Abstract
Peripartum cardiomyopathy (PPCM) is a rare entity, and anesthetic management for cesarean section of a patient with this condition can be challenging. We hereby present the anesthetic management of a patient with PPCM complicated with preeclampsia scheduled for cesarean section, along with a mini review of literature. A 24 year-old primigravida with twin gestation was admitted to our hospital with severe PPCM and preeclampsia for peripartum care, which finally required a cesarean section. Preoperative optimization was done according to the goal of managing left ventricular failure. Combined spinal epidural (CSE) anaesthesia with bupivacaine and sufentanil was used for cesarean section under optimal monitoring. The surgery was completed without event or complication. Postoperative pain relief was adequate and patient required only one epidural top up with sufentanil 6 hours after operation. To the best of our knowledge there is no report in literature of the use of sufentanil as a neuraxial opioid in the anesthetic management of cesarean section in a patient with PPCM. CSE with sufentanil may be a safer and more effective alternative in such cases.
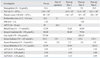
Peripartum cardiomyopathy (PPCM) is by definition a primary myocardial disease without any demonstrable cause and having onset during the last month of pregnancy or in the first five months after delivery.1 Echocardiographic features of left ventricular dysfunction were added to the modified definition later to make it more precise (Table 1).2,3 PPCM may be associated with preeclampsia and the clinical scenario can worsen heart failure.1,4-20 Anesthetic management of cesarean section in PPCM patients can be a challenge to the anesthesiologist.5,8,10,21,22 Correct choice of anesthesia and precise titration is crucial for a favorable outcome. We present the anesthetic management of such a patient along with a small relevant literature review.
A twenty-four year-old primigravida weighing fifty kilogram (kg) was admitted to a cardiac center at thirty-two weeks of gestation with complaints of increasing breathlessness and generalized swelling for two weeks without any prior coexisting medical illnesses. She was diagnosed with peripartum cardiomyopathy complicated with preeclampsia based on clinical and echocardiographic findings (Table 2) and was put on oral digoxin 0.25 mg (five days a week), furosemide 40 mg once daily, carvedilol 3.125 mg twice daily and potassium supplements. She was referred to our hospital for further management.
Treatment was started in the intensive care unit by a multidisciplinary team of physicians with a plan to control her heart failure medically and to induce fetal lung maturation by dexamethasone before elective delivery.12 Because of intrauterine death (IUD) of one fetus (as revealed by repeat ultrasonogram) and progressive deterioration of cardiac status and liver function tests (LFT) (Table 3), a decision was made to electively terminate the pregnancy by cesarean section.
Preanaesthetic examination revealed pulse rate (PR), blood pressure (BP), peripheral oxygen saturation (SpO2) and respiratory rate of 80 beats/min, 90/70 mmHg, 90% on room air and 15/min, respectively. The chest was found to be clear on auscultation. Examination of the cardiovascular system (CVS) showed a third heart sound and an ejection systolic murmur in the mitral area. The preoperative echocardiogram showed dilated cardiac chambers, global hypokinesia with a left ventricular ejection fraction (LVEF) of 25% and moderate pulmonary arterial hypertension (PAH) (Table 2). Significant laboratory investigations were borderline derangement in LFT, coagulation parameters, marginal leucocytosis and platelet count of 98 × 109/L (Table 3). The anesthetic plan of performing the procedure under combined spinal epidural (CSE) after optimization of cardiovascular and coagulation status was discussed with the parent team and the patient, who gave informed consent.
The preoperative optimization process was initiated. Invasive arterial and central venous accesses were established. Dopamine and dobutamine infusions were started and titrated to optimize her cardiovascular variables. She received fresh frozen plasma (FFP) for correction of her coagulation status. Intravenous ranitidine (50 mg) and metoclopramide (10 mg) and oral sodium citrate solution (0.3 M, 30 mL) were given 30 minutes before transferring her to the operating room (OR). Standard ASA monitors along with invasive blood pressure (IBP), central venous pressure (CVP) and urine output were used for intraoperative monitoring. Oxygen was administered via facemask at 4 L/min. Her preoperative heart rate (HR), mean arterial pressure (MAP), CVP, and SpO2 were 108/min, 65 mmHg, 15 mmHg and 94%.
The CSE technique consisted of sitting position and midline approach at L3-L4 interspace. The epidural space was identified by loss of resistance to saline on the first attempt with an 18G Tuohy needle (Portex). A subarachnoid block (SAB) was done by 27G Whitacre needle by needle through needle technique and 1.2 mL of 0.5% heavy bupivacaine (6 mg) with 7.5 µg of sufentanil was injected after free flow of cerebrospinal fluid (CSF). An 18 gauge epidural catheter (EC) was threaded up to the length of four cm into epidural space. A fifteen cm wedge was placed under the left hip to maintain a left lateral tilt. Level of block (response to ice cube) was checked at 3, 5 and 10 minutes and was found to be up to thoracic 10th, 8th, 6th segment level respectively. Effective onset of block resulted in some improvement of MAP, SpO2 and clinical symptoms. Surgery went ahead without event and both the living baby and dead fetus were delivered. Apgar scores of the baby at 1 and 5 minutes were 7 and 9 respectively. Intravenous oxytocin drip (15 units/500 mL of saline at 40 drops/min) was started slowly after delivery. Intravenous furosemide 10 mg and midazolam 2 mg were given incrementally at this time. Dopamine and dobutamine infusions were continued throughout the surgery titrated to the hemodynamics. The total estimated blood loss was about 250 mL during the hour-long procedure. Intravenous fluid replacement was targeted to maintain the CVP of 12 to 14 mmHg, and 750 mL of Ringer's Lactate (RL) was given intraoperatively. Urine output was 75 mL without any episode of adverse hemodynamic events. Intraoperative parameters like heart rate (HR), mean arterial pressure (MAP), CVP and SpO2 remained within 20% of the preoperative value.
The patient was transferred back to the ICU after the procedure. She remained absolutely pain free for the next six hours and the EC was removed after administration of 20 µg of sufentanil in 10 mL NS. Furosemide and digoxin were restarted and FFP transfusion was continued q6h for a day with close monitoring of coagulation profile. Clinical improvement was evident from post-operative day (POD) 2, with a decrease in ionotrope requirement and an improvement in LFT. Patient had mild dyspnea on POD 3 and a chest radiograph showed signs of pulmonary edema, which was relieved by furosemide. Gradually she was weaned off dobutamine completely and restarted on carvedilol. Oral captopril 6.25 mg, spironolactone 25 mg once daily and DVT prophylaxis with 5,000 U unfractionated heparin were added on POD 4. The remainder of her postoperative stay was uneventful. Her LFT, serum creatinine, and uric acid levels showed a decreasing trend corresponding with her improved clinical condition (Table 3). Repeat echocardiography on POD 6 showed severe generalized left and right ventricular hypokinesia with further reduction in ejection fraction to less than 25% (Table 2).
She was later transferred back to the cardiac center, where she underwent placement of temporary pacemaker for resistant bradyarrhythmia with some symptomatic improvement without any change in echocardiographic findings. As per the latest verbal information from cardiac center, she continues to have features of moderate ventricular dysfunction while the baby is doing fine. She was strongly advised against any future pregnancies.
PPCM is a severe form of heart failure which was first described by Demakis and Rahimtoola1 comprising of 3 criteria; namely, 1) Development of heart failure in the last month of pregnancy or within the first 5 months of postpartum, 2) Absence of any determinable cause of cardiac failure and/or 3) Any prior demonstrable heart disease. Later, echocardiographic evidence of left ventricular dysfunction was added by the PPCM workshop committee of the National Institute of Health (NIH) (Table 1).2,3 The time period in the definition was specified to exclude congenital and acquired causes of heart failure which may as well be present in the earlier stages of pregnancy although some cases of PPCM have been re-ported to occur outside this time limit.1,2,5,7-9,11,13,21-27 Although the earlier reported incidence was 1 in every 3,000 to 15,000 live births,1,4,5 more recently reported incidence in the USA was about 1 in every 1,485-4,000 pregnancies, thus indicating an increasing trend, and even more so in African-Americans.2,5,7,8,14-16,25,28-32 This increased incidence may be due to better health awareness and improved diagnostic modalities.27 But PPCM appears to occur more frequently in Haiti (1 in 300 live births)25 and in Africa (1 in 100 to 1,000 live births).6,9,25 A proper explanation for this much higher incidence of PPCM in some geographic areas is not yet known. Environmental or genetic factors, local cultural habits and re-porting, as well as diagnostic bias, may be some reasons for this higher incidence.6,14,15,18-20,32-34
Several risk factors that have been correlated to PPCM are: advanced maternal age, multiparity, multiple gestation, black race, African-American female, malnutrition, hypertension, preeclampsia, alcohol, cocaine and tobacco abuse, poor antenatal care, low socioeconomic condition, breast feeding and positive family history.1-11,13-18,20,25-30,32,35-40 Although PPCM has been reported to occur classically in cases with higher maternal age, parity and African race;1-10,15,21,22,25,32,36-39,41 recently it has been found to occur increasingly in younger age groups, and in primigravida and white mothers as well.5-11,13,14,16,17,19,20,22,23,25,32,35,41-46 Most of the researchers agree that PPCM commonly occurs in twin pregnancies.1,4,5,8,9,13,14,20,25,26,28,37 Preeclampsia and hypertension has been frequently reported to be associated with PPCM cases.1,4-20 The similarities in immunopathologic process involving prolactin, matrix-metalloproteinase (MMP) and graft vs. host reaction between preeclampsia and PPCM strongly support this association.19,47-49 Some authors even described it as a hypertensive heart failure and described it as a significant risk factor for PPCM.6,16,44 Initially, breast feeding, malnutrition, poor socioeconomic condition and antenatal care were implicated as risk factors;1,5,38 however, no such correlations have been found in recent reports.5,7,37 Likewise, although substance abuse and familial occurrence have been causally implicated,2,10,11,37 they should be regarded as a variety of cardiomyopathy.5,8 All the reported risk factors are quite old, predating modified definition and echocardiography. Thus, further evaluation will be neces-sary, keeping in mind advances in medical technology.5,10
Proper etiology of PPCM is unclear and several etiologies such as inflammation (myocarditis, cytokines), viral infection, autoimmunity, abnormal response to the hemodynamic stress of pregnancy, cytokine-mediated inflammation, Gq-related myocyte apoptosis, oxidative stress-induced Cathepsin D production which produces defective prolactin leading to endothelial damage and apoptosis of vascular cells, prolonged tocolysis, and selenium deficiency have been proposed.1-11,13,15,16,19,25,28-31,33,35-38,40,46-52 There is stronger literary evidence to support inflammation, viral infection, 16 kDa prolactin induced apoptosis and autoimmunity as possible etiology of PPCM.2,3,5,6,9,13,19,25,27,29-31,33,34,36,37,46-52 Thus, it is more likely that etiology is multifactorial.7,13,25,28,33 New targeted research directing towards inflammatory, viral, prolactin and autoimmune etiologies are needed using modern molecular and biochemical techniques to find out actual reason behind PPCM.13,25,37
PPCM clinically presents with orthopnea, dyspnea upon exertion, palpitation, chest pain, headache, cough and malaise suggestive of left ventricular failure.1-8,12,14,21-31,36,39-42,45 The majority of patients present with severe heart failure [New York Heart Association (NYHA) physical class III or IV].7,8,14,18,25,27,34,36 However, the actual categorization used by NYHA in advanced pregnancy can be confounded by the physiological changes of pregnancy.20,30,31 Ventricular and supraventricular tachyarrhythmias, intracardiac thrombi, features of systemic embolism such as chest pain, haemoptysis and hemiplegia due to acute myocardial infarction, pulmonary and cerebral embolism, infarction of the spleen and kidney, mesenteric artery occlusion, limb gangrene, and finally multiorgan failure have all been reported as either as presenting symptoms or complications of PPCM.1,4-6,8,10,16,20,21,23,25,27,30,31,34,37,39,42
PPCM is a diagnosis of exclusion after ruling out other common causes of heart failure, such as toxic, metabolic, ischaemic or valvular heart diseases.1,8,25,27,30,40 Early diagnosis of PPCM is difficult because of physiologic changes of advanced pregnancy.2,3,5,30,37 Certain complications of pregnancy such as anemia, toxemia and amniotic fluid embolism may have similar clinical presentation.5 However, PPCM usually presents in postpartum period (72-93%) when physiologic changes of pregnancy should be normalizing.1,4,5,7,9,17-20,27,31,34,40 Thus, if a patient presents with persistent or worsening congestive heart failure especially in puerperium, the possibility of PPCM should always be considered as delay in diagnosis is often associated with increased morbidity and mortality.2,25,30 A few asymptomatic cases of PPCM have also been reported.25,39 Routine investigations done to confirm the diagnosis are ECG, chest X-ray (CXR), and Doppler echocardiography.7,30 ECG usually shows sinus tachycardia, low voltage complexes, ST-T changes, conduction defects, left axis deviation and ventricular hypertrophy.1,2,4,5,12,18,21-23,25,29,30,34,39 Other arrhythmias such as supraventricular, ventricular extrasystoles, and ventricular tachycardia may occur.1,4,16,23,34,37,39,42 Common CXR findings are cardiomegaly, pulmonary edema and pleural effusion.1,4,5,12,21-23,27,29,30,39,41 As CXR features are nonspecific, routine use of X-ray should be discouraged during pregnancy.40 However, absolutely normal ECG and CXR have been reported.4,5,29 This makes echocardiography the most valuable and confirmatory diagnostic tool.2,27 Patients may present features of severe ventricular dysfunction such as increased left ventricular end diastolic diameter (LVEDD), left ventricular end systolic diameter (LVESD), decreased left ventricular fractional shortening (LVFS) and LVEF, right ventricular dysfunction, valvular regurgitation, regional wall motion abnormality, pulmonary arterial hypertension (PAH) as well as intra cardiac thrombi.2,3,5,7-12,18,21-23,25,26,29,30,35,36,39,41-44 Valvular regurgitant lesions are the consequence of cardiac dilatation.5,26 Magnetic resonance imaging (MRI) and computerized topographic scans are more sensitive diagnostic tools for detection of cardiac thrombus.5,10 Cardiac MRI has become an attractive modality to assess cardiac function and to distinguish etiologic nature of PPCM.27,31,53,54 Delayed gadolinium enhancement (DGE) can help to detect inflammatory myocarditis and should be used in patients who do not respond to standard heart failure management.27,54 The detection of DGE in order to detect myocardial fibrosis has been indicated as a good prognostic factor.27,53 Cine MRI can be used as an alternative to detect all the pa-rameters like echocardiography.54 Currently, routine use of endomyocardial biopsy is somewhat controversial.5,8,10,25,30,37 It may be considered if the patient does not improve after two weeks of conventional management.5,7,9,25,28,37 Routine haematological, biochemical, serological and blood culture studies are used to rule out other causes of heart failure.4,5,23 Polymerase chain reaction and immunohistochemistry techniques should be used to rule out viral and autoimmune etiology in suspected cases.27,34 Estimation of C-reactive protein (CRP), Interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), Fas-Apo-1, interferon-γ (IFN-γ), and N-terminal-pro Brain natriuretic peptide (NT-proBNP, a serum marker of heart failure), serum prolactin should now be strongly considered in light of current evidence of the inflammatory and autoimmune nature of PPCM.5,25,27,29,36,46,49,52
Medical therapy for PPCM follows the routine principles of management of heart failure and is aimed at reduction of preload, afterload and increase in cardiac contractility through judicious use of bed rest, salt restriction, diuresis, digitalization, vasodilators, β-blockers and anticoagulants.1,2,4,5,8,10,14,17,25-31,36-42,51 Safety of drugs during pregnancy and lactation should be kept in mind.2,31,37 Though strict bed rest used to be advised earlier on,1,38 the current recommendation is a gradual increase in activity as tolerated, after the initial distressing symptoms are relieved by drugs, as this has been shown to improve outcome.1,2,28,30 Salt and fluid restriction has been advised only in severe PPCM cases.2,23,25,41 Digoxin is considered safe during pregnancy and lactation, but patients should be carefully monitored, especially when it is used along with diuretics, because parturients show an increased sensitivity.1,5,25,30,38,55 Diuretics have been indicated to relieve symptoms of fluid overload.12,25,27,29 They are safe when used carefully, but can inadvertently cause hypokalemia and hypovolemia, which may lead to placental hypo-perfusion.25,36 When combined with conventional medical management, spironolactone has been shown to improve outcomes for PPCM patients because of its anti-aldosterone action. However, its safety during pregnancy has yet to be proven.5,28 Vasodilators are now considered vital for a positive outcome in PPCM.5,28 Angiotensin-converting enzyme inhibitors (ACEI) or angiotensin II receptor blockers (ARB) are now a mainstay of congestive cardiomyopathy management.5,8,25,28,29,31,36,37 They are contraindicated during pregnancy because of their teratogenecity; however, they can be considered to treat especially resistant heart failure when the benefit outweigh the risks, or after delivery.2,5,8,25,28,30,31,37 These groups of drugs are excreted in milk and may prevent breast feeding if their use is warranted.5 During the antepartum period, hydralazine, with or without nitrates, is the vasodilator of choice and has been shown to reduce mortality.2,5,25,27-31,38 This is the second tier drug after ACEI/ARB in this regard during the postpartum period.5,28 In severe cases, intravenous nitropruside, nitroglycerin, or nesiritide may be used.5,21,22,26,30,37,41 Nitropruside should be avoided during the antepartum period due to the risk of fetal cyanide toxicity.5,29,30,37 Calcium channel blockers (CCB) were earlier avoided in heart failure because of their negative inotropic effect;2,5,37 a few recent studies have shown that amlodipine improves survival and reduces interleukin-6 (IL-6) level in heart failure, indicating a role in management of PPCM patients.2,5,37 Levosimendan, a calcium sensitizer with vasodilator property, has successfully been used in PPCM patients. This results in the reduction of elevated pulmonary capillary wedge pressure (PCWP) and improvement of ventricular dysfunction, thus allowing for earlier weaning from inotropes.43 Similarly, beta blockers were also initially contraindicated in heart failure patients due to their negative inotropic properties. Recent studies have shown that beta blockers such as carvedilol actually improve outcome.2,5,28,37 Although beta blockers are associated with low birth weight babies, they are not absolutely contraindicated in pregnancy.37,55 Both beta blockers and ACEI have been shown to suppress immune response in patients with PPCM.5,19,25,51 This may be beneficial considering the increased evidence for autoimmune etiology.2,5,25,28,56
Antiarrhythmic agents may be required for control of arrythmias. No antiarrhythmic agent is fully safe in pregnancy. Drugs with the highest safety profiles should be considered first.5,55 Digoxin and β-blockers have been used safely.55 Though amiodarone is toxic during pregnancy, it can be considered in resistant arrhythmias when weighing the risks and benefits.55 Pacemakers and automated implantable cardioverter defibrillators (AICD) are options for refractory and life-threatening arrhythmias for those who have LVEF of less than 25% because of higher incidence of ventricular arrhythmias in this group of patients.2,5,9,20,23,28,31,37,51,55
The incidence of thromboembolism is reported to be very high in PPCM patients having LVEF < 35% and LVFS < 15% with atrial fibrillation,1,2,4,5,10,25,28,31,36,37 and patients usually need prophylactic heparin (unfractionated/fractionated) during the antepartum and heparin/warfarin during the post partum period.5,20,21,25,28-31,36,37,40,51
Currently, the role of immunosuppressive therapy (azathioprine and prednisolone) in PPCM is controversial,5,25,37 but may be considered for patients not responding to conventional management for two weeks and an endomyocardial biopsy reveals myocarditis.2,5,7,25,37,44 Even though the role of immunoglobulin has been questioned, it has been used successfully in PPCM.28,56 Considering the increasing evidence of autoimmunity, it can be tried in refractory cases.5,19,25,28,57 Recently, pentoxifylline, an immunomodulating agent, has been shown to improve physical status (NYHA class) and LVEF when added with conventional drugs therapy of PPCM.25,28,36,37 Bromocriptine or its congener cabergolin has recently emerged as the causative treatment of PPCM because of emerging evidence of role of 16 kDa fragment of prolactin in the causation of PPCM.6,27,30,46,52 This group of drugs has been shown to improve ventricular dysfunction and to encourage normalization of NT-proBNP, CRP, NYHA class, and LVEF when given to PPCM patients along with standard heart failure therapy, which has shown a real prospect for the etiologic treatment of PPCM.27,33,46,52 Routine use of bromocriptine may result in the suppression of lactation, which may deprive the infant of essential nutrition and sometimes cause acute myocardial infarction.58 Moreover, a larger randomized controlled trial is needed to comment firmly on bromocriptine's role in PPCM.31 According to current literature, it may be considered in severe cases.27,33,46,52
Heart transplant is reserved for those young patients resistant to medical treatment with minimal systemic damage.2,5,7-11,25,27,28,30,31,35,37,40,59 Patients with less than 25% of LVEF end up requiring heart transplant for survival in first or subsequent pregnancies.17 Aggressive measures such as an intra aortic balloon pump (IABP), a ventricular assist device (VAD), veno-atrial bypass, and an extracorporeal membrane oxygenator (ECMO) may be needed in severe cases as a bridging measure for heart transplant.5,10,20,23,27,28,31,40,51,59,60
PPCM in the antepartum period requires management by a multidisciplinary team consisting of cardiologists, obstetricians and intensivists as the lives of both mother and fetus are at stake.2,5,12,21,28,37,45,57 Induction of labour is considered if patient's condition worsens despite maximal medical management.5,9,21,28,37 Labor analgesia is favored because of its ability to reduce sympathetic stress response of labor pain.5,42,61,62 Although a graded epidural is most often used for labor analgesia in PPCM,5,41,61 combined spinal epidural (CSE) and continuous spinal analgesia (CSA) may be better choices (the reasons for this are described later).5,26,41,42,61 Forceps and vacuum devices should be used liberally to reduce the hemodynamic stress of 2nd stage of labour.29,37 Cesarean section is mostly reserved for obstetric indications, but it may be considered in the case of a rapidly decompensating patient where maximum medical therapy fails.5,9,10,12,21,28,37,45,57 These patients will need to be monitored in the ICU for the initial 2-3 postoperative or post-delivery days due to increased risk of pulmonary edema caused by fluid overload and post-anesthetic cardiac dysfunction.5,6,12,20,35,37,44 NYHA class III or IV patients require ICU admission for aggressive management with invasive monitoring, ionotropic, mechanical circulatory and ventilatory support, and ECMO for preoperative optimization.2,5,20-23,26,28,37,41,60,62 Apart from classical inotropes, inodilators like dobutamine, amrinone, milrinone, enoximone and levosimendan may be beneficial in selective cases.5,22,29,30,37,59,60
Cesarean sections in PPCM patients have been performed under general as well as regional anesthesia.21-24,26,39,41,42,45,57,62 General anesthesia is mostly used in emergency surgery or when regional anesthesia is contraindicated,12,21,22,28,39,41,42 and it offers the advantage of controlling airway and ventilation.5,26,42,61 But, hemodynamic stress from rapid sequence induction can be dangerous if opioids are not used to prevent fetal respiratory depression.5,42 Though both inhalation and intravenous anesthesia have been used in PPCM cases,21,22,39,41,42,45 both of these techniques can lead to materno-fetal cardiorespiratory adverse effects which may sometimes require naloxone for reversal.22,39,41,42 Cardiac arrest following general anaesthesia in PPCM cases is also reported.39,41 General anaesthesia adds to the already existing risk of thromboembolism.21 Vasodilators may be required to accommodate the extra volume released from uterine autotransfusion after delivery of the fetus to prevent acute cardiac failure and pulmonary edema.5,26
Regional anesthesia on the other hand can be advantageous in PPCM because of sympatholysis-induced reduction of preload and afterload.42,57,61,62 Single-shot spinal anesthesia is not recommended due to uncontrolled sympathetic blockade and acute hemodynamic instability which may precipitate an adverse cardiac event including arrest.41,52 Carefully titrated epidural anesthesia has been used in majority of cases because of its hemodynamic stability.41,42,57,62 The major disadvantages of this technique are failure or partial anesthesia which may lead to forced conversion to general anesthesia.26 CSE has been successfully used in patients with PPCM and found to have lower rate of failure, smaller drug requirement, easy titrability with fewer hypotensive episodes (as it can be precisely titrated), faster onset with excellent analgesia, and better patient satisfaction and postoperative pain score.5,12,26,37,42 Other disadvantages such as technical difficulty and post dural puncture headache (PDPH) may rarely be encountered when a 27-gauge pencil point spinal needle is used.26,61 Some anesthesiologists have successfully used continuous spinal anesthesia (CSA) for caesarian section in patients with severe PPCM.26,61 CSA has theoretical advantages over CSE in terms of rapid onset with precise titrability requiring less local anesthetic, but it can be associated with higher incidence of PDPH and neurological complications.5,26,37,41,61 Avoidance of microcatheter and lignocaine has resulted in reduction of these complications.26,61
Local anesthetic infiltration along with bilateral ilio-inguanal nerve block is a novel technique for cesarean section with minimal hemodynamic effects.24 Unfamiliarity with the technique and higher incidence of failure are major obstacles to its routine implementation,5,26 but it can be considered in extreme cases. Although cesarean sections have been successfully conducted in PPCM patients with routine non-invasive monitoring,62 echocardiography and invasive parameters (IBP, CVP and/or PCWP) are usually monitored during anesthesia.5,12,21,22,26,39,41,42,45,57,60-62 The benefits of invasive and advanced monitoring may outweigh all arguments against it in severe cases.
Postoperatively, these patients should be routinely monitored in an ICU as they may require a ventilator, inotropic agents, and mechanical circulatory support due to a higher risk of congestive heart failure.5,9,12,21-23,28,39,41,42,61 Parenteral opioids or regional techniques are used to manage postoperative pain.5,21,26,42,45 Anticoagulant should be restarted early in view of higher risk of thromboembolism.5,21 All preoperative medications should be resumed. Drugs with teratogenic potential such as ACEI/ARBs and warfarin can be safely used after delivery and proper counseling for breast feeding.37
Prognosis of PPCM is related to presentation as well as to recovery of ventricular dysfunction.1-5,11 Though about 30-50% recovery of ventricular dysfunction was reported earlier,1,4,5 currently 60-90% to even complete echocardiographic recovery is reported if LVEF and LVESD on presentation is ≥ 27% and ≤ 5.5 cm.5,8-10,18,20,26,34,41,63 Basal level of NT-proBNP and IFN-γ may be a better predictor in this regard.49 Full recovery is documented by attainment of NYHA class I and LVEF of more than 50%.18,27,64 This recovery may take 1-2 years, as compared with the classic 6-month time period.27 Those who have persistent LVEF of less than 40% at 3 months or less than 20% at 1-2 months after diagnosis and treatment fail to improve.51 Those with a baseline LVEF of 25% had the worst prognosis and a higher rate of requiring heart transplant for survival.17 This risk was also found not to be modified by subsequent recovery of LVEF after delivery. This specific group of patients may benefit from cardiac MRI, catheterization and endomyocardial biopsy, and may need aphresis, immunoadsorption, intravenous gamma globulin, immunomodulation and antiviral therapy.27,51 Those who do recover have a good survival rate.4,5,25,35 Reduction of NT-proBNP and CRP level indicates good recovery of ventricular function. These markers can be monitored to evaluate the prognosis of PPCM.65 The earlier 25-85% mortality rate was reported in patients with persistent or deteriorating cardiac dysfunction,1-5,28,38 and the current mortality rate has been reduced to about 0-9% in PPCM cases.5,7-10,15,25,27,28,31,32,35,37 The higher mortality in the past was probably due to diagnostic bias and lack of modern heart failure management technology.20 The current trend of improvement is due to advances in medical management.5,9,10,35,37 Comparatively higher mortality (10-30%) and lower rates of recovery of ventricular function (25-35%) have been reported from Africa, Haiti, Turkey and the African-American population in USA.14,18,27,64 Race, ethnicity, lack of advanced medical facilities, and lower socioeconomic condition may play a role in this relatively poorer outcome.14,15,20 A substantial number of these deaths could be prevented with modern medical care.20 Advanced age, multiparity, multiple gestation, African origin, African-American and Hispanic ethnic group, delayed postpartum presentation, coexisting diseases, cardiac thrombus, higher QRS time, LVEDD, LVESD, pulmonary artery pressure, PCWP and reduced LVFS, LVEF, delay in management, higher basal level of NT-proBNP, IFN-γ, prolactin, TNF-α have been cited as poor prognostic criteria.1,4,5,10,18,20,25,27,29,31,49
Recurrence of PPCM in subsequent pregnancies is frequently reported.1,4,5,25,27,38,66 PPCM patients with persistent ventricular dysfunction have a higher risk of mortality in future pregnancies.4,5,25,66 Fett, et al. found that 46% of patients who had LVEF of less than 55% before pregnancy had a relapse of heart failure in subsequent pregnancies, compared to only 17% relapse of heart failure in those who had LVEF of more than 55% before pregnancy. They suggested that presenting LVEF during pregnancy may an important determinant for relapse of heart failure in subsequent pregnancies.66 It is not fully clear, however, whether patients with improved cardiac function can safely become pregnant again.2,5 There remains the risk of further cardiac damage in subsequent pregnancies.2,5,9,25,28,37 Recently, one researcher found that even patients whose LVEF was normalized (over 40%) after delivery still had a higher chance of recurrence and worsening heart failure in subsequent pregnancies if the baseline LVEF was less than 25%. Such patients should thus be strongly counseled against future pregnancies.17 Dobutamine stress tests have shown ventricular contractile reserve to be severely impaired in patients showing echocardiographic normalization of cardiac dysfunction.67 Researchers strongly advise against future pregnancies for patients with persistent ventricular dysfunction.1,4,5,37 But with currently improved life expectancy and medical management, it may not be always justified to rule out further pregnancy in patients who recover full ventricular function.5,31,55,63 If unavoidable, subsequent pregnancies should always be managed by a multidisciplinary approach.2
Our case report once again supports the recently increasing trend of PPCM in young primigravida. patient's low body weight corroborates the average build of rural Indian population due to malnutrition and poor access to health care. Though cases occurring in last month of pregnancy are included in the classic category of PPCM, cases like ours presenting outside the time range are also categorized as PPCM in literature.9,11,12,21-26,39,41,45 The increased hemodynamic load of twin pregnancy with superadded preeclampsia resulted in earlier presentation in our patient. The absence of prior cardiac illness, typical clinical presentation, echocardiographic features, and the persistence of ventricular dysfunction after delivery confirmed the diagnosis of PPCM.1,2,4 Preeclampsia was diagnosed based on her presenting BP (152/94 mmHg) and proteinuria (grade ++). Her high uric acid level also supported the diagnosis (Table 3).68 Co-occurrence of preeclampsia and PPCM has been reported in literature and is usually associated with higher morbidity and mortality.1,4-20 In our patient, deranged LFT and coagulation parameters caused by the preeclampsia complicated the severe heart failure. The obstetrician ruled out possibility of Hemolysis, Elevated liver enzymes, Low platelet count (HELLP) syndrome, as the laboratory parameters did not fit the classic picture.
Though termination of pregnancy by cesarean section in PPCM is reserved for obstetric indications, it was done in our patient because of fetal death, rapid worsening of cardiac failure and deteriorating laboratory parameters. A multidisciplinary approach was taken for preoperative optimization with standard management of cardiac failure and correction of coagulation parameters as per literature.2,5,8,12,21,28,37,42 Heparin was not started preoperatively as the patient's coagulation profile was deranged. ACEI was avoided in antepartum period for obvious reasons of teratogenecity.
We did not preload the patient prior to CSE as we were monitoring the CVP to avoid fluid overload. Although coagulopathy is a relative contraindication for regional anesthesia, the deranged coagulation parameters were corrected and specific precautions were taken as per standard guidelines before performing CSE.69
A low dosage of intrathecal bupivacaine was used to avoid excessive hypotension and associated complications. We used a slightly higher dosage of intrathecal sufentanil to reduce local anaesthetic requirement and to provide prolonged analgesia, and our patient did not require any epidural top-ups during the surgery.70 This may be advantageous as compared to the use of intrathecal fentanyl, where frequent top ups were required.26,42 This has helped us to avoid epidural-induced hypotension, which would have required vasopressor for management of its adverse consequences in a already cardiac compromised patient.12 Prolonged duration of analgesia seen with neuraxial sufentanil may be because of its higher potency and affinity to opioid receptors.71 No major materno-fetal cardiorespiratory complications occurred, as evidenced by the stable intraoperative vital parameters and the Apgar scores of the fetus. The patient complained of mild itching, which responded appropriately to antihistaminic. Though there are reports of use of intrathecal fentanyl in PPCM patients,26,42 use of sufentanil as an intrathecal opioid for CSE in PPCM patients has not been reported to date. In our patient, subarachonoid block with bupivacaine plus sufentanil was sufficient for operation and resulted in excellent postoperative analgesia for up to six hours. Physiological changes due to severe PPCM might have altered the pharmacokinetics and pharmacodynamics of the spinally administered drugs prolonging their duration of action. Therefore, we feel that sufentanil as an additive in CSE may be more advantageous for anesthesia as well as postoperative pain relief in PPCM patients. More studies are needed to clarify this issue.
Furosemide was used prophylactically to prevent fluid overload from uterine auto transfusion.41 Vasodilator infusion is also recommended at this stage,5,21,26 but this was not possible in our case because the patient was already on inotropes. There was significant symptomatic improvement after effective onset of the block as seen by the decrease in severity of respiratory symptoms and some improvement in BP as well as SpO2 due to sympatholysis caused by regional anesthesia establishing its superiority in PPCM.26,42,57,61
Although newer inodilators are more effective for managing biventricular failure,5,9,41 they were not available at our hospital, and a hypotensive state precluded their use. The epidural catheter was removed after the first top up dose under FFP cover as there was a plan to start DVT prophylaxis as soon as the coagulation profile normalized.69 Postoperative pain from cesarean section is not severe from the second postoperative day onwards, and can be managed by conventional analgesics.26
Dyspnea on the second postoperative day was probably due to volume overload and worsening pathology of PPCM, which was resolved with furosemide and titration of inotropes, confirming our assumption and this was a typical feature of PPCM.12,21,39 Standard medical management of PPCM was resumed gradually when oral feeding was started. ACEI, spironolactone, carvedilol were added at appropriate time. Although bromocriptine would have been a good choice considering the recent favorable evidence, it was not a good option in this patient due to the concern about depriving the neonate of breast milk.
Elective termination of pregnancy resulted in improvement in our patient's clinical and laboratory parameters (Table 3). However, worsening of her echocardiographic parameters indicates ongoing pathology resulting in persistent postoperative dysfunction. She required insertion of a pacemaker due to persistent bradyarrhythmia, which further supports the higher incidence of malignant arrhythmias in these patients.20 Our case report strengthens the association of bad prognosis in patients with PPCM with multiple gestation, associated preeclampsia presenting with low LVEF and PAH.
However, as a single patient case report does not carry much scientific weight, we decided to report, as it shows, that CSE approach with sufentanil as a neuraxial opioid can be a safe choice for anesthesia in this delicate subgroup of pregnant patients, if planned properly.
Anesthetic management of a patient with PPCM should be comprised of adequate preoperative optimization using a multidisciplinary approach, careful monitoring, proper use of anesthetic technique and vigilant postoperative care. Regional anesthesia using CSE with sufentanil may be a good choice for this subgroup of patients.
ACKNOWLEDGEMENTS
We are grateful for the help provided by Dr. Somnath Bose and Dr. Mandeep Singh in editing as well as facilitating the acquisition of relevant literature for the preparation of this manuscript.
References
2. Pearson GD, Veille JC, Rahimtoola S, Hsia J, Oakley CM, Hosenpud JD, et al. Peripartum cardiomyopathy: National Heart, Lung and Blood Institute and Office of Rare Diseases (National Institutes of Health) workshop recommendation and review. JAMA. 2000. 283:1183–1188.
3. Hibbard JU, Lindheimer M, Lang RM. A modified definition for peripartum cardiomyopathy and prognosis based on echocardiography. Obstet Gynecol. 1999. 94:311–316.
4. Demakis JG, Rahimtoola SH, Sutton GC, Meadows WR, Szanto PB, Tobin JR, et al. Natural course of peripartum cardiomyopathy. Circulation. 1971. 44:1053–1061.
5. Bhakta P, Biswas BK, Banerjee B. Peripartum cardiomyopathy: review of the literature. Yonsei Med J. 2007. 48:731–747.

6. Mayosi BM. Contemporary trends in the epidemiology and management of cardiomyopathy and pericarditis in sub-Saharan Africa. Heart. 2007. 93:1176–1183.

7. Midei MG, DeMent SH, Feldman AM, Hutchins GM, Baughman KL. Peripartum myocarditis and cardiomyopathy. Circulation. 1990. 81:922–928.

8. Ford RF, Barton JR, O'brien JM, Hollingsworth PW. Demographics, management, and outcome of peripartum cardiomyopathy in a community hospital. Am J Obstet Gynecol. 2000. 182:1036–1038.

9. Elkayam U, Akhter MW, Singh H, Khan S, Bitar F, Hameed A, et al. Pregnancy-associated cardiomyopathy: clinical characteristics and a comparison between early and late presentation. Circulation. 2005. 111:2050–2055.
10. Amos AM, Jaber WA, Russell SD. Improved outcomes in peripartum cardiomyopathy with contemporary. Am Heart J. 2006. 152:509–513.

11. Rizeq MN, Rickenbacher PR, Fowler MB, Billingham ME. Incidence of myocarditis in peripartum cardiomyopathy. Am J Cardiol. 1994. 74:474–477.

12. Pryn A, Bryden F, Reeve W, Young S, Patrick A, McGrady EM. Cardiomyopathy in pregnancy and caesarean section: four case reports. Int J Obstet Anesth. 2007. 16:68–73.

13. Ntusi NB, Mayosi BM. Aetiology and risk factors of peripartum cardiomyopathy: a systemic review. Int J Cardiol. 2009. 131:168–179.
14. Modi KA, Illum S, Jariatul K, Caldito G, Reddy PC. Poor outcome of indigent patients with peripartum cardiomyopathy in the United States. Am J Obstet Gynecol. 2009. 201:171.e1–171.e5.

15. Mielniczuk LM, Williams K, Davis DR, Tang AS, Lemery R, Green MS, et al. Frequency of peripartum cardiomyopathy. Am J Cardiol. 2006. 97:1765–1768.

16. Gentry MB, Dias JK, Luis A, Patel R, Thornton J, Reed GL. African-American women have a higher risk for developing peripartum cardiomyopathy. J Am Coll Cardiol. 2010. 55:654–659.

17. Habli M, O'Brien T, Nowack E, Khoury S, Barton JR, Sibai B. Peripartum cardiomyopathy: prognostic factors for long-term maternal outcome. Am J Obstet Gynecol. 2008. 199:415.e1–415.e5.

18. Duran N, Günes H, Duran I, Biteker M, Ozkan M. Predictors of prognosis in patients with peripartum cardiomyopathy. Int J Gynaecol Obstet. 2008. 101:137–140.

19. Gleicher N, Elkayam U. Peripartum cardiomyopathy, an autoimmune manifestation of allograft rejection? Autoimmun Rev. 2009. 8:384–387.

20. Goland S, Modi K, Bitar F, Janmohamed M, Mirocha JM, Czer LS, et al. Clinical profile and predictors of complications in peripartum cardiomyopathy. J Card Fail. 2009. 15:645–650.

21. Kaufman I, Bondy R, Benjamin A. Peripartum cardiomyopathy and thromboembolism; anesthetic management and clinical course of an obese, diabetic patient. Can J Anaesth. 2003. 50:161–165.

22. Zangrillo A, Landoni G, Pappalardo F, Oppizzi M, Torri G. Different anesthesiological management in two high risk pregnant women with heart failure undergoing emergency cesarean section. Minerva Anestesiol. 2005. 71:227–236.
23. Yahagi N, Kumon K, Nakatani T, Ishikawa T, Tanigami H, Eishi K, et al. Peripartum cardiomyopathy and tachycardia followed by multiple organ failure. Anesth Analg. 1994. 79:581–582.

24. Mellor DJ, Bodenham A. Infiltration anesthesia in the management of Cesarean section in a patient with peripartum cardiomyopathy. Anaesthesia. 1996. 51:409.

26. Velickovic IA, Leicht CH. Peripartum cardiomyopathy and cesarean section: report of two cases and literature review. Arch Gynecol Obstet. 2004. 270:307–310.

27. Tibazarwa K, Sliwa K. Peripartum cardiomyopathy in Africa: challenges in diagnosis, prognosis, and therapy. Prog Cardiovasc Dis. 2010. 52:317–325.

28. Phillips SD, Warnes CA. Peripartum cardiomyopathy: Current Therapeutic Perspectives. Curr Treat Options Cardiovasc Med. 2004. 6:481–488.

29. Egan DJ, Bisanzo MC, Hutson HR. Emergency department evaluation and management of peripartum cardiomyopathy. J Emerg Med. 2009. 36:141–147.

30. Moioli M, Valenzano Menada M, Bentivoglio G, Ferrero S. Peripartum cardiomyopathy. Arch Gynecol Obstet. 2010. 281:183–188.

31. Ramaraj R, Sorrell VL. Peripartum cardiomyopathy: Causes, diagnosis, and treatment. Cleve Clin J Med. 2009. 76:289–296.
32. Brar SS, Khan SS, Sandhu GK, Jorgensen MB, Parikh N, Hsu JW, et al. Incidence, mortality, and racial differences in peripartum cardiomyopathy. Am J Cardiol. 2007. 100:302–304.

33. Hilfiker-Kleiner D, Sliwa K, Drexler H. Peripartum cardiomyopathy: recent insight in its pathophysiology. Trends Cardiovasc Med. 2008. 18:173–179.
34. Lamparter S, Pankuweit S, Maisch B. Clinical and immunologic characteristics in peripartum cardiomyopathy. Int J Cardiol. 2007. 118:14–20.

35. Felker GM, Thompson RE, Hare JM, Hruban RH, Clemetson DE, Howard DL, et al. Underlying causes and long term survival in patients with initially unexplained cardiomyopathy. N Engl J Med. 2000. 342:1077–1084.

36. Sliwa K, Skudicky D, Bergemann A, Candy G, Puren A, Sareli P. Peripartum cardiomyopathy: analysis of clinical outcome, left ventricular function, plasma levels of cytokines and Fas/Apo-1. J Am Coll Cardiol. 2000. 35:701–705.

38. Burch GE, McDonald CD, Walsh JJ. The effect of prolonged bed rest on postpartal cardiomyopathy. Am Heart J. 1971. 81:186–201.

39. McIndoe AK, Hammond EJ, Babington PC. Peripartum cardiomyopathy presenting as a cardiac arrest at induction of anesthesia for emergency cesarean section. Br J Anaesth. 1995. 75:97–101.
40. Shaikh N. An obstetric emergency called peripartum cardiomyopathy! J Emerg Trauma Shock. 2010. 3:39–42.

41. Malinow AM, Butterworth JF 4th, Johnson MD, Safon L, Rein M, Hartwell B, et al. Peripartum cardiomyopathy presenting at cesarean delivery. Anesthesiology. 1985. 63:545–547.

42. Shnaider R, Ezri T, Szmuk P, Larson S, Warters RD, Katz J. Combined spinal-epidural anesthesia for Cesarean section in a patient with peripartum dilated cardiomyopathy. Can J Anaesth. 2001. 48:681–683.
43. Benezet-Mazuecos J, de la Hera J. Peripartum cardiomyopathy: a new successful setting for levosimendan. Int J Cardiol. 2008. 123:346–347.
44. Melvin KR, Richardson PJ, Olsen EG, Daly K, Jackson G. Peripartum cardiomyopathy due to myocarditis. N Engl J Med. 1982. 307:731–734.
45. Bilehjani E, Kianfar AA, Toofan M, Fakhari S. Anaesthesia with etomidate and remifentanil for cesarean section in a patient with severe peripartum cardiomyopathy--a case report. Middle East J Anesthesiol. 2008. 19:1141–1149.
46. Meyer GP, Labidi S, Podewski E, Sliwa K, Drexler H, Hilfiker-Kleiner D. Bromocriptine treatment associated with recovery from peripartum cardiomyopathy in siblings: two case reports. J Med Case Reports. 2010. 4:80.

47. Reuwer AQ, Reuwer PJ, van der Post JA, Cramer MJ, Kastelein JJ, Twickler MT. Prolactin fragmentation by trophoblastic matrix metalloproteinases as a possible contributor to peripartum cardiomyopathy and pre-eclampsia. Med Hypotheses. 2010. 74:348–352.
48. Hilfiker-Kleiner D, Kaminski K, Podewski E, Bonda T, Schaefer A, Sliwa K, et al. A cathepsin D-cleaved 16 kDa form of prolactin mediates postpartum cardiomyopathy. Cell. 2007. 128:589–600.
49. Forster O, Hilfiker-Kleiner D, Ansari AA, Sundstrom JB, Libhaber E, Tshani W, et al. Reversal of IFN-gamma, oxLDL and prolactin serum levels correlate with clinical improvement in patients with peripartum cardiomyopathy. Eur J Heart Fail. 2008. 10:861–868.

50. Hayakawa Y, Chandra M, Miao W, Shirani J, Brown JH, Dorn GW 2nd, et al. Inhibition of cardiac myocyte apoptosis improves cardiac function and abolishes mortality in the peripartum cardiomyopathy of Galpha(q) transgenic mice. Circulation. 2003. 108:3036–3041.

52. de Jong JS, Rietveld K, van Lochem LT, Bouma BJ. Rapid left ventricular recovery after cabergoline treatment in a patient with peripartum cardiomyopathy. Eur J Heart Fail. 2009. 11:220–222.

53. Mouquet F, Lions C, de Groote P, Bouabdallaoui N, Willoteaux S, Dagorn J, et al. Characterisation of peripartum cardiomyopathy by cardiac magnetic resonance imaging. Eur Radiol. 2008. 18:2765–2769.

54. Marmursztejn J, Vignaux O, Goffinet F, Cabanes L, Duboc D. Delayed-enhanced cardiac magnetic resonance imaging features in peripartum cardiomyopathy. Int J Cardiol. 2009. 137:e63–e64.
56. Bozkurt B, Villaneuva FS, Holubkov R, Tokarczyk T, Alvarez RJ Jr, MacGowan GA, et al. Intravenous immune globulin in the therapy of peripartum cardiomyopathy. J Am Coll Cardiol. 1999. 34:177–180.

57. George LM, Gatt SP, Lowe S. Peripartum cardiomyopathy: four case histories and a commentary on anaesthetic management. Anaesth Intensive Care. 1997. 25:292–296.

58. Hopp L, Weisse AB, Iffy L. Acute myocardial infarction in a healthy mother using bromocriptine for milk suppression. Can J Cardiol. 1996. 12:415–418.
59. Zimmerman H, Bose R, Smith R, Copeland JG. Treatment of peripartum cardiomyopathy with mechanical assist devices and cardiac transplantation. Ann Thorac Surg. 2010. 89:1211–1217.

60. Smith IJ, Gillham MJ. Fulminant peripartum cardiomyopathy rescue with extracorporeal membranous oxygenation. Int J Obstet Anesth. 2009. 18:186–188.

61. Okutomi T, Saito M, Amano K, Fukuoka K, Hoka S. Labour analgesia guided by echocardiography in a parturient with primary dilated cardiomyopathy. Can J Anaesth. 2005. 52:622–625.

62. Gambling DR, Flanagan ML, Huckell VF, Lucas SB, Kim JH. Anaesthetic management and non-invasive monitoring for caesarean section in a patient with cardiomyopathy. Can J Anaesth. 1987. 34:505–508.

63. Sutton MS, Cole P, Plappert M, Saltzman D, Goldhaber S. Effects of subsequent pregnancy on left ventricular function in peripartum cardiomyopathy. Am Heart J. 1991. 121:1776–1778.

64. Fett JD, Christie LG, Carraway RD, Murphy JG. Five-year prospective study of the incidence and prognosis of peripartum cardiomyopathy at a single institution. Mayo Clin Proc. 2005. 80:1602–1606.

65. Cénac A, Tourmen Y, Adehossi E, Couchouron N, Djibo A, Abgrall JF. The duo low plasma NT-PRO-BRAIN natriuretic peptide and C-reactive protein indicates a complete remission of peripartum cardiomyopathy. Int J Cardiol. 2006. 108:269–270.

66. Fett JD, Fristoe KL, Welsh SN. Risk of heart failure relapse in subsequent pregnancy among peripartum cardiomyopathy mothers. Int J Gynaecol Obstet. 2010. 109:34–36.

67. Dorbala S, Brozena S, Zeb S, Galatro K, Homel P, Ren JF, et al. Risk stratification of women with peripartum cardiomyopathy at initial presentation: a dobutamine stress echocardiography study. J Am Soc Echocardiogr. 2005. 18:45–48.

68. Williams KP, Galerneau F. The role of serum uric acid as a prognostic indicator of the severity of maternal and fetal complication in hypertensive pregnancies. J Obstet Gynaecol Can. 2002. 24:628–632.

69. Horlocker TT, Wedel DJ, Rowlingson JC, Enneking FK, Kopp SL, Benzon HT, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Third Edition). Reg Anesth Pain Med. 2010. 35:64–101.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download