INTRODUCTION
The axillary brachial plexus block (ABPB) for wrist and hand surgery is a valuable anesthetic method for postoperative pain control, decreased recovery time, and early discharge of ambulatory surgery patients.
1 Currently, ABPB is known to be more effective when performed with ultrasound-guidance, and ultrasound-guided ABPB (US-ABPB) with or without nerve stimulation is widely used as perineural (PN) injection technique.
2,
3 However, this technique has risks of direct nerve injury by the needle due to limitations of US imaging related to inter-individual anatomical variation and operator-dependent skills. It also requires needle repositioning, which can increase the risk of vessel damage and other complications.
Recently, several studies showed that one or two injections around axillary artery, which means perivascular (PV) injection, is a highly successful method to perform an ABPB; it is faster, requires fewer injections, and reduces procedural pain and discomfort.
4,
5,
6 This technique is based on the concept that highly accurate local anesthetics (LA) injection in the axillary sheath, which is possible with US, results in diffusion to the median, ulnar, and radial nerves, making individual nerve blocks unnecessary. In addition, the previous trials showed comparable success rate.
4,
5,
6
The present study compared a PN injection technique with two methods of PV injection. One PV method required a single injection in the 12-o'clock position of the axillary artery while the other involved two injections around the axillary artery, one in the 12-o'clock position and the other at 6-o'clock. Previous studies examined a PV method with a single injection at the 6-o'clock position.
4,
5 Clear ultrasonographic imaging of the anatomy and visualization of the needle make handling easier and it increases safety. The needle insertion angle affects visibility; steeper angles generate poorer images and lower accuracy resulting in tissue injury.
7,
8 In our earlier study, therefore, we compared 6- and 12-o'clock positions and found there were no differences in the aspects of procedure time, onset time, and complications.
9 Nevertheless, handling of needle was easier in 12-o'clock position because of structures around deeper area of axillary 839artery such as multiple veins, and muscles fascia. In the present study, therefore, we again selected the 12-o'clock position which was closer to skin for PV single injection, and compared this position to PV double injection and PN injection techniques to find out which method is more effective and superior in terms of risk of complications.
MATERIALS AND METHODS
This prospective, randomised, and observer-blinded trial was approved by our Institutional Review Board (IRB No. ECT 12-22-04). The 87 patients provided written informed consent, and were enrolled following an explanation of the purpose and methods. Subjects were adults (20-85 yr) with American Society of Anesthesiologists physical status classification of I or II who were scheduled for hand or wrist surgery with ABPB. Exclusion criteria were as follows: pregnancy, infection in the injection area, allergy to LA, coagulopathy, and the inability to communicate.
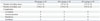
All patients were allocated into groups by a computer-generated randomised sequence with 29 patients in each group. There were no significant differences in the demographic characteristics among the three groups (
Table 1). The proportions of various types of surgical procedures were similar among the three groups (
Table 1).
The blocks were performed by two experienced anesthesiologists who have performed more than 50 US-ABPBs. Standard monitoring was initiated including electrocardiography, non-invasive blood pressure, and pulse oximetry. Patients were in the supine position, and the arm was externally rotated with 90° shoulder abduction and 90° elbow flexion. Oxygen (6 L/minutes) was supplied by mask, and the patient was sedated with intravenous injections of midazolam (1-2 mg) and fentanyl (25-50 µg). The axillary area was disinfected with povidone-iodine solution.
We used the Sonosite M-Turbo® US (Sonosite, Bothell, WA, USA). The 38 mm, 6-13 MHz linear US probe was covered with sterile vinyl, and placed on the axillary fold so that the artery and nerve were visible in the short axis view. It was positioned, so that the 3-o'clock position was medial and the 9-o'clock position was lateral with respect to the axillary artery. In this view, the 12-o'clock position (closest to the skin) faced anteriorly, while the 6-o'clock position was posterior.
9 The orientation of each nerve was recorded. The block was performed with the in-plane technique using a 22-gauge, 50-mm needle (Stimuplex®, B. Braun, Melsungen, Germany) connected to a syringe containing 2% lidocaine with epinephrine (5 µg/mL).
For the PN group, the needle tip was placed in close proximity to individual nerves of axillary brachial plexus; the median, ulnar, and radial nerves. The nerves were identified visually by US, and if they were well defined, LA was injected. In case of any doubts regarding nerve identity, a nerve stimulator (Stimuplex® Dig RC, B. Braun, Melsungen, Germany) was used and delivered an electronic stimulus of 2 Hz and 0.6 mA, and observed whether the movement of the fingers or hand by nerve innervation was induced. After identification of each nerve, 8 mL of LA were injected around the nerve after aspirating for blood. If hypoechoic sign surrounding the nerve (doughnut sign) was not observed on the real-time US image during injection of LA, the needle was repositioned.
For the PV1 group, the needle tip was positioned anteriorly in the 12-o'clock position of the axillary artery. After assuring that the needle was not in the artery, 24 mL of LA were injected. LA injection was observed with the US, and the needle position could be readjusted if necessary.
In the PV2 group, 12 mL of LA were injected in the 12-o'clock position, and the remaining 12 mL were injected posterior to the axillary artery in the 6-o'clock position.
Lastly, the musculocutaneous (MC) nerve in all groups was blocked separately using US. The needlepoint was positioned close to the nerve in the coracobrachialis muscle and LA was administered.
After performing the block, the anesthetic procedure time (the time from insertion to removal of the needle), the number of needle insertions, and the number of axillary arteries and veins were recorded. After completing procedure, a blinded observer measured the degree of sensory and motor blockade, the onset time (the time from removal of the needle to obtaining surgical anesthesia), and the calculated induction time (sum of the anesthetic procedure and onset time).
The degree of sensory and motor blockade was evaluated according to the movement and dermatome of each nerve. It was evaluated at 5 minutes intervals for 15 minutes with the final needle removal being time 0. The sensory blockade was evaluated with a pinprick test and was graded as follows: 0=no block and 1=no pain sensation. The sensory blockade of the median nerve was evaluated on the palm side of the third finger, the ulnar nerve on the palm side of the fifth finger, the radial nerve in the lateral portion of the back of the hand, and the MC nerve in the lateral portion of the forearm. Motor blockade was graded as follows: 0=no weakness; 1=incomplete motor block; and 2=complete motor block. Motor blockade of the median nerve was evaluated by flexion of the second and third fingers, the ulnar nerve by flexion of the fourth and fifth fingers, the radial nerve by abduction of the thumb, and the MC nerve by flexion of the elbow.
Surgical anesthesia was achieved when the sensory blockade reached stage 1 in all four nerves and the motor blockade reached stage 1 or 2. If the sensory blockade in any nerve did not reach stage 1 in 15 minutes after the procedure, it was considered a block failure and general anesthesia was initiated. Also, if the patients felt pain in any time during surgery, the surgery procedure was stopped, and the anesthesia method was switched to general. A successful blockade was achieved when there was no need for general anesthesia.
Patient sedation during surgery was achieved by a continuous infusion of propofol at 15-50 µg/kg/minutes, and was performed to reach 3-4 on the Modified Observer's Assessment of Alertness/Sedation Scale. After the surgery, if the patients wanted postoperative pain control, intravenous patient controlled analgesia was used.
Any adverse events were evaluated while performing the block and perioperatively. Adverse events from LA toxicity included: numbness of the tongue and lips, a metallic taste, tinnitus, disorientation, loss of consciousness, seizures, arrhythmias, respiratory arrest, and cardiac arrest. Adverse events from inadvertent blood vessel puncture (haematoma) and nerve damage (paraesthesia and numbness) were monitored.
The primary study outcome was the induction time. In our previous trial, the induction time for the PV1 technique was about 540 (SD, 200) seconds.
9 We presumed that the induction time of the PN technique is longer than the PV technique, and a time difference of 3.5 minutes was considered as clinically relevant. The significance level was accepted as 0.05, and alpha was adapted to 0.0167 by Bonferroni correction to correct for type-I errors due to multiple testing (number of testing=3). By a power analysis based on 90% power and considering 20% drop out rate, the number of subjects required for each group was calculated to be 29 patients.
Data management and all statistical analyses were performed using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA). One-way ANOVA was used for continuous variables, while the Kruskal-Wallis test was used for categorical variables to analyse the differences among groups. A p value less than 0.05 was considered to indicate significance.
RESULTS
The success rate was 89.7% in the PN group, 86.2% in the PV1 group, and 89.7% in the PV2 group, however, the differences were not significant (
p=0.893). The average performance time was 391.2 seconds (SD, 171.6) in the PN group, which was significantly longer than PV1 [192.8 seconds (SD, 59.0)] and PV2 [211.4 seconds (SD, 58.6)]. The average onset time was not significantly different. The average induction time was 673.4 seconds (SD, 149.6) in the PN group and was longer than PV1 [557.6 seconds (SD, 194.9)] and PV2 [561.5 seconds (SD, 129.8)]. There was a significant difference in the number of needle passes, with the most occurring in the PN group and the fewest in the PV1 group (
Table 2).
The numbers of axillary arteries and veins were 1-2 and 1-5, respectively, and there were no significant differences (
Table 3).
The sensory blockade of the four nerves was evaluated at 5 minutes intervals for 15 minutes following the procedure. The median, ulnar, and radial nerves were blocked significantly more in the PN group (
Fig. 1). There were no differences in the proportion of patients with a blockade at 5 minutes following the anesthetic procedure (
Fig. 1). There were no differences in MC nerve blockade at any time period. There were no differences between the PV groups at all time periods for all nerves.
Regarding the motor blockade, the median, ulnar, and radial nerves at 10 and 15 minutes had complete motor block, significantly more in the PN group (
Fig. 2). For the MC nerve block, there were no significant differences between the PN and PV1 groups, but fewer patients in the PV2 group had complete motor block than in the PN group at 5 minutes. There were no differences between PV1 and PV2 at all time periods for all nerves.
No vascular punctures occurred in the PN group, but did occur in two patients in the PV1 group and two in the PV2 group. No further complications, such as haematoma, developed. There was no LA toxicity symptoms or complications such as paraesthesia or continued numbness from nerve damage (
Table 3).
DISCUSSION
We compared a PN injection technique with two methods of PV injection using US-ABPB. The anesthetic procedure duration was longer for the PN group, and the onset time was not significantly different among the three groups. Consequently, the induction time was significantly longer in the PN group. Nevertheless, there were no significant differences in the success rates or adverse events. Therefore, single or multiple PV injection techniques can be used as an alternative method for US-ABPB.
Currently, US is used widely for ABPB. With US, the operator can approach the target site and avoid intraneural and intravascular injections. Recent studies showed that the success rate of US-ABPB had comparable results between PN and PV injection techniques.
4,
5,
6 This may be due to the visualisation of LA diffusion with real-time US. Imasogie, et al.
4 compared separately blocked median, ulnar, and radial nerves (PN group) using both US and a nerve stimulator with a single injection at the 6-o'clock position of the axillary artery (PV group), and reported a success rate of 88-89%. This was explained by the neurovascular sheath in the axilla. The time required to perform the block was longer in PN group, therefore, it was concluded that PV injection is effective and more time efficient. Bernucci, et al.
5 compared a PN block with a PV block at the 6-o'clock position and found a comparable success rate and total anesthesia time, however, the PV block resulted in fewer needle passes and less paraesthesia. Tran, et al.
6 conducted a study with three PV injection groups: a single injection in the 6-o'clock position, injections in the 6- and 12-o'clock positions, and injections in the 2-, 10-, and 6-o'clock positions. There was a comparable success rate, but the first group had fewer needle passes. Thus, a two injection US-ABPB protocol was recommended: one injection for the MC nerve and another around the axillary artery. These results are in good agreement with our findings, and show that sufficient surgical anesthesia can be achieved by PV injection for US-ABPB.
Although our previous study that compared two positions (6-o'clock and 12-o'clock) in PV single injection technique showed no differences in time effectiveness, success rate, and complications, it is highly desirable to find out whether 12-o'clock single injection is just as effective as PN injection or PV multiple injection.
9 And this investigation showed similar results in PV1 and PV2 groups and unfavourable results in PN group in terms of procedure time and induction time. LA does not tend to spread to areas where the surrounding tissues have a higher pressure. When performing infraclavicular BPB, injections posterior to the axillary artery are at higher pressures from the pectoralis major muscle which make the technique more effective.
10,
11 However, in case of axillary BPB, high pressure from the brachial fascia anteriorly and latissimus dorsi muscle fascia posteriorly allow effective injection at the 12-o'clock position. This fact might affect the comparative results between PV1 and PV2 groups.
The numbers of arteries and veins and their topographic relationship within the axillary sheath are important factors of block success. Orebaugh and Williams
12 suggested that abnormal axillary vascular anatomy could affect ABPB. In our study, only 14 patients had one axillary artery and vein, 7 had two arteries, and 72 had 2-5 veins (avg.=2.48). Multiple veins may interfere with the procedure, especially when the veins were located between the axillary artery and nerve. In these patients, PV injection failed and conversion to general anesthesia was needed in three cases in the PV1 group and one case in the PV2 group. This might be due to the increased distance between the injection site and nerve and disturbed LA diffusion. Anatomical variation of axillary vessels was related to failure in two cases in the PN group, because the vein altered the approach to the nerve. Both required general anesthesia.
A patient from PV1 group required general anesthesia because the median, ulnar, and radial nerves were insufficiently blocked. However, when the block was reassessed in the recovery room, the block was adequate. In this patient, the median nerve was at the 7-o'clock position and there was a large distance from the injection site. The LA had to cross three axillary veins that were close to axillary artery to reach the ulnar and radial nerves. In this case, we speculate that LA can diffuse globally in the axillary sheath, but may take a longer time due to individual anatomy.
The success rate in the present study was similar or slightly lower compared to previous studies: 87.9-89.3% Imasogie, et al.,
4 90-97.5% Tran, et al.,
6 and 92-96% Bernucci, et al.
5 We evaluated the blockade for only 15 minutes, which is shorter than that in other studies (30 minutes). Disinfection and draping for surgery preparation took 20-30 minutes following the block procedure, so we chose a 15 minutes observation time, considering the rapid onset and short duration of lidocaine. The patient mentioned above may not have needed general anesthesia if the observation time was longer. Bernucci, et al.
5 used 24 mL, as did our study, but Imasogie, et al.
4 used 30 mL and Tran, et al.
6 used 28 mL. Despite this, we achieved an 80.8-88.5% success rate. This was greater than the proportion of patients with full blockade at 15 minutes in the studies by Tran, et al.
6 and Bernucci, et al.
5
There was no direct nerve injury or hematoma from vascular punctures. The number of needle passes was lowest in the PV1 group with no difference in the success rate among the three groups. Both the procedure time and induction time were similar in PV1 and PV2 groups. The onset time was not significantly different among the three groups. Given these results, a single PV injection for US-ABPB is a favorable method. Considering the diversity of axillary anatomy, a single PV injection may not be adequate to reach the level of surgical anesthesia in some patients. Future study regarding whether fewer needle passes actually decreases the risk of complications and increases patient satisfaction is necessary.
In conclusion, a PV injection technique consisting of a single injection in the 12 o'clock position above the axillary artery in addition to a MC perineural injection is an effective method for US-ABPB. This technique has a high success rate, and less time than the PN injection technique. Thus, PV injection may be valuable for high-volume clinics and in patients with anatomical variation in whom it is difficult to identify individual nerve.








 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download