Dear Editor,
We report a case study of mitochondrial encephalopathy, lactic acidosis, and stroke-like episode (MELAS) syndrome with presentation of headache and prolonged visual aura.
Mitochondrial encephalopathy, lactic acidosis, and stroke-like episode syndrome is one of the most commonly recognized mitochondrial diseases. It is characterized by lactic acidosis, the occurrence of stroke-like episodes, and other secondary manifestations such as migraine-like headache, seizure, cognitive impairment, cardiac conduction defects, and short stature.1,2 These syndromic phenomena are most commonly caused by an m.3243A>G (adenine to guanine) mutation at position 3243 of the mitochondrial genome. The seizures are often associated with migraine-like headache and occur primarily in a group of patients who develop stroke-like episodes. Since stroke-like episodes have a predilection for the parieto-occipital and posterior temporal areas, the seizure semiology frequently demonstrates disturbance in these locations.1,3
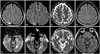
We describe a MELAS syndrome patient who presented with recurrent headache and visual aura lasting for more than several days. The patient was a 23-year-old female who was referred to our outpatient clinic due to headache with visual aura lasting for 1 week. Her past medical history and family history were unremarkable, and with the exception of small stature (height, 147 cm; weight, 38 kg), a physical examination yielded normal results. During a neurological examination the patient was alert but complained of a continuous glittering light as well as visual loss in the left visual field. No abnormalities were found on motor, sensory, cerebellar, and reflex function testing. The results of laboratory studies, including blood lactic acid and CSF analyses, were normal. The diffusion-weighted imaging (DWI) and fluid-attenuated inversion recovery (FLAIR) MRI scans performed on the second day of hospitalization revealed a high signal intensity in the right parietal lobe (Fig. 1A, B, and C); the EEG exhibited rhythmic activities in the corresponding area.
Under the presumptive diagnosis of partial status epilepticus, she was treated with levetiracetam (1,000 mg/day) after receiving an injection of intravenous lorazepam. The visual aura subsided completely after 3 days, and the follow-up MRI performed on day 7 of hospitalization revealed disappearance of the previously observed abnormality (Fig. 1D). The patient was maintained on low-dose levetiracetam (500 mg/day) for 2 years. Three years later the patient visited our outpatient clinic again for recurrence of visual aura lasting for 3 days, contralateral to the previous side. DWI and FLAIR MRI scans revealed a high signal intensity in the left occipital lobe (Fig. 1E, F, and G); a follow-up EEG showed rhythmic activities in the corresponding area. A genetic study revealed the presence of a mitochondrial mutation (m.3243A>G), indicating the presence of MELAS syndrome.
Neurological problems are the most frequent clinical features of mitochondrial disorder, and recurrent strokes or transient-ischemic-attack-like episodes are the most common manifestations of MELAS syndrome. Stroke-like lesions usually appear as multifocal infarct-like areas with cortical involvement that has no matching vascular territory.4 The MRI abnormalities in MELAS syndrome often disappear on follow-up MRI, as in our case, as a result of the reversible pathogenesis due to mitochondrial cytopathy or angiopathy.4,5 However, other common and clinically nonserious symptoms of MELAS syndrome, including migraine-like headache, seizure, short stature, and even psychological problems such as depression and anxiety, can go unrecognized for up to 20 years before the onset of overt neurological impairment.6
The findings of the present study show that patients with MELAS syndrome can present with common neurological diseases, such as migraine with aura or occipital lobe epilepsy.1,2,3 Our experience suggests that clinical suspicion is important for an early diagnosis of this particular metabolic disease.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download