Abstract
Objective
To evaluate the association between alpha angle and herniation pit on MRI in asymptomatic hip joints and their associations with demographic variables.
Materials and Methods
Hip MRI of 185 asymptomatic hip joints of 105 adults (age 18 to 80 years) from September 2011 through December 2012 were retrospectively studied. Alpha angles were measured on oblique axial MR images by 2 observers. Herniation pit was determined by 1 observer. Size measures, prevalence, and statistical analyses were conducted regarding its association with age, gender, laterality (right or left hip). Intra- and inter-observer agreements were determined by intra-class correlation coefficient.
Results
The prevalence of herniation pit in asymptomatic hips was 21.6%. The range of alpha angle was 27.6-65.0 degrees. Seventeen and 16 out of 185 (9.1% and 8.6%) hip joints showed alpha angle of ≥ 55 degrees in first and second measurement sessions, respectively. There was no association between alpha angle ≥ 55 and presence of herniation pit. There was no association between alpha angle ≥ 55 and the size of herniation pit. Inter-observer agreement of alpha angle was 0.485 between first measurements of first vs. second observer, respectively. Intra-observer agreement of alpha angle was 0.654, respectively. Forty (21.6%) of 185 hip joints (35 of 105 patients, 33.3%) had herniation pit, with no difference according to age, gender, or laterality of hip joint.
Femoroacetabular impingement (FAI) has recently gained much attention as a cause of hip pain and restriction of hip motion in young adults, and especially as a possible cause of osteoarthritis (OA) in young adults (123456). It is thought that FAI occurs when there is a conflict between the proximal femur and acetabular rim (1). The prevalence of FAI on clinical diagnosis ranges from 6-35% in the general population (17). There are 3 types of FAI, i.e., pincer-, cam-, and combined type with reported prevalence of 16.6-57.0%, 10.2-35.0%, and 3.7-14.0%, respectively (89). In pincer-type FAI, acetabular over-coverage leads to conflict between femoral head-neck junction and acetabular rim (10) resulting in impingement, pain and limited range of motion. In cam-type FAI, the normal waist at femoral head-neck junction is decreased resulting in aspheric morphology in the femoral head-neck junction (10). This also leads to impingement and symptoms of FAI. The contour of the femoral head-neck junction may be quantified with alpha angle (11121314), and is generally considered as abnormal finding when alpha angle is ≥ 55 degrees (1516). It is believed as a useful method to diagnose cam-type FAI, because previous studies have shown that there is a significant association between increased alpha angle and presence of cam-type FAI (11). But other studies suggested that alpha angle shows considerable variability and there is no significant association between increased alpha angle and presence of cam-type FAI when evaluated on MR arthrography (17).
Herniation pit was once thought as a normal variant; it is formed by herniation of soft tissue through erosion or perforation at the reactive interface area in the femoral neck (18). In the current literature, it has been mentioned in context with FAI (19202122). Panzer et al. (19) reported that alpha angle was significantly larger in patients with herniation pit and there was no correlation between radiographic indicators of pincer-type FAI and the presence of herniation pit on computed tomography. Another study suggested that presence of herniation pits has little relevance to FAI (23), so it remains controversial whether herniation pit may serve as a reliable radiographic predictor of FAI. The association between herniation pit and increased alpha angle has not been studied on MRI.
Therefore, the purpose of this study was to evaluate alpha angle, a possible radiologic indicator of cam-type FAI, and herniation pit on MRI in asymptomatic hip joints; and to analyze their associations with demographic variables and each other.
The Institutional Review Board approved this retrospective study and waived informed consent. Two hundred and forty-eight hip joints of 124 adults (age from 18 to 80 years), who underwent hip MRI due to trauma or unilateral pelvic symptoms from September 2011 through December 2012 were retrospectively studied. Electronic medical records and MR images were reviewed to exclude hip joints with symptoms or abnormal imaging findings. Among the 248 hips of 124 patients, we excluded 19, which were diagnosed clinically as FAI or whose alpha angle was not measurable due to avascular necrosis (AVN) or definite osteophytes or OA or history of bilateral hip surgery. Among residual 210 hips of 105 patients, we additionally excluded 13 right and 12 left hips, in which alpha angles were not measurable due to unilateral hip surgery, AVN, fracture and malignancy. As a result, 185 hips (91 right and 94 left hips) of 105 patients (44 male and 61 female; mean age, 54.3 years; age range, 18-80 years) were analyzed in our study.
Hip MRI was performed using a 1.5T scanner (Gyroscan Intera; Philips, Best, the Netherlands) with SENSE-body coil (Philips, Best, the Netherlands) and a 3T scanner (Achieva; Philips, Best, the Netherlands) with SENSE-XL-Torso coil (Philips, Best, the Netherlands), with the patients in supine position. Sequence, scan plane, repetition time, echo time, slice thickness, and field of view were shown in Table 1. Oblique axial images were obtained by positioning a box in the femoral neck on coronal image and oblique axial slices were obtained parallel to femoral neck.
Alpha angles were measured on oblique axial T2-weighted MR images twice by first observer (resident, 3 years of experience) after a 2-week interval. Alpha angles were also measured once by second observer (musculoskeletal radiology fellow, 4 years of experience). The results obtained by the second observer were used only when calculating inter-observer agreement of measuring alpha angle. Each observer chose his/her own image for measurement using measurement methods described previously (Fig. 1) (19).
Presence of herniation pit was subjectively assessed and size of herniation pit was measured on axial, coronal and oblique axial MR images only by first observer, using the typical radiologic finding of focal fibrocystic lesion in femoral head and neck of > 2 mm in diameter with low signal intensity (SI) on T1-weighted image and intermediate to high SI on T2-weighted image (Fig. 2). The size of herniation pit was defined as the longest diameter between measured value from axial, coronal and oblique axial images. Herniation pits were divided into 2 groups; herniation pits larger than mean value (> 5.2 mm) and smaller than mean value (< 5.2 mm). Before assessment, the first observer underwent a consensus training session with a musculoskeletal staff radiologist (12 years of experience) for proper diagnosis of herniation pit. The radiologist was blinded to the alpha angles when evaluating herniation pit. Ten ambiguous cases from first observer were rechecked by being assessed under consensus with the musculoskeletal staff radiologist (12 years of experience).
Statistical analysis was performed using dedicated statistical software (SPSS 12.0, SPSS Inc., Chicago, IL, USA). The prevalence of alpha angle ≥ 55 degrees and herniation pit was calculated (first and second measurement by first observer) and statistical analysis was done regarding their association with age, gender, laterality of hip (right or left). Prevalence was calculated by frequency analysis. Inter-observer agreement of alpha angle was determined by reliability analysis using intra-class correlation coefficient; between first analysis by first observer and analysis by second observer. Intra-observer agreement of alpha angle was determined by Pearson chi-square contingency test; between first and second analysis by first observer. The association between alpha angle ≥ 55 degrees and the presence of herniation pit was analyzed using Pearson chi-square analysis. The association between alpha angle ≥ 55 degrees and the size of herniation pit (larger than 5.2 mm vs. smaller than 5.2 mm) was analyzed using Pearson chi-square analysis. The association between alpha angle ≥ 55 degrees and the actual size of herniation pit was also analyzed using generalized linear models. The correlation between alpha angle ≥ 55 degrees and several variables (age, gender, and laterality of hip) was analyzed using Pearson chi-square analysis and generalized linear models. Likewise, the association between presence of herniation pit and various demographic variables (age, gender, and laterality of hip) was analyzed using Pearson chi-square analysis and generalized linear models.
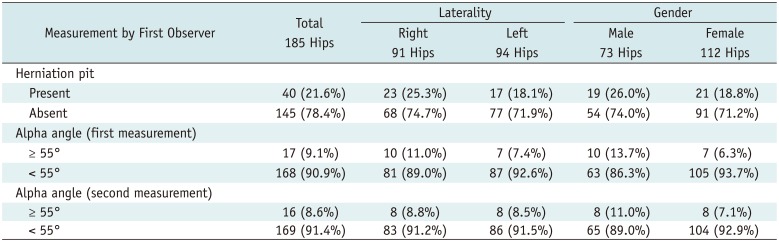
Forty out of 185 asymptomatic hips were found to have herniation pits; 35 out of 105 patients were found to have herniation pits. The prevalence of herniation pits was 21.6% (40 in a total of 185 hips, 25.3% at right and 18.1% at left hips) (Table 2). The range of size of herniation pit was 2-12 mm, with mean 5.2 ± 2.1 mm. Twenty-six of herniation pits were < 5.2 mm and 14 of them were ≥ 5.2 mm. Correlation analyses between herniation pit and several variables (gender and laterality of hip) indicated that there was no significant correlation between the presence of herniation pit and these variables (p = 0.160, p = 0.157). Herniation pits were most common in patients in their 60's (11 out of total 35 herniation pits, 45.8%) and there was no significant association between the presence of herniation pit and age (p = 0.110).
The range of alpha angle was 27.6-65.0 degrees with mean 41.8 ± 6.2 and 42.0 ± 5.5 degrees in 185 hips of 105 asymptomatic patients in first and second measurement sessions, respectively. Seventeen and 16 out of 185 hips had alpha angle ≥ 55 degrees in first and second measurement sessions, respectively, resulting in a prevalence of 9.1 and 8.6%, respectively (Table 2). Correlation analyses between alpha angle ≥ 55 degrees and several variables (age, gender, and laterality of hip) indicated that there was no significant correlation between increased alpha angle and those variables (p = 0.483-0.386, p = 0.171-0.657, p = 0.298-0.488) (Table 2).
Using the Pearson's chi-square contingency test, there was no significant association between alpha angle ≥ 55 degrees and the presence of herniation pit (p = 0.205-0.521). Using the Pearson's chi-square contingency test, there was no significant association between alpha angle ≥ 55 degrees and the size of herniation pit > 5.2 mm (p = 0.350-0.583). Using generalized linear model, there was no significant association between alpha angle ≥ 55 degrees and the actual size of herniation pit (p = 0.212-0.560).
The inter-observer agreement of alpha angle was 0.485 between the first measurements of first and second observers. The intra-observer agreement of alpha angle was 0.654 between the first and second measurements of first observer.
In a prior study by Pitt et al. (18) using radiographic imaging, the prevalence of herniation pits in normal adults was approximately 5%. Nokes et al. (24) reported a prevalence of 4% (5 of 120 patients) in anteroposterior radiographs and MRI. In our study, the prevalence of herniation pit in asymptomatic hips was 21.6% of total 185 hips, which was similar to results from recent studies (26.7%, 107 of 400 hips) (19), and higher than those in other previous studies (1824). With the wide application and improved resolution of CT and MRI of the hips, herniation pits of the femoral neck are increasingly identified (25). Probably due to the higher resolution and tissue contrast, our study showed a higher prevalence of herniation pit in asymptomatic patients than in previous studies.
Recently, it is reported that FAI may be a cause of herniation pit (1920212223). Ganz et al. (1) and Leunig et al. (21) suggested that herniation pit might be indicative of impingement. Leunig et al. (21) found a 33% prevalence of herniation pits in hips with FAI, which was expressed in terms of juxtaarticular fibrocysts. Kassarjian et al. (26) reported the prevalence of herniation pits as 4.8% (2 of 42 hips) in a patient collective with cam-type FAI. The result of our study showed similar or even higher prevalence of herniation pits in asymptomatic patients than those reported in FAI, as compared to previous studies. This confirmed that herniation pit might not be associated with FAI.
Our study showed a wide range of alpha angles (27.6-65.0 degrees) with mean of 41.8 ± 6.2 and 42.0 ± 5.5 degrees in asymptomatic patients. In previous literature of asymptomatic patients, alpha angle showed a wide range (32-57 degrees) and similar mean (45 degrees) to our study (27). In our study, the prevalence of alpha angle ≥ 55 degrees in asymptomatic patients was 8.1% and 11.9% in the first and second measurement sessions, respectively. Thus, interpretation of increased alpha angle with suggested particular cut-off values, such as 50 or 55 degrees, as FAI needs caution and comprehensive consideration with accompanying radiologic and clinical findings. This is in concordance with a previously published commentary (24).
Several prior studies showed that cam-type deformities were more common in male, whereas pincer-type deformities were more common in female (12829). Another study suggested that pincer deformities were frequent in both male and female (8). In our study, there was no association between gender and alpha angle, which may be a radiographic indicator of cam-type FAI.
In our study, there was no association between increased alpha angle and presence of herniation pit; there was no significant difference between the prevalence of herniation pit in the 2 groups with alpha angle ≥ vs. < 55 degrees, which was different from results of previous literature; in a study by Panzer et al. (19), alpha angles were significantly larger in the group of patients with herniation pits than in the group without herniation pits. Our study suggested that herniation pit might not be associated with either increased alpha angle or presence of FAI. This was consistent with the results of a previous report of low association of positive radiographic signs related to FAI among patients with herniation pit, suggesting that herniation pit has limited significance in the diagnosis of FAI (23).
The inter-observer agreement of alpha angle (0.485) was moderate and intra-observer agreement (0.654) was good, suggesting that alpha angle on oblique axial MR images can have substantial inter-observer variation.
There were some limitations in our study. First, our study was a retrospective single-center study in a tertiary teaching hospital, so the size of study population was relatively small and there may have been a selection bias in the patient population. However, it is difficult to obtain MR imaging in completely normal, asymptomatic patients in a usual clinical setting. Second, although we included the presumed normal/asymptomatic hip for analysis after carefully excluding hips indicated to have symptoms in medical records review, we cannot ascertain that these were truly asymptomatic. Third, we conducted observational review in patients without symptoms, so we do not have any comparable control group. Fourth, we assessed the association between herniation pit and alpha angle that are known relevant features of cam type FAI; and we did not consider the other features, such as acetabular deformity or lateral center edge angle, known to be associated with pincer type FAI. Fifth, some elderly patients may have possible femoral head deformity due to OA, which can affect alpha angle. We included asymptomatic patients between ages of 18 to 80 years and did not exclude elderly patients because not all elderly patients have OA with significant femoral head deformity. Last, we did not evaluate the presence and association with other findings associated with FAI, such as center edge angle, femoral offset, cartilage loss or labral tear. However, our study was the first study to evaluate the relationship between increased alpha angle and herniation pit and demographic variables using MR images in a large number of asymptomatic hips.
In summary, the prevalence of herniation pit in asymptomatic patients was 21.6% in 185 hips, which was similar or higher than those reported in studies of FAI patients. There was no significant association between increased alpha angle and presence of herniation pit; their association in patients with FAI may be just incidental. Alpha angle showed a wide range in asymptomatic patients and substantial inter-observer variation. In conclusion, the presence of herniation pit and increased alpha angle need to be interpreted with caution, as both are common in asymptomatic hips without significant association with each other.
Acknowledgments
Presented at ECR 2013 as a scientific paper; study materials obtained at previous affiliation of corresponding author, namely, Seoul National University Bundang Hospital. The authors would like to thank Sungehn Jo, MD and Soyeon Ahn, PhD for help in data and statistical analysis, respectively.
References
1. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003; (417):112–120. PMID: 14646708.
2. Jäger M, Wild A, Westhoff B, Krauspe R. Femoroacetabular impingement caused by a femoral osseous head-neck bump deformity: clinical, radiological, and experimental results. J Orthop Sci. 2004; 9:256–263. PMID: 15168180.

3. Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004; (429):178–181. PMID: 15577484.
4. Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007; 188:1540–1552. PMID: 17515374.

5. Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004; (429):170–177. PMID: 15577483.
6. Palmer WE. Femoroacetabular impingement: caution is warranted in making imaging-based assumptions and diagnoses. Radiology. 2010; 257:4–7. PMID: 20851933.

7. Fukushima K, Uchiyama K, Takahira N, Moriya M, Yamamoto T, Itoman M, et al. Prevalence of radiographic findings of femoroacetabular impingement in the Japanese population. J Orthop Surg Res. 2014; 9:25. PMID: 24725368.

8. Laborie LB, Lehmann TG, Engesæter IØ, Eastwood DM, Engesæter LB, Rosendahl K. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology. 2011; 260:494–502. PMID: 21613440.

9. Nardo L, Parimi N, Liu F, Lee S, Jungmann PM, Nevitt MC, et al. Femoroacetabular Impingement: Prevalent and Often Asymptomatic in Older Men: The Osteoporotic Fractures in Men Study. Clin Orthop Relat Res. 2015; 473:2578–2586. PMID: 25736918.

10. Standaert CJ, Manner PA, Herring SA. Expert opinion and controversies in musculoskeletal and sports medicine: femoroacetabular impingement. Arch Phys Med Rehabil. 2008; 89:890–893. PMID: 18452737.

11. Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006; 240:778–785. PMID: 16857978.

12. Pfirrmann CW, Duc SR, Zanetti M, Dora C, Hodler J. MR arthrography of acetabular cartilage delamination in femoroacetabular cam impingement. Radiology. 2008; 249:236–241. PMID: 18682585.
13. Kassarjian A, Cerezal L, Llopis E. [MR arthrography of the hip with emphasis on femoroacetabular impingement]. Radiologia. 2009; 51:17–29. quiz 119PMID: 19303477.
14. Anderson SE, Siebenrock KA, Tannast M. Femoroacetabular impingement. Eur J Radiol. 2012; 81:3740–3744. PMID: 21924849.

15. Beaulé PE, Zaragoza E, Motamedi K, Copelan N, Dorey FJ. Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res. 2005; 23:1286–1292. PMID: 15921872.

16. Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002; 84:556–560. PMID: 12043778.

17. Lohan DG, Seeger LL, Motamedi K, Hame S, Sayre J. Cam-type femoral-acetabular impingement: is the alpha angle the best MR arthrography has to offer? Skeletal Radiol. 2009; 38:855–862. PMID: 19565238.

18. Pitt MJ, Graham AR, Shipman JH, Birkby W. Herniation pit of the femoral neck. AJR Am J Roentgenol. 1982; 138:1115–1121. PMID: 6979213.

19. Panzer S, Augat P, Esch U. CT assessment of herniation pits: prevalence, characteristics, and potential association with morphological predictors of femoroacetabular impingement. Eur Radiol. 2008; 18:1869–1875. PMID: 18389244.

20. Guo Z, Xu L, Su YB, Cheng XG. Correlation between the prevalence of herniation pits and the α angle of the hip: computed tomography evaluation in healthy Chinese adults. BMC Musculoskelet Disord. 2013; 14:288. PMID: 24106774.

21. Leunig M, Beck M, Kalhor M, Kim YJ, Werlen S, Ganz R. Fibrocystic changes at anterosuperior femoral neck: prevalence in hips with femoroacetabular impingement. Radiology. 2005; 236:237–246. PMID: 15987977.

22. Panzer S, Augat P, Scheidler J. [Herniation pits and their renaissance in association with femoroacetabular impingement]. Rofo. 2010; 182:565–572. PMID: 20449791.
23. Kim JA, Park JS, Jin W, Ryu K. Herniation pits in the femoral neck: a radiographic indicator of femoroacetabular impingement? Skeletal Radiol. 2011; 40:167–172. PMID: 20495799.

24. Nokes SR, Vogler JB, Spritzer CE, Martinez S, Herfkens RJ. Herniation pits of the femoral neck: appearance at MR imaging. Radiology. 1989; 172:231–234. PMID: 2740509.

25. Gao ZH, Yin JQ, Ma L, Wang J, Meng QF. Clinical imaging characteristics of herniation pits of the femoral neck. Orthop Surg. 2009; 1:189–195. PMID: 22009841.

26. Kassarjian A, Yoon LS, Belzile E, Connolly SA, Millis MB, Palmer WE. Triad of MR arthrographic findings in patients with cam-type femoroacetabular impingement. Radiology. 2005; 236:588–592. PMID: 15972331.

27. Chakraverty JK, Sullivan C, Gan C, Narayanaswamy S, Kamath S. Cam and pincer femoroacetabular impingement: CT findings of features resembling femoroacetabular impingement in a young population without symptoms. AJR Am J Roentgenol. 2013; 200:389–395. PMID: 23345362.

28. Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008; 466:264–272. PMID: 18196405.
29. Ito K, Minka MA 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001; 83:171–176. PMID: 11284559.
Fig. 1
Alpha angle was measured on oblique axial MR images parallel to axis of femoral neck.
Subsequently, prevalence of alpha angle ≥ 55° and herniation pit was calculated and statistical analysis was done regarding their association with age, gender, laterality of hip (right or left).
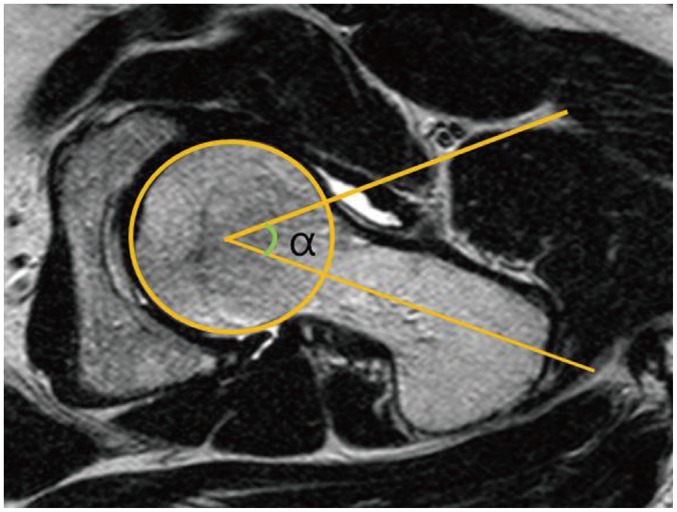
Fig. 2
Presence of herniation pit was determined on MRI.
It was shown as focal fibrocystic lesion with low signal intensity (arrow) on T1-weighted image (A) and intermediate to high signal intensity (arrow) on T2-weighted image (B) in location of femur head and neck junction.
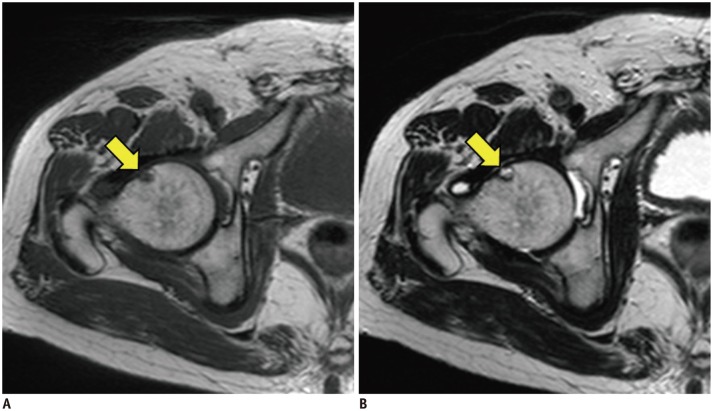
Table 1
MRI Protocol
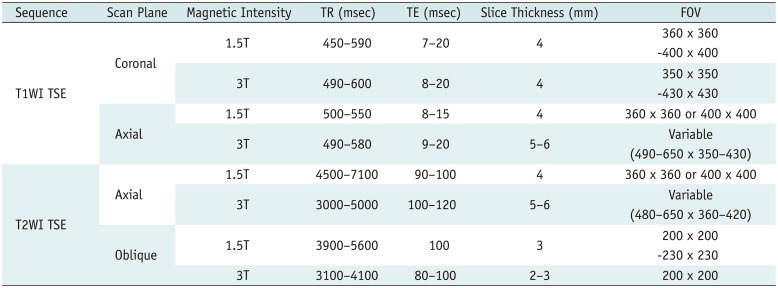
Table 2
Prevalence of Alpha Angle Over 55 Degrees and Herniation Pit




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download