: 25377466.

7. Wingard EM, Barrett AM, Crucian GP, Doty L, Heilman KM. The Gerstmann syndrome in Alzheimer's disease. J Neurol Neurosurg Psychiatry. 2002; 72:403–405. PMID: 11861708.

8. Rusconi E, Pinel P, Eger E, LeBihan D, Thirion B, Dehaene S, et al. A disconnection account of Gerstmann syndrome: functional neuroanatomy evidence. Ann Neurol. 2009; 66:654–662. PMID: 19938150.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download