1. Huang YC, Ni YH, Lai HS, Chang MH. Corrosive esophagitis in children. Pediatr Surg Int. 2004. 20:207–210.
2. Song HY, Han YM, Kim HN, Kim CS, Choi KC. Corrosive esophageal stricture: safety and effectiveness of balloon dilation. Radiology. 1992. 184:373–378.
3. Park JY, Shin JY, Yang HR, Ko JS, Kim WS, Seo JK. Usefulness of early endoscopy for predicting the development of stricture after corrosive esophagitis in children. Korean J Pediatr. 2009. 52:446–452.
4. Hamza AF, Abdelhay S, Sherif H, Hasan T, Soliman H, Kabesh A, et al. Caustic esophageal strictures in children: 30 years' experience. J Pediatr Surg. 2003. 38:828–833.
5. Weintraub JL, Eubig J. Balloon catheter dilatation of benign esophageal strictures in children. J Vasc Interv Radiol. 2006. 17:831–835.
6. London RL, Trotman BW, DiMarino AJ Jr, Oleaga JA, Freiman DB, Ring EJ, et al. Dilatation of severe esophageal strictures by an inflatable balloon catheter. Gastroenterology. 1981. 80:173–175.
7. Goldthorn JF, Ball WS Jr, Wilkinson LG, Seigel RS, Kosloske AM. Esophageal strictures in children: treatment by serial balloon catheter dilatation. Radiology. 1984. 153:655–658.
8. Sato Y, Frey EE, Smith WL, Pringle KC, Soper RT, Franken EA Jr. Balloon dilatation of esophageal stenosis in children. AJR Am J Roentgenol. 1988. 150:639–642.
9. Ko HK, Shin JH, Song HY, Kim YJ, Ko GY, Yoon HK, et al. Balloon dilation of anastomotic strictures secondary to surgical repair of esophageal atresia in a pediatric population: long-term results. J Vasc Interv Radiol. 2006. 17:1327–1333.
10. Lisy J, Hetkova M, Snajdauf J, Vyhnanek M, Tuma S. Long-term outcomes of balloon dilation of esophageal strictures in children. Acad Radiol. 1998. 5:832–835.
11. Fasulakis S, Andronikou S. Balloon dilatation in children for oesophageal strictures other than those due to primary repair of oesophageal atresia, interposition or restrictive fundoplication. Pediatr Radiol. 2003. 33:682–687.
12. Lan LC, Wong KK, Lin SC, Sprigg A, Clarke S, Johnson PR, et al. Endoscopic balloon dilatation of esophageal strictures in infants and children: 17 years' experience and a literature review. J Pediatr Surg. 2003. 38:1712–1715.
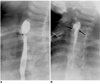
13. Doo EY, Shin JH, Kim JH, Song HY. Oesophageal strictures caused by the ingestion of corrosive agents: effectiveness of balloon dilatation in children. Clin Radiol. 2009. 64:265–271.
14. Kukkady A, Pease PW. Long-term dilatation of caustic strictures of the oesophagus. Pediatr Surg Int. 2002. 18:486–490.
15. Yeming W, Somme S, Chenren S, Huiming J, Ming Z, Liu DC. Balloon catheter dilatation in children with congenital and acquired esophageal anomalies. J Pediatr Surg. 2002. 37:398–402.
16. Yararbai O, Osmanodlu H, Kaplan H, Tokat Y, Coker A, Korkut M, et al. Esophagocoloplasty in the management of postcorrosive strictures of the esophagus. Hepatogastroenterology. 1998. 45:59–64.
17. Ragheb MI, Ramadan AA, Khalia MA. Management of corrosive esophagitis. Surgery. 1976. 79:494–498.
18. Kim JH, Song HY, Kim HC, Shin JH, Kim KR, Park SW, et al. Corrosive esophageal strictures: long-term effectiveness of balloon dilatation in 117 patients. J Vasc Interv Radiol. 2008. 19:736–741.
19. Lovejoy FH Jr. Corrosive injury of the esophagus in children: failure of corticosteroid treatment reemphasizes prevention. N Engl J Med. 1990. 323:668–670.
20. Muhletaler CA, Gerlock AJ Jr, de Soto L, Halter SA. Acid corrosive esophagitis: radiographic findings. AJR Am J Roentgenol. 1980. 134:1137–1140.
21. de Lange EE, Shaffer HA Jr. Anastomotic strictures of the upper gastrointestinal tract: results of balloon dilation. Radiology. 1988. 167:45–50.
22. McLean GK, Cooper GS, Hartz WH, Burke DR, Meranze SG. Radiologically guided balloon dilation of gastrointestinal strictures. Part I. Technique and factors influencing procedural success. Radiology. 1987. 165:35–40.
23. Kim IO, Yeon KM, Kim WS, Park KW, Kim JH, Han MC. Perforation complicating balloon dilation of esophageal strictures in infants and children. Radiology. 1993. 189:741–744.
24. Maynar M, Guerra C, Reyes R, Mayor J, Garcia J, Facal P, et al. Esophageal strictures: balloon dilation. Radiology. 1988. 167:703–706.
25. Jayakrishnan VK, Wilkinson AG. Treatment of oesophageal strictures in children: a comparison of fluoroscopically guided balloon dilatation with surgical bouginage. Pediatr Radiol. 2001. 31:98–101.
26. Han HY, Song HY, Han YM, Chon SB, Chung GH, Sohn MH, et al. Difficulty of balloon dilatation in corrosive esophageal strictures. J Korean Radiol Soc. 1993. 29:1181–1186. [Korean].
27. Gundogdu HZ, Tanyel FC, Buyukpamukcu N, Hicsonmez A. Conservative treatment of caustic esophageal strictures in children. J Pediatr Surg. 1992. 17:767–770.
28. Wilkinson AG, MacKinlay GA. Use of a cutting balloon in the dilatation of caustic oesophageal stricture. Pediatr Radiol. 2004. 34:414–416.







 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download