Abstract
Background
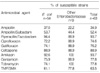
A high prevalence of fluoroquinolone resistance among uropathogens has been observed in Korea. Since empirical antimicrobial therapy should be guided by the proportion of pathogens resistant to the chosen antibiotic, the limitation of fluoroquinolones as the first empirical choice for acute cystitis is noticed in the clinical setting. The present study was undertaken to determine the susceptibility profiles of urinary isolates to cefcapene pivoxil and assess the clinical efficacy in patients with acute uncomplicated cystitis.
Materials and Methods
The study was a prospective, open label, non-comparative, non-blinded trial. Ninety-two patients with acute, uncomplicated symptomatic cystitis from two hospitals were treated with cefcapene pivoxil 100 mg tid for 5 days and followed up for 2 weeks.
Results
Seventy-seven of the 92 patients were evaluated. Bacteriological eradication of initial pathogens was achieved in 97.4% by 2 weeks after therapy termination. Seventy-four of 77 (96.1%) patients were symptomatically cured or improved after completion of therapy. Drug related adverse experiences were seen in 8 patients. None necessitated cessation of therapy. No significant biochemical or hematological abnormalities occurred.
References
1. Sobel JD. Bacterial etiologic agents in the pathogenesis of urinary tract infection. Med Clin North Am. 1991. 75:253–273.

2. Gupta K, Hooton TM, Stamm WE. Increasing antimicrobial resistance and the management of uncomplicated community-acquired urinary tract infections. Ann Intern Med. 2001. 135:41–50.

3. Warren JW, Abrutyn E, Hebel JR, Johnson JR, Schaeffer AJ, Stamm WE. Guidelines for antimicrobial treatment of uncomplicated acute bacterial cystitis and acute pyelonephritis in women. Infectious Diseases Society of America (IDSA). Clin Infect Dis. 1999. 29:745–758.

4. Kim SW, Lee JY, Park WJ, Cho YH, Yoon MS. Antibiotic Sensitivity to the Causative Organism of Acute Simple Urinary Tract Infection. Korean J Urol. 2000. 41:1117–1124.
5. Lee SJ, Cho YH, Kim BW, Lee JG, Jung SI, Lee SD, Lee SE, Kim ME, Choi YD, Rim JS, Sim BS, Cho IR, Ryu SB, Kim CS, Kim WJ, Lee TY. A Multicenter Study of Antimicrobial Susceptibility of Uropathogens Causing Acute Uncomplicated Cystitis in Woman. Korean J Urol. 2003. 44:697–701.
6. Kim ME, Ha US, Cho YH. Prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in female outpatients in South Korea: a multicentre study in 2006. Int J Antimicrob Agents. 2008. S1:15–18.

7. Saito A, Hiraga Y, Watanabe A, Saito A, Shimada K, Kobayashi H, Odagiri S, Miki F, Soejima R, Oizumi K, Hara K, Nakashima M. The Japanese Cefcapene Study Group. Comparative clinical study of cefcapene pivoxil and cefteram pivoxil in chronic respiratory tract infections by a double-blind method. J Int Med Res. 2004. 32:590–607.

8. National Committee for Clinical Laboratory Standards. NCCLS document M100-S13. Performance standards for antimicrobial susceptibility testing. 2003. Wayne, PA: NCCLS.
9. Nicolle LE. Epidemiology of urinary tract infection. Infect Med. 2001. 18:153–162.
11. Karlowsky JA, Kelly LJ, Thornsberry C, Jones ME, Sahm DF. Trends in antimicrobial resistance among urinary tract infection isolates of Escherichia coli from female outpatients in the United States. Antimicrob Agents Chemother. 2002. 46:2540–2545.

12. Song HJ, KIM SJ. A Study of Antimicrobial Sensitivity to the Causative Organism of Urinary Tract Infection. Korean J Urol. 2005. 46:68–73.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download