Abstract
Purpose
Behçet's disease (BD) is a chronic inflammatory disease characterized by orogenital ulcers, skin and ocular lesions, in addition to articular, vascular, and neurologic symptoms. Carpal tunnel syndrome (CTS), can also occur in BD patients secondary to inflammation in the connective tissues, vessels, and tendons, as well as nerve involvement in BD itself. However, reports of patients who have CTS in BD are rare. The aim of this study was to evaluate the clinical characteristics of CTS in BD patients.
Materials and Methods
Retrospective analysis of the medical records of 1750 BD patients, and 14 (0.8%) BD patients who were diagnosed with CTS was performed at the BD Specialty Clinic of Severance Hospital. Patient demographics, disease activity/severity for both diseases, and the clinical characteristics of CTS in BD were recorded and analyzed.
Results
All 14 BD patients with CTS were women. Twelve patients (85.7%) were diagnosed with active BD. The CTS was mild in 8 patients (57.2%), moderate in 3 patients (21.4%), and severe in 3 patients (21.4%). Ten patients (71.4%) had BD prior to the diagnosis of CTS, and these 10 patients all had active BD.
Conclusion
CTS can occur as a result of the inflammation associated with BD and can also be the presenting symptom of nerve involvement in BD. CTS can also develop as the initial symptom of BD. Therefore, a higher degree of suspicion should be maintained for CTS in patients with BD and vice versa; however, the exact relationship is uncertain.
Behçet's disease (BD), a chronic systemic inflammatory disease, is characterized by recurrent oral and genital ulcers, cutaneous lesions, and recurrent uveitis. These major findings can occasionally be accompanied by other manifestations, including gastrointestinal, articular, vascular, and neurologic involvement.1 Neurologic involvement has been reported to occur in 2.2% to 49% of BD patients234 and is one of the major causes of morbidity in BD.5 Although central nervous system involvement is not infrequent in BD, and symptoms such as headache and cognitive and behavioral changes can occur in BD patients, involvement of the peripheral nervous system is relatively rare.34678 Only a few cases of peripheral neuropathy and myopathy in BD patients have been reported in the literature.39 However, according to recent studies, peripheral neuropathy is not as uncommon among BD patients as previously thought.3101112 Articular manifestations are also relatively common, including subacute to chronic synovitis.13
Carpal tunnel syndrome (CTS) is a representative mononeuropathy caused by entrapment of the median nerve in the carpal tunnel that affects approximately 0.9% to 1.2% of the general population.14 CTS can result from any cause that induces compression or irritation of the median nerve, including synovitis, thickening of the tendon or flexor retinaculum, fluid accumulation, or subsynovial connective tissue alterations.15 Patients with CTS typically present with pain and paresthesia/numbness (intermittent or constant) of the hand along the median nerve distribution. Atrophy and wasting of the thenar muscle can also occur in the advanced stages.15
By definition, BD is associated with chronic, widespread inflammation and can be accompanied by peripheral nerve involvement; therefore, it is not surprising that CTS can occasionally develop in BD patients. In this study, 14 BD patients who were also diagnosed with CTS were studied. As far as we know, there has been no detailed report discussing CTS in BD patients. The purpose of this study is to analyze the clinical presentation, characteristics, treatment, and prognosis of CTS in BD.
A retrospective review of the medical records of 1750 BD patients in search of people who were diagnosed with CTS between 2005 and 2012 at the BD Specialty Clinic of Severance Hospital was performed. The final study included 14 BD patients diagnosed according to the criteria of the International Study Group for BD and the revised criteria of the BD Research Committee of Japan.1617 CTS was diagnosed based on the patients' clinical presentation, physical examination (including Tinel's sign and Phalen's test), and nerve conduction studies (NCS) performed by a neurologist or an orthopedic surgeon.
The disease activity of BD was assessed based on the patients' presenting symptoms, using the diagnostic criteria of the International Study Group for BD and the revised criteria of the BD Research Committee of Japan.1617 Patients with ≥2 major criteria with or without any minor criteria were considered to have active disease. The clinical severity of the CTS was assessed by the clinical symptoms and was classified as mild, moderate, and severe according to the degree of paresthesia, numbness/pain, and associated muscle weakness as suggested by the British Society for Surgery of the Hand in 2011.18
In our study, all 14 BD patients who had CTS were women, with a mean age of 54.1±8.3 years (range, 45 to 71 years) (Table 1). The overall frequency of CTS in our cohort was 0.8%. The high percentage of women in our study may also be the result of the female predominance of BD in Korea.19 The average patient age at the time of disease onset showed a slight difference between the 2 diseases, with onset at 31 to 64 years for BD (mean 44.3±8.7 yr), and at 37 to 64 years for CTS (mean 48.1±8.3 yr). Ten patients (71.4%) had BD as the preceding disease, and 4 patients (28.6%) were diagnosed with CTS before being diagnosed with BD.
Twelve patients (85.7%) were diagnosed with active BD, and two patients (14.3%) were in a stable disease state without any need for systemic medication. With respect to CTS, eight patients (57.2%) were diagnosed as mild, three patients were diagnosed (21.4%) as moderate, and three patients (21.4%) were diagnosed as severe. The three patients diagnosed with severe CTS all had atrophy of the thenar muscle, and five patients (35.7%) had bilateral CTS. The clinical features of the 14 patients are shown in Table 2.
CTS was diagnosed with NCS in 12 patients (85.7%). Two patients (14.3%) failed to show any changes on NCS and were diagnosed clinically with CTS. No significant associations were identified between the disease activity of BD and the severity of CTS or between the BD activity and the ability of NCS to detect CTS.
Colchicine was prescribed for 10 patients (71.4%) as the main therapeutic drug for BD. Non-steroidal anti-inflammatory drugs (NSAIDs) were used in three patients (21.4%) for arthralgias or pain control; systemic corticosteroids were used in five patients (35.7%) for uveitis or acute symptom relief. Anticoagulants were administered to one patient (7.1%) for venous thrombosis, and 5-aminosalicylic acid was prescribed for two patients (14.3%) for gastrointestinal symptoms. Topical corticosteroids were available for all patients to help treat mucocutaneous ulcers.
For the treatment of CTS, NSAIDs were used in seven patients (50.0%) for pain control. Antidepressants or anti-epileptic agents, such as benzodiazepines or gabapentin, were prescribed to help reduce neuropathic pain in three patients (21.4%). Three patients who were classified with severe CTS had surgical treatment to release the transverse carpal ligament. Three other patients did not receive any treatment for CTS and were kept under observation only.
Although there have been some reports about peripheral neuropathy in BD,3101112 no studies have focused on CTS in BD. Despite an obvious pathophysiologic relationship between BD and CTS with respect to disease characteristics, studies exploring the relationship between the two entities are lacking. In this study, we retrospectively evaluated the medical records of 14 patients who had both BD and CTS.
BD, which can theoretically involve all sizes of vessels, causes chronic inflammation in various organ systems, resulting in diverse clinical manifestations including mucocutaneous, ocular, gastrointestinal, neurologic, and articular symptoms.2021 Therefore, BD patients can present with various joint symptoms and neurologic symptoms, such as joint pain or swelling, tingling sensations, and numbness. BD patients with such complaints undergo thorough history-taking and physical examinations and are referred to the rheumatology, orthopedic surgery, or neurology departments for further testing. In the present study, CTS was diagnosed based on physical and neurological examinations including Tinel's sign and Phalen's test. NCS and other radiologic studies were performed and confirmed by a specialist.
The overall prevalence of CTS among BD patients was 0.8% in this retrospective study. Previous reports suggest that the prevalence of CTS among the general population is 0.9-1.2%.14 Given the retrospective nature of the present investigation, there is a greater chance of underestimation of CTS among BD patients in our clinic. Further prospective study is required to determine a precise prevalence of CTS in BD and compare it with that of the general population.
All BD patients with CTS in the present study were middle-aged or elderly females. These findings reflect the general epidemiology of CTS, which develops most commonly in patients between 45 and 65 years of age, with a male to female ratio of 1:3.22 In most patients, BD developed before the onset of CTS. The 10 patients who had BD prior to the diagnosis of CTS had an active disease state, suggesting the possibility of active inflammatory processes additionally affecting CTS development. The remaining four patients were diagnosed with CTS before the diagnosis of BD.
In general, bilateral CTS occurs in approximately 55% to 65% of cases.23 In this study, however, bilateral CTS occurred in only 35.7% of patients. This unusually low percentage might again be a result of the small sample size and have included patients before the other hand was affected. Patients presenting with unilateral symptoms are at increased risk for the development of CTS on the other side and should be followed closely. In the present study, the dominant hand was affected in eight (88.9%) of nine patients who had unilateral CTS. All five patients with bilateral CTS had the dominant hand affected first.
According to our findings, there were no significant associations between the disease activity of BD and the clinical severity of CTS or NCS findings of CTS. These results are similar to previous reports which also showed a lack of correlation between the clinical findings of BD and electrophysiologic data.41224 Although inflammation created by vasculitis-induced tissue damage and secretion of pro-inflammatory cytokines are involved in the development of neurologic symptoms in BD, non-vascular, nerve-targeted pathologic reactions that may not always correlate with disease activity can also occur in BD.1220 The lack of association between BD activity and NCS findings may be due to subclinical neurologic abnormalities or clinical alteration of the disease status.4 The two patients who had normal findings in NCS studies had a relatively short duration of CTS (3 months and 6 months) compared to patients with detectable peripheral neuropathy. These findings agree with previous studies that mentioned that patients with detectable peripheral neuropathy had a longer duration of disease.41224
However, the relatively low frequency of CTS among BD patients, the lack of association between the disease activities of the two conditions, and the frequent involvement of the side of the dominant hand suggest that CTS might simply be caused by mechanical stress rather than BD-related inflammation. Nevertheless, as most patient with CTS in this case series had associated arthritis or vasculitis, they may have been susceptible to inflammation and mechanical stress and subsequent CTS development. Regarding the lack of published evidence supporting this hypothesis, it is necessary to conduct further studies to determine if BD-associated and CTS development are directly or indirectly related.
Colchicine is used frequently for the treatment of BD. Although it is generally well-tolerated, adverse effects including gastrointestinal disturbance, renal dysfunction, myopathy, and peripheral neuropathy have been reported.252627 Because more than 70% of patients in our study group were on colchicine, the relationship between colchicine and the development of peripheral neuropathy should be considered. However, colchicine-induced neuromuscular toxicity is associated with prominent myopathic features (including painless proximal muscle weakness and elevated creatine phosphokinase levels), mild areflexia, and paresthesias.27 None of our patients experienced any symptoms consistent with colchicine-induced neuropathy.
The treatment of CTS is based on the severity of the disease and the patient's preference. Until recently, there was no established definitive treatment.15 Nonoperative methods include oral corticosteroids, NSAIDs, local steroid injection, and splinting.15 Although surgical treatment is more effective than other non-invasive, conservative treatments,28 only three patients (21.4%) in our study underwent surgery. Treatment options may have been based on the clinical severity of CTS and may also reflect the tendency of BD patients to avoid surgery whenever possible. BD patients have a divergent wound healing process with an intense inflammatory response compared to healthy controls;29 therefore, most patients are anxious about abnormal wound healing and pathergy reactions.
In this study, we report our experience of 14 BD patients also diagnosed with CTS. The chronic inflammatory state associated with BD may play a role in CTS development. As medications commonly used to treat BD (colchicine, cyclosporine A, azathioprine, and thalidomide) can have neurologic side effects,30 the physician must be able to differentiate drug-induced complications from other peripheral neuropathies such as CTS.
Although this study had a small sample size and lacked biopsy results, it is meaningful in that it is the first description of the relationship between CTS and BD. CTS can be the presenting symptom of neurologic involvement in BD, but it is more likely that "inflammation-prone" conditions of BD can result in CTS as an associated musculoskeletal symptom or can promote the effects of mechanical stressors. CTS can even represent the first symptom of BD. Therefore, it is important to maintain a high degree of suspicion for CTS when BD patients present with wrist pain, tingling sensations, or finger numbness.
References
1. James DG. Behcet's syndrome. N Engl J Med. 1979; 301:431–432. PMID: 460347.
2. Siva A, Altintas A, Saip S. Behçet's syndrome and the nervous system. Curr Opin Neurol. 2004; 17:347–357. PMID: 15167071.

3. Atasoy HT, Tunc TO, Unal AE, Emre U, Koca R, Esturk E, et al. Peripheral nervous system involvement in patients with Behçet disease. Neurologist. 2007; 13:225–230. PMID: 17622917.

4. Akbulut L, Gur G, Bodur H, Alli N, Borman P. Peripheral neuropathy in Behçet disease: an electroneurophysiological study. Clin Rheumatol. 2007; 26:1240–1244. PMID: 17149536.

5. Onder M, Gürer MA. The multiple faces of Behçet's disease and its aetiological factors. J Eur Acad Dermatol Venereol. 2001; 15:126–136. PMID: 11495519.
6. Siva A, Kantarci OH, Saip S, Altintas A, Hamuryudan V, Islak C, et al. Behçet's disease: diagnostic and prognostic aspects of neurological involvement. J Neurol. 2001; 248:95–103. PMID: 11284141.

7. Kidd D, Steuer A, Denman AM, Rudge P. Neurological complications in Behçet's syndrome. Brain. 1999; 122(Pt 11):2183–2194. PMID: 10545402.

8. Akman-Demir G, Baykan-Kurt B, Serdaroglu P, Gürvit H, Yurdakul S, Yazici H, et al. Seven-year follow-up of neurologic involvement in Behçet syndrome. Arch Neurol. 1996; 53:691–694. PMID: 8929179.
9. Namer IJ, Karabudak R, Zileli T, Ruacan S, Küçükali T, Kansu E. Peripheral nervous system involvement in Behçet's disease. Case report and review of the literature. Eur Neurol. 1987; 26:235–240. PMID: 3595663.
10. Lannuzel A, Lamaury I, Charpentier D, Caparros-Lefebvre D. Neurological manifestations of Behçet's disease in a Caribbean population: clinical and imaging findings. J Neurol. 2002; 249:410–418. PMID: 11967645.

11. Akbulut L, Gur G, Bodur H, Alli N, Borman P. Peripheral neuropathy in Behçet disease: an electroneurophysiological study. Clin Rheumatol. 2007; 26:1240–1244. PMID: 17149536.

12. Birol A, Ulkatan S, Koçak M, Erkek E. Peripheral neuropathy in Behçet's disease. J Dermatol. 2004; 31:455–459. PMID: 15235183.

13. Kim HA, Choi KW, Song YW. Arthropathy in Behçet's disease. Scand J Rheumatol. 1997; 26:125–129. PMID: 9137328.
14. Walker-Bone K, Palmer KT, Reading I, Coggon D, Cooper C. Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Rheum. 2004; 51:642–651. PMID: 15334439.

15. Uchiyama S, Itsubo T, Nakamura K, Kato H, Yasutomi T, Momose T. Current concepts of carpal tunnel syndrome: pathophysiology, treatment, and evaluation. J Orthop Sci. 2010; 15:1–13. PMID: 20151245.

16. International Study Group for Behçet's Disease. Criteria for diagnosis of Behçet's disease. Lancet. 1990; 335:1078–1080. PMID: 1970380.
17. Kurokawa MS, Yoshikawa H, Suzuki N. Behçet's disease. Semin Respir Crit Care Med. 2004; 25:557–568. PMID: 16088499.
18. The British Society For Surgery of The Hand. Evidence for Surgical Treatment 1 (BEST 1) Carpal Tunnel Syndrome (CTS). England: Lincoln's Inn Fields, London, British Society for Surgery of the Hand;2011. accessed on 2014 July 15. Available at: http://www.bssh.ac.uk/education/guidelines/carpal_tunnel_syndrome.pdf.
19. Cho SB, Cho S, Bang D. New insights in the clinical understanding of Behçet's disease. Yonsei Med J. 2012; 53:35–42. PMID: 22187230.

20. Sakane T, Takeno M, Suzuki N, Inaba G. Behçet's disease. N Engl J Med. 1999; 341:1284–1291. PMID: 10528040.

21. Kalayciyan A, Zouboulis C. An update on Behsçet's disease. J Eur Acad Dermatol Venereol. 2007; 21:1–10. PMID: 17207160.
22. Bongers FJ, Schellevis FG, van den Bosch WJ, van der Zee J. Carpal tunnel syndrome in general practice (1987 and 2001): incidence and the role of occupational and non-occupational factors. Br J Gen Pract. 2007; 57:36–39. PMID: 17244422.
23. Street ER, Eastwood GL, Royle SG. Staged release of bilateral carpal tunnel syndrome: cancellation rates of the second side procedure. J Hand Surg Eur Vol. 2013; 38:552–553. PMID: 23172822.

24. Budak F, Efendi H, Apaydin R, Bilen N, Komsuoglu S. The F response parameters in Behçet's disease. Electromyogr Clin Neurophysiol. 2000; 40:45–48. PMID: 10782357.
25. Pirzada NA, Medell M, Ali II. Colchicine induced neuromyopathy in a patient with normal renal function. J Clin Rheumatol. 2001; 7:374–376. PMID: 17039178.

26. Altiparmak MR, Pamuk ON, Pamuk GE, Hamuryudan V, Ataman R, Serdengecti K. Colchicine neuromyopathy: a report of six cases. Clin Exp Rheumatol. 2002; 20(4 Suppl 26):S13–S16. PMID: 12371628.
28. Verdugo RJ, Salinas RA, Castillo JL, Cea JG. Surgical versus non-surgical treatment for carpal tunnel syndrome. Cochrane Database Syst Rev. 2008; CD001552. PMID: 18843618.
29. Melikoglu M, Uysal S, Krueger JG, Kaplan G, Gogus F, Yazici H, et al. Characterization of the divergent wound-healing responses occurring in the pathergy reaction and normal healthy volunteers. J Immunol. 2006; 177:6415–6421. PMID: 17056573.

30. Yazici H, Yurdakul S, Hamuryudan V. Behçet disease. Curr Opin Rheumatol. 2001; 13:18–22. PMID: 11148711.

Table 1
Demographics of the 14 Women with Behçet's Disease and Carpal Tunnel Syndrome
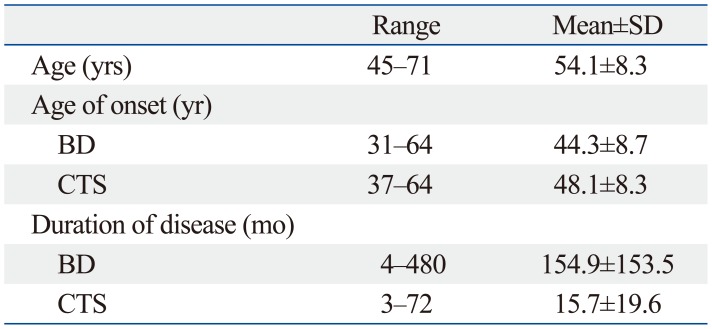
| Range | Mean±SD | |
|---|---|---|
| Age (yrs) | 45-71 | 54.1±8.3 |
| Age of onset (yr) | ||
| BD | 31-64 | 44.3±8.7 |
| CTS | 37-64 | 48.1±8.3 |
| Duration of disease (mo) | ||
| BD | 4-480 | 154.9±153.5 |
| CTS | 3-72 | 15.7±19.6 |
Table 2
Clinical Characteristics of the 14 Patients with BD and CTS
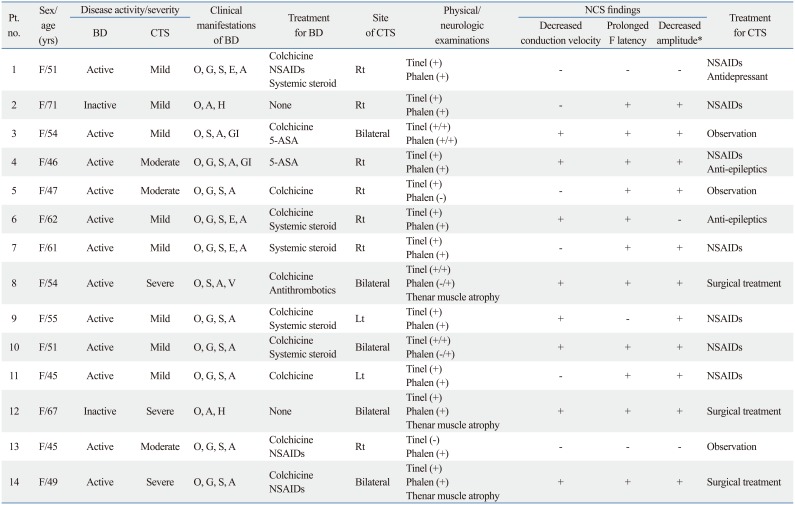
BD, Behçet's disease; CTS, carpal tunnel syndrome; NCS, nerve conduction studies; O, oral ulceration; G, genital ulceration; S, skin lesion; E, eye lesion; A, arthralgia; V, vascular lesion; H, headache; GI, gastrointestinal symptoms; NSAIDs, non-steroidal anti-inflammatory drugs; 5-ASA, acetylsalicylic acid.
*Amplitude of compound muscle action potential and sensory nerve action potential.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download