Abstract
Objective
Using a pulsating coronary artery phantom at high heart rate settings, we investigated the efficacy of a motion correction algorithm (MCA) to improve the image quality in dual-energy spectral coronary CT angiography (CCTA).
Materials and Methods
Coronary flow phantoms were scanned at heart rates of 60–100 beats/min at 10-beats/min increments, using dual-energy spectral CT mode. Virtual monochromatic images were reconstructed from 50 to 90 keV at 10-keV increments. Two blinded observers assessed image quality using a 4-point Likert Scale (1 = non-diagnostic, 4 = excellent) and the fraction of interpretable segments using MCA versus conventional algorithm (CA). Comparison of variables was performed with the Wilcoxon rank sum test and McNemar test.
Results
At heart rates of 70, 80, 90, and 100 beats/min, images with MCA were rated as higher image scores compared to those with CA on monochromatic levels of 50, 60, and 70 keV (each p < 0.05). Meanwhile, at a heart rate of 90 beats/min, image interpretability was improved by MCA at a monochromatic level of 60 keV (p < 0.05) and 70 keV (p < 0.05). At a heart rate of 100 beats/min, image interpretability was improved by MCA at monochromatic levels of 50 keV (from 69.4% to 86.1%, p < 0.05), 60 keV (from 55.6% to 83.3%, p < 0.05) and 70 keV (from 33.3% to 69.3%, p < 0.05).
Coronary CT angiography (CCTA) is widely used in populations with low to middle risk of coronary artery disease as a non-invasive method to rule out coronary artery disease, due to its high diagnostic accuracy and low invasiveness (1). At present, CCTA still has the following limitations: certain images cannot be evaluated with motion artifacts due to limited temporal resolution (2); and CCTA with retrospective electrocardiography (ECG)-gating leads to a high radiation dose, while the prospective ECG-gating technique is limited to the patients with a heart rate of less than 65 beats per minute (bpm) (3).
Recently, a novel intra-cycle motion compensation algorithm (MCA) was developed, able to define the precise vessel location using the adjacent cardiac phase information and correct partial coronary motion (4). Preliminary study results have confirmed that MCA can improve image quality and image interpretability in CCTA, under both prospective and retrospective ECG gating modes (56). At high heart rates, using retrospective ECG gating mode still result in a relatively high radiation dose. Dual-energy spectral coronary CT with a rapid kVp-switching technique can generate a 40–140 keV monochromatic image, a promising prospective ECG-triggered CCTA imaging technique for the assessment of both coronary artery and myocardial perfusion (789). Initial investigation suggests that monochromatic image scans eliminate beam-hardening artifacts with a reduction in radiation dose (2), but this was limited to patients with low heart rates. Accordingly, we sought to explore the possibility of using coronary CT spectral imaging with MCA at different monochromatic levels, using a coronary flow phantom to expand the application of spectral imaging with a prospective ECG-gating technique in patients with higher heart rates.
A quantitative pulsating coronary phantom (Mocomo, Fuyo Corporation, Tokyo, Japan) was adopted (Fig. 1) to simulate different heart rates. A silica gel ball with a cavity was used to simulate myocardium. The cavity was filled with diluted iodine contrast (Omnipaque 350 mg I/mL; Nycomed, Princeton, NJ, USA) of about 300 Hounsfield unit under 120 kVp. Silica gel tubes of 0.5 mm to 1.0 mm thickness were attached to the surface of the ball to simulate the coronary artery tree with an inner diameter from 0.5 mm to 6.0 mm. The tubes were filled with diluted iodine contrast (Omnipaque 350 mg I/mL; Nycomed) of about 550 HU under 120 kVp (Fig. 1).
The phantom model was scanned on a single-source dual-energy CT scanner (Discovery CT 750HD; GE Healthcare, Milwaukee, WI, USA). A prospective ECG-triggered acquisition was performed using an 80-millisecond padding centered at 75% of the cardiac cycle. Other scan parameters were: a tube voltage of fast-kVp (80 kVp/140 kVp) switching, tube current of 600 mA, a gantry rotation time of 0.35 second, a slice thickness of 0.625 mm, and a detector collimation of 64 × 0.625 mm. The phantom was scanned with five simulated heart rates (60–100 beats/minutes with a 10 bpm increment).
Under each simulated heart rate, five monochromatic image sets (50–90 keV at 10 keV increments) were reconstructed at a 75% R-R interval. The reconstructed images were sent to a dedicated workstation (Advantage Workstation 4.6, GE Healthcare, Milwaukee, WI, USA). Both conventional algorithm (CA) and MCA techniques were applied to each image set. Blinded to image groups, two experienced independent radiologists interpreted images, and a third interpreted any images with an inconsistent diagnosis to give the final diagnosis decision. Image evaluation was performed at a fixed window width of 800 HU and a window level of 100 HU.
In accordance with the definition of coronary segments, as defined by the New York Heart Association (NYHA) (10), the proximal, middle and distal parts of 12 segments of the model coronary artery, with a total of 36 parts, were evaluated. The image quality of the model coronary segments was scored using a 4-point Likert Scale, specifically: 1) poor image quality, coronary artery could not be evaluated because of serious motion artifacts or insufficient contrast; 2) acceptable image quality, the image quality was decreased due to motion artifacts or low enhancement attenuation; 3) good image quality with slight motion artifacts or low contrast; and 4) excellent image quality without motion artifacts, and a clear vascular wall outline was visible. Image interpretability was defined as the percentage of vascular segments scored as 2, 3, and 4 points from the total number of vascular segments.
SPSS 17.0 (SPSS Inc., Chicago, IL, USA) statistical software package was used for statistical analyses. Continuous variables were expressed as the mean and 95% confidence interval (CI), and the numeration data were presented as percentages. The image scores of CA and MCA under the same heart rate, but on different keV levels, were compared in terms of their pairwise signed rank sum test (Wilcoxon test), while image interpretability of CA and MCA were compared using a χ2 test (McNemar test). Significance level (α) was set as 0.05, and p > α was not statistically
significant.
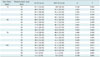
On monochromatic images of 70 keV, image scores of both CA and MCA decreased with an increase in heart rate. CA image scores at different heart rates was 2.9 (95% CI: 2.7–3.1), 2.6 (95% CI: 2.3–2.9), 2.3 (95% CI: 2.0–2.6), 1.6 (95% CI: 1.3–1.9), and 1.4 (95% CI: 1.2–1.6), corresponding to 60, 70, 80, 90, and 100 bpm, respectively. The image interpretability at heart rates of 70 bpm and above was lower than 90% (Table 1). The image score of MCA at different heart rates was 3.1 (95% CI: 2.9–3.2), 2.9 (95% CI: 2.6–3.1), 2.6 (95% CI: 2.4–2.9), 2.3 (95% CI: 2.0–2.6), and 2.0 (95% CI: 1.7–2.3) corresponding to 60, 70, 80, 90, and 100 bpm, respectively. The image interpretability of MCA was improved at heart rates of 90 and 100 bpm; however, the image interpretability at heart rates of 80 bpm and above remained lower than 90% (Table 1).
At heart rates of 70–100 bpm, MCA had higher image scores of 50, 60, and 70 keV images compared with CA, and the differences were statistically significant (p < 0.05). However, no statistically significant differences were observed between MCA and CA on the 80 and 90 keV images (p > 0.05) (Fig. 2). In particular, at a heart rate of 90 bpm, MCA increased the maximum image score of the 50 keV image from 2.2 (95% CI: 1.9–2.5) to 3.0 (95% CI: 2.7–3.3). At a heart rate of 100 bpm, MCA increased the score of the 50 keV image from 1.9 (95% CI: 1.6–2.1) to 2.8 (95% CI: 2.5–3.1) (Fig. 3).
At a heart rate of 90 bpm, MCA improved image interpretability of 60 and 70 keV images (both p < 0.05); MCA at 50 keV had the highest image interpretability of 88.9%. At a heart rate of 100 bpm, MCA also improved image interpretability of the 50, 60, and 70 keV images (each p < 0.05); MCA at 50 keV had the highest image interpretability of 97.1%. At other heart rates, there was no statistical difference observed in image interpretability between CA and MCA at each monochromatic level (each p > 0.05) (Table 2).
Our study confirms that, with the cardiac phantom in spectral coronary CT imaging, MCA increased the image score at heart rates of 70–100 bpm of low keV level images, and also improved image interpretability at heart rates of 90 and 100 bpm on low keV level images.
Coronary motion artifacts are a factor restricting CCTA image quality. At present, the majority of multi-detector CTs may generate motion artifacts due to limited temporal resolution. Patients with high heart rate have shortened cardiac end-systole and middle-diastole, and as such motion artifacts are more readily generated. As such, beta-receptor blockers are often used to lower heart rate prior to CCTA. However, the use of beta-receptor blocker is contraindicated in some patients, meaning that heart rate cannot be controlled within the ideal range (11).
To date, several methods have been developed to reduce the impact of motion artifacts in CCTA. Hardware-based methods include the use of dual-source CT and increasing the detector width; the method based on the adjustment of scan parameters increases gantry rotation speed, and the software-based method uses a multi-sector reconstruction technique. These technical methods partially reduce motion artifacts, but motion artifacts in CCTA remain present, due to scanner or software limitations (12).
MCA is a novel coronary motion artifact correction technique, which is used to accurately record the motion pathway and speed of the coronary artery. It is also used to trace the motion trail of the coronary artery by analyzing the data of 3 phases, including the target phase plus 80 ms padding in a cardiac cycle, thus improving the localization accuracy of the coronary artery in the target phase and compensating for the motion in this phase, so effectively compressing the reconstruction time window (12). In contrast to conventional multi-sector reconstruction techniques, the MCA method improves the temporal resolution of images by utilizing the data from the same cardiac cycle (12). As such, the correction of motion artifacts by MCA is minimally influenced by heart rate changes seen across different cardiac cycles, and MCA can be applied in the prospective ECG-gating with a lower radiation dose than that used in multi-sector reconstruction (13).
Li et al. (13) compared image interpretability of MCA versus sector reconstruction in patients with moderate heart rates and found that MCA improved image interpretability at both the patient and vessel level, whilst also increasing image interpretability of some coronary segments. Using coronary phantom, Cho et al. (12) studied the correction effects of MCA on coronary motion artifacts, combined with a retrospective ECG-gating technique at different heart rates. At a heart rate of 80–100 bpm, MCA improved image interpretability, image score and diagnostic accuracy, indicating MCA has a larger significant correction effect at high heart rates. A clinical study conducted by Lee et al. (14) also confirmed that patients with high heart rates benefited more from MCA. Fuchs et al. (15) expanded the heart rate applicable range of CCTA in prospective ECG-gating by the application of MCA in prospective ECG-triggered CCTA.
Preliminary study results have confirmed that in retrospective and prospective ECG-gating CCTA, MCA can correct coronary motion artifacts and thus improve image interpretability and diagnostic efficiency of CCTA. However, the use of the application of MCA in spectral CT imaging and its effect on motion artifacts at different monochromatic levels remains to be elucidated. With the cardiac phantom, our study has confirmed that in spectral CT imaging, MCA increases image score at heart rates of 70–100 bpm of low keV levels, and also improved image interpretability at heart rates of 90 and 100 bpm of low keV levels. Innovatively, the phantom was scanned with set heart rates (60–100 bpm with a 10 bpm increment). Compared with previous studies, this study is particularly valuable, as we have shown more clearly the relationship between heart rate and MCA efficacy. Our study confirms the feasibility of applying MCA in spectral CT imaging and the effects of MCA in improving CCTA image quality at low keV levels. At low monochromatic levels (50–70 keV), coronary arteries had higher attenuation and better contrast than in high keV images, and could be characterized by MCA more easily and precisely. At high monochromatic levels (80–90 keV), coronary arteries had lower attenuation and poor contrast, and as such MCA did not improve the image quality score of these images.
This study has the following limitations: firstly, pulsating heart phantom was used in the present study to realize the application of spectral imaging combined with MCA in CCTA at high heart rates, and there was a difference between the simulated heart beats or environment in pulsating heart phantom and the human body. As such the results need to be further confirmed in in vivo study. Secondly, poor image quality can be due to poor enhancement or from a severe motion artifact. This study solely evaluated motion artifacts. However, contrast-to-noise ratio or contrast grade should also be considered in further study. Thirdly, diagnostic accuracy of spectral imaging combined with MCA in CCTA was not evaluated in comparison with that of CA.
Our study of the pulsating coronary artery phantom suggests that image quality degrades with an increase in heart rate on 70 keV spectral CT images, and fails to meet the diagnostic demand when the heart rate is ≥ 70 bpm. MCA could be applied in spectral CCTAs at different monochromatic levels. High simulated heart rate (≥ 70 bpm) and low monochromatic levels (50, 60, and 70 keV) increased image quality score. heart rates of 90 and 100 bpm and low keV levels (≤ 70 keV), combined with MCA, allowed for additional improvements in image interpretability.
Figures and Tables
Fig. 1
Pulsating coronary artery phantom and segmentations of vessels.
A. Pulsating coronary artery phantom. B. Volume rending images demonstrate segmentations of vessels.

Fig. 2
Comparison of image score and 95% confidence interval (CI) between MCA and CA at heart rates of 70, 80, 90, and 100 bpm, at different monochromatic levels.
A. Comparison of image quality score (95% CI) between MCA and CA at heart rate of 70 bpm. B. Comparison of image quality score (95% CI) between MCA and CA at heart rate of 80 bpm. C. Comparison of image quality score (95% CI) between MCA and CA at heart rate of 90 bpm. D. Comparison of image quality score (95% CI) between MCA and CA at heart rate of 100 bpm. *0.05, †p < 0.01. bpm = beats/minute, CA = conventional algorithm, MCA = motion correction algorithm

Fig. 3
Comparison of phantom axial images after CA and MCA at different keV levels at heart rate of 90 bpm.

Table 1
Comparison of Image Interpretability and Image Score between CA and MCA at Monochromatic Images of 70 keV

Table 2
Comparision of Image Interpretability between CA and MCA at Different Heart Rates and on Different Monochromatic Levels
Acknowledgments
The authors would like to thank Dr. Munekuni Sato for providing the silicone models of branching coronary vessels.
References
1. Chang SM, Bhatti S, Nabi F. Coronary computed tomography angiography. Curr Opin Cardiol. 2011; 26:392–402.
2. Taylor CM, Blum A, Abbara S. Patient preparation and scanning techniques. Radiol Clin North Am. 2010; 48:675–686.
3. Hausleiter J, Meyer TS, Martuscelli E, Spagnolo P, Yamamoto H, Carrascosa P, et al. Image quality and radiation exposure with prospectively ECG-triggered axial scanning for coronary CT angiography: the multicenter, multivendor, randomized PROTECTION-III study. JACC Cardiovasc Imaging. 2012; 5:484–493.
4. Min JK, Arsanjani R, Kurabayashi S, Andreini D, Pontone G, Choi BW, et al. Rationale and design of the ViCTORY (Validation of an Intracycle CT Motion CORrection Algorithm for Diagnostic AccuracY) trial. J Cardiovasc Comput Tomogr. 2013; 7:200–206.
5. Leipsic J, Labounty TM, Hague CJ, Mancini GB, O’Brien JM, Wood DA, et al. Effect of a novel vendor-specific motion-correction algorithm on image quality and diagnostic accuracy in persons undergoing coronary CT angiography without rate-control medications. J Cardiovasc Comput Tomogr. 2012; 6:164–171.
6. Carrascosa P, Deviggiano A, Capunay C, De Zan MC, Goldsmit A, Rodriguez-Granillo GA. Effect of intracycle motion correction algorithm on image quality and diagnostic performance of computed tomography coronary angiography in patients with suspected coronary artery disease. Acad Radiol. 2015; 22:81–86.
7. Fuchs TA, Stehli J, Fiechter M, Dougoud S, Gebhard C, Ghadri JR, et al. First experience with monochromatic coronary computed tomography angiography from a 64-slice CT scanner with Gemstone Spectral Imaging (GSI). J Cardiovasc Comput Tomogr. 2013; 7:25–31.
8. Scheske JA, O’Brien JM, Earls JP, Min JK, LaBounty TM, Cury RC, et al. Coronary artery imaging with single-source rapid kilovolt peak-switching dual-energy CT. Radiology. 2013; 268:702–709.
9. So A, Hsieh J, Imai Y, Narayanan S, Kramer J, Procknow K, et al. Prospectively ECG-triggered rapid kV-switching dual-energy CT for quantitative imaging of myocardial perfusion. JACC Cardiovasc Imaging. 2012; 5:829–836.
10. Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975; 51:Suppl 4. 5–40.
11. Sabarudin A, Sun Z. Beta-blocker administration protocol for prospectively ECG-triggered coronary CT angiography. World J Cardiol. 2013; 5:453–458.
12. Cho I, Elmore K, Ó Hartaigh B, Schulman-Marcus J, Granser H, Valenti V, et al. Heart-rate dependent improvement in image quality and diagnostic accuracy of coronary computed tomographic angiography by novel intracycle motion correction algorithm. Clin Imaging. 2015; 39:421–426.
13. Li Q, Li P, Su Z, Yao X, Wang Y, Wang C, et al. Effect of a novel motion correction algorithm (SSF) on the image quality of coronary CTA with intermediate heart rates: segment-based and vessel-based analyses. Eur J Radiol. 2014; 83:2024–2032.
14. Lee H, Kim JA, Lee JS, Suh J, Paik SH, Park JS. Impact of a vendor-specific motion-correction algorithm on image quality, interpretability, and diagnostic performance of daily routine coronary CT angiography: influence of heart rate on the effect of motion-correction. Int J Cardiovasc Imaging. 2014; 30:1603–1612.
15. Fuchs TA, Stehli J, Dougoud S, Fiechter M, Sah BR, Buechel RR, et al. Impact of a new motion-correction algorithm on image quality of low-dose coronary CT angiography in patients with insufficient heart rate control. Acad Radiol. 2014; 21:312–317.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download