INTRODUCTION
Intracranial lipoma is a rare disease entity accounting for about 0.1-0.5% of all intracranial tumors. More than 50% of intracranial lipomas are located in the callosal cisterns (123). Intracranial lipomas are also found in other locations including the quadrigeminal, superior cerebellar, suprasellar, interpeduncular, cerebellopontine angle, and Sylvian cisterns (456). An off-midline location of an intracranial lipoma is uncommon (378). We report an intracranial lipoma with an unusual location in the high parietal convexity along with massive calcification and no underlying arteriovenous malformation or congenital anomaly.
CASE REPORT
A 63-year-old male visited our institute with a chief complaint of an incidentally found intracranial vascular malformation about which he had been informed in a local clinic. He had a history of concussion about 20 years prior, and minor head trauma about 3 months prior. However, he had no referred associated symptoms or signs.
A week before the patient visited our institute, he had a minor headache with dizziness, tinnitus, and facial palsy on the left side. Therefore, he went to see an otolaryngologist at a local clinic. During the examination, he was told that an arteriovenous malformation-like lesion had been found incidentally in the convexity of the right parietal lobe on the brain MRI. He was referred to our institute to check the brain MRI and for further evaluation.
On the MRI performed at our institute, we noted an irregular-shaped mass-like lesion under the dura mater, with high signal intensity on a T1-weighted image (T1WI), and intermediate signal intensity on a T2-weighted image (T2WI), and a fluid attenuated inversion recovery (FLAIR) image. It was differentially diagnosed as a lipomatous mass or subdural hematoma. Below the mass, massive calcification of low signal intensity was evident on all pulse sequences.
Contrast-enhanced T1WI with fat suppression revealed fat-suppressed, heterogeneous intermediate signal intensity of the mass without definite enhancement. There was no evidence of vascular malformation in the brain MRI (Fig. 1).
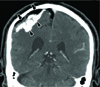
A brain CT was performed after a brain MRI, and revealed a distinct fatty mass overlying the massive calcifications over the convexity of the parietal lobe. Based on the radiologic findings, the lesion could be diagnosed as lipoma with massive calcification (Fig. 2). After conservative treatment for the dizziness, the patient was discharged and scheduled to be followed up.
DISCUSSION
Intracranial lipoma generally occurs in the midline struc ture and subarachnoid cistern (123). It is also sometimes found in the interpeduncular cistern, cerebellopontine angle, Sylvian, and prepontine cistern. The most common type of intracranial lipoma is an interhemispheric lipoma (4).
Yilmaz et al. (9) reported a clinical study about intracranial lipoma in 14 patients, of which the most frequent locations were the quadrigeminal cistern in five cases, the dorsal mesencephalic area in four, pericallosal lipoma in three, and only one case each in the prepontine cistern and the cerebellopontine angle cistern. Britt et al. (10) reported a case of intracranial lipoma in the cerebral cortex and categorized the locations of intracranial lipomas in the previous reports in sites such as the Sylvian fissure and cerebral convexity. Our case belongs to the category involving the right parietal convexity, which is quite a rare location for intracranial lipomas.
The pathogenesis of intracranial lipoma has been explained in two ways: Truwit and Barkovich (7) suggested that it is a consequence of displacement of embryonal mesenchyme during development. In a similar way, a congenital hamartomatous lesion can incorporate mesenchymal cells in the neural tube. On the other hand, Verga (11) proposed an origin in an abnormal dysgenetic process, in which premodial pia mater or mesenchymal cells persist around the brain and generate the intracranial lipoma.
Other combined anomalies have been reported, including agenesis of the corpus callosum, micropolygyria with lipomas over the cerebral cortex, spina bifida, cleft lip, high-arched palate, facial asymmetry, funnel chest, and septal defects of the heart (712). However, our case had no underlying congenital anomaly or vascular malformation, except for focal encephalomalatic changes in the adjacent brain parenchyma.
Lipoma of the corpus callosum is usually accompanied by calcification resembling a chalice or shell at the margin of the tumor. Kazner et al. (2) reported 11 cases of intracranial lipomas, some of which showed the typical features of shell-like calcifications at the edge of the lipoma or small areas of calcification within the lipoma. In our patient, the lower margin of the lipoma along the cerebral cortex contained calcifications. Although at a different location, our case had calcifications at the edge of the lipoma which resembled previous reports of lipomas with calcifications in the corpus callosum.
Intracranial lipomas can be diagnosed from radiologic findings on CT as well as fat-suppressed magnetic resonance (MR) studies, which permit a differential diagnosis to be made. Fat-saturated MR imaging is the key to the differentiation an intracranial lipoma from hemorrhage with high signal intensity on T1-weighted MR images. The high signal intensity due to the paramagnetic effect of a hematoma is not suppressed in fat saturation images, unlike that of an intracranial lipoma (5). There are other fat-containing lesions such as an epidermoid, teratoma, lipomatous meningioma, and so on. Epidermoids and teratomas present as cystic lesions that can contain localized fat components as well as other associated specific components. The fat droplet of a dermoid/epidermoid will spread to the subarachnoid cistern or ventricles if it is ruptured (13). There are some reports of lipomatous meningiomas with signal intensities similar to a lipoma. However, the contrast enhancement and typical attachment to the dura differentiate lipomatous meningioma from a lipoma (14). Although our diagnosis was not surgically confirmed due to benign nature of the lipoma, it could be radiologically diagnosed on CT and MR scans on the basis of its CT Hounsfield number, T1 shortening, and by means of the fat saturation technique. It was accompanied by massive calcification under the lipoma mass, with low signal intensity on T1- and T2-weighted MR images and high density on CT scan. A follow-up of the patient is planned.
We report an intracranial convexity lipoma combined with massive calcification in the unusual location of high parietal convexity.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download