Abstract
Purpose
The study aimed to evaluate the morphologic changes in transarterial chemoembolization (TACE) puncture sites implanted with an ExoSeal vascular closure device (VCD) using follow-up computed tomography (CT).
Materials and Methods
16 patients who used ExoSeal VCD after TACE were enrolled. Using CT images, the diameters and anterior wall thicknesses of the puncture sites in the common femoral artery (CFA) were compared with those of the contralateral CFA before TACE, at 1 month after every TACE session, and at the final follow-up period. The rates of complications were also evaluated.
Results
There were no puncture- or VCD-related complications. Follow-up CT images of the CFA's of patients who used ExoSeal VCDs showed eccentric vascular wall thickening with soft-tissue densities considered to be hemostatic plugs. Final follow-up CT images (mean, 616 days; range, 95–1106 days) revealed partial or complete resorption of the hemostatic plugs. The CFA puncture site diameters did not differ statistically from those of the contralateral CFA on the final follow-up CT (p > 0.05), regardless of the number of VCDs used.
Regional cancer therapy procedures such as transarterial chemoembolization (TACE) have become mainstay in the treatment of unresectable primary and metastatic hepatic malignancies. TACE extends the life expectancy of patients with advanced hepatocellular carcinoma, and it is now widely used for palliation. Arterial puncture is required to deliver chemotherapeutic agents to a hepatic tumor. In fact, patients often require one or more additional arterial punctures to treat partially cured or new lesions. Safe and effective catheter-directed therapy can increase survival in this population which often has other associated comorbid conditions (123). The vascular closure device (VCD) is widely used in this population for patient comfort and safety (45).
In the mid-1990s, the VCD was introduced into clinical practice with the aim of improving the efficacy and safety of percutaneous procedures (6). The devices are implanted to close the arteriotomy site of the vessel wall by targeted force. Different types of VCDs have been developed, including intravascular and extravascular devices (78). Increased efficacy, i.e., decreased time to hemostasis and earlier ambulation, has been a consistent finding in different VCD trials compared with manual compression (91011). VCD is preferred to manual compression in patients with coagulopathy (1213). The common femoral artery (CFA) is the most common puncture site and is usually included in the scanning range of follow-up abdominal CT images. However, changes in puncture sites after VCD insertion have seldom been reported.
The purpose of this study is to evaluate the morphologic changes in TACE puncture sites after VCD (ExoSeal; Cordis, Miami Lakes, FL, USA) implantation in patients using follow-up CT.
Our hospital's institutional review board approved this retrospective study and waived the informed consent requirement. We performed 628 TACE procedures in 600 patients between December 2008 and March 2014. A total of 67 VCDs were deployed in 58 patients with low coagulation profiles [platelet count < 50000/µL or prothrombin time–international normalized ratio (PT-INR) > 1.4], and in those who requested VCD implantation. Among those 58 patients, 24 patients who used ExoSeal VCD were evaluated further for inclusion in this study. Eight of the 24 ExoSeal VCD patients were excluded for the following reasons (Fig. 1): 1) contrast-enhanced abdominal CT examination was not performed before or after TACE (n = 4), 2) CFA images were not included in the pre- or post-TACE CT (n = 2), 3) both ExoSeal and another VCD were used in one patient during the study period (n = 2). A total of 16 patients (4 females, 12 males; mean age, 62.3 years; range, 45–78 years) were enrolled in this study. The mean serum platelet count was 64875/µL (range, 29000–161000) and mean PT-INR was 1.23 (range, 0.97–1.49). The demographic data of these 16 patients are summarized in Table 1.
Clinical information concerning the cases, including serum platelet count, PT-INR, number of closures with a VCD, number of punctures, and presence of complications were collected through a review of our institution's electronic medical records system.
All patients underwent pre-TACE abdominal CT imaging including the right CFA with the injection of contrast medium. The mean time between pre-TACE CT imaging and TACE was 39 days (range, 2–108 days), and there was no prior history of endovascular procedures requiring an arterial puncture via the CFA, especially on the right side.
The patients underwent follow-up CT examinations at our institution 1 month after every TACE session for evaluation of the viable tumor. If any viable portion of the tumor was detected, a subsequent TACE was performed. We reviewed all 1-month follow-up CT images, as well as the latest CT images, to evaluate long-term ExoSeal-related vessel wall changes. The mean time between the first TACE session and the final CT examination was 616 days (range, 95–1106).
Different CT systems (Somatom Definition Flash, Somatom Definition AS+, or Somatom Sensation 16, Siemens Medical Systems, Erlangen, Germany; and Discovery 750HD, General Electric Medical Systems, Milwaukee, WI, USA) were used at 180–250 mA and 120 kV. CT examinations included the area from the dome of the hemidiaphragm to the level of the femoral neck, and included unenhanced and contrast agent–enhanced dynamic imaging after initiation of the contrast agent injection (late arterial phase, 20–25 seconds; portal venous phase, 50–60 seconds; and delayed phase, 3–5 minutes).
All TACE procedures were performed via 5F sheath access in the right CFA. Upon completion, puncture sites were closed using an ExoSeal VCD. The VCDs were implanted by one author with 8 years of experience in interventional radiology (U.B.J.). Anticoagulation status and body habitus were assessed at the time of closure to ensure appropriate choice of closure device. After closure, patients were restricted to bedrest for 3 hours and then allowed to ambulate. Any evidence of complications was recorded and appropriate therapy was initiated.
The CT images were evaluated to consensus by two abdominal radiologists (J.W.L. and T.U.K.) who had 20 and 5 years of experience, respectively. One month after TACE, CT measurements were made of the diameters and anterior wall thicknesses of the puncture sites in the right CFA, and compared with measurements at the same level of the left CFA. All measurements were taken on the portal venous or delayed phase. The presence of puncture- and device-related complications such as pseudoaneurysm, arterial dissection, occlusion, arteriovenous fistula, luminal filling defect, large hematoma (> 3 cm), or groin infection was also evaluated. The CT images collected before TACE and during the follow-up periods were analyzed in the same manner. Special attention was given to match the CT images of the same patient at different follow-up time points by using several anatomical landmarks (i.e., femoral bifurcation, inguinal lymph nodes).
The differences in CT measurements of puncture site diameters and anterior wall thicknesses between the right and left CFA were compared using Student's t-test. The changes in CT measurements of the puncture site in the right CFA at different follow-up time points were compared using the Wilcoxon signed rank test. All of the statistical analyses were processed using SPSS 21.0 (IBM SPSS Statistics, IBM Corp., Armonk, NY, USA). A p-value < 0.05 was considered statistically significant.
The 16 patients included in this study underwent a total of 34 CFA punctures and 21 closures with an ExoSeal VCD. The mean number of punctures per patient was 2.13 (range, 1–5) and mean number of closures was 1.31 (range, 1–3).
The CT images 1 month after the first TACE demonstrated changes in the puncture sites compared to the pre-TACE CT images. They showed eccentric anterior wall thickening with soft-tissue densities at the punctured right CFA representing the hemostatic plug. The mean hemostatic plug size was 4.1 ± 1.6 mm (range, 2–7 mm).
Among the 16 patients, 13 patients (81%) used one ExoSeal VCD alone during the study period. The mean size of the hemostatic plug seen on the 1-month follow-up CT images after the first TACE of these patients was 3.6 mm (range, 2–4). The final CT images of these patients demonstrated partial or total absorption of the hemostatic plug. The mean size of the residual hemostatic plug on the final CT images was 1.0 mm (range, 0–4), a significantly smaller size compared to that seen in the 1-month follow-up CT images (p = 0.001). The final CT images of seven patients (54%) showed total resorption of the hemostatic plug. The mean duration between the first TACE and final CT examination in these patients was 727 days (range, 278–1106 days) (Fig. 2). The final CT images from the other six patients demonstrated partial resorption. The mean duration between the first TACE and final CT examination was 323 days (range, 95–614 days). The diameters of the CFA puncture sites (mean, 9.19 mm; range, 7–11 mm) were not statistically different from those of the contralateral CFA on the final follow-up CT (p = 0.885). The changes in hemostatic plug size and right femoral artery lumen diameter are summarized in Table 2.
Three patients had at least one repeated ipsilateral vascular closure. Two patients had three ExoSeal vascular closures, while the other patient had two vascular closures during the study period. The mean hemostatic plug size on the CT images 1 month after the first TACE session was 4.66 mm (range, 3–7mm). This was decreased to 2.00 mm (range, 0–4 mm) on the final CT images. The mean duration between the last VCD used in a TACE session and the final CT examination was 416 days (range, 234–587 days). The puncture site CFA diameters (mean, 9.19 mm; range, 7–11 mm) were not significantly different from the contralateral CFA diameters (mean, 9.13 mm; range, 9–11 mm) in the final follow-up CT images in both groups. The results are summarized in Table 3. No closure failures or VCD-related complications occurred in these patients.
In this study, we used ExoSeal VCDs for closing arteriotomy sites. The ExoSeal VCD is a novel, bioabsorbable device which is introduced directly through a vascular sheath. The device deploys a polyglycolic acid plug over the arteriotomy site, using a visually guided deployment mechanism (14). The 1-month follow-up CT examinations in this study showed eccentric wall thickening with soft-tissue densities at the anterior wall of the CFA, which resembled the bioabsorbable plug. Therefore, the eccentric soft-tissue dense wall thickening was assumed to be the hemostatic plug (15). We found that the diameters of the puncture site CFA did not differ significantly from the contralateral CFA on the 1-month and final follow-up CT images in both the single and multiple vascular closure groups, which suggests the safety of this VCD. Our results correspond to those of previous studies showing the safety and efficacy of these VCDs (71617). Because the hemostatic plug is attached to the outside of punctured vessel wall (18), it is assumed that the ExoSeal VCD rarely induced luminal narrowing in the vessel. It is known that the hemostatic plug of the ExoSeal is fully resorbed within 60–90 days (18), but only 54% of our cases showed a completely resorbed hemostatic plug. The remaining cases demonstrated partial resorption at a mean follow-up duration of 323 days, which was longer than the duration reported in a previous study. Choo et al. (15) evaluated the hemostatic plug change in an ExoSeal group in 6-month follow-up sonograms, and showed a partial resorption, consistent with our results.
Although it was a small number, three patients in this study underwent ExoSeal VCD implantation at least twice. There was no puncture-related problem such as pain or puncture failure during the study period, and follow-up CT images of these patients demonstrated no evidence of VCD-related complications. Boschewitz et al. (14) also showed that the ExoSeal VCD is safe and effective in repeated closures of retrograde percutaneous femoral arterial access in a study including a total of 404 repeated closures in non-cardiac settings such as transarterial hepatic procedures. They even demonstrated four cases of repeated vascular closures on the same day and an additional 196 cases in which the time between the two closures was shorter than the time the plug needs to dissolve completely (60–90 days), and reported no occurrence of hemostatic or technical difficulties in those cases.
This study had several limitations. First, it was retrospective and included a small number of patients with only one device and short follow-up periods. In particular, the sample size (n = 3) for repeated vascular closures was too small for interpreting the arterial changes after the repetitive punctures during TACE, which is usually done repetitively. Further evaluation with a large number of patients, and various VCDs with longer study periods, will be necessary for assessing clinical significance. Second, the follow-up durations and numbers of punctures of each patient were not exactly the same. Although these factors can affect vascular wall changes, the effect is considered minor. Third, no histological confirmation of the CT findings of the VCD vascular closures was performed. Moreover, there are no previous histological studies about the CT findings of VCD vascular closures. Thus, there is little definite evidence to interpret the CT findings. However, because the follow-up CT appearance of ExoSeal was very similar to the unique structure of the device, the eccentric anterior wall thickening with soft-tissue density was identified as the hemostatic plug of ExoSeal. Thus, a further histological study is required.
In conclusion, follow-up CT images in patients who underwent TACE and vascular closure with an ExoSeal VCD showed no evidence of significant vascular stenosis or significant vessel wall thickening despite repetitive punctures. Therefore, ExoSeal VCD can be used safely to achieve hemostasis after regional oncologic interventional procedures in patients with hepatic malignancy.
Figures and Tables
Fig. 1
Inclusion criteria.
CT = computed tomography, TACE = transarterial chemoembolization, VCD = vascular closure device

Fig. 2
A 59-year-old female patient (patient #4) underwent TACE for HCC, and after the procedure ExoSeal was applied in the right CFA. The second TACE was performed after 3 months of follow-up. At that time, the puncture site was closed using simple manual compression.
A. Preprocedural CT demostrates two patent CFAs with no wall thickening.
B. One-month follow-up CT shows eccentric wall thickening with soft-tissue density (white arrow) at the puncture site.
C. Seven-month follow-up CT demostrates disappearance of the soft-tissue density during the follow-up period.
CFA = common femoral artery, CT = computed tomography, HCC = hepatocellular carcinoma, TACE = transarterial chemoembolization

Table 1
Patient Demographics and Clinical Information

Table 2
Changes in Wall Thickness and Lumen of the Right Femoral Artery in the Single-Use ExoSeal Group (mm)
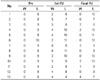
Table 3
Changes in Wall Thickness and Lumen of the Right Femoral Artery in the Multi-Use ExoSeal Group (mm)
| No | Pre | 1F | 2F | 3F | 4F | 5F | FF | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| W | L | W | L | W | L | W | L | W | L | W | L | W | L | |
| 1 | 0 | 8 | 3* | 7* | 7† | 8† | 3 | 8 | 5‡ | 8‡ | - | - | 2 | 9 |
| 2 | 0 | 9 | 7* | 9* | 2 | 9 | 2† | 9 | 1 | 8 | 3 | 9 | 4 | 9 |
| 3 | 0 | 12 | 4* | 10* | 1† | 11† | - | - | - | - | - | - | 0 | 11 |
*First VCD used TACE 1-month follow-up.
†Second VCD used TACE 1-month follow-up.
‡Third VCD used TACE 1-month follow-up.
Pre = pre-transarterial chemoembolization (TACE) computed tomography (CT), 1F–5F = first to fifth TACE 1-month follow-up CT, W = wall thickness of the right femoral artery (puncture site), L = diameter of the right femoral artery lumen, FF = final follow-up, VCD = vascular closure device
References
1. Lo CM, Ngan H, Tso WK, Liu CL, Lam CM, Poon RT, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002; 35:1164–1171.
2. Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology. 2003; 37:429–442.
3. Llovet JM, Real MI, Montaña X, Planas R, Coll S, Aponte J, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002; 359:1734–1739.
4. Marelli L, Shusang V, Senzolo M, Cholongitas E, Goode A, Yu D, et al. Repeated courses of transarterial embolization with polyvinyl alcohol particles: ‘long life elixir’ in a cirrhotic patient with unresectable hepatocellular carcinoma. Eur J Gastroenterol Hepatol. 2007; 19:329–332.
5. Ramsey DE, Kernagis LY, Soulen MC, Geschwind JF. Chemoembolization of hepatocellular carcinoma. J Vasc Interv Radiol. 2002; 13(9 Pt 2):S211–S221.
6. Tavris DR, Gallauresi BA, Lin B, Rich SE, Shaw RE, Weintraub WS, et al. Risk of local adverse events following cardiac catheterization by hemostasis device use and gender. J Invasive Cardiol. 2004; 16:459–464.
7. Schwartz BG, Burstein S, Economides C, Kloner RA, Shavelle DM, Mayeda GS. Review of vascular closure devices. J Invasive Cardiol. 2010; 22:599–607.
8. Lasic Z, Nikolsky E, Kesanakurthy S, Dangas G. Vascular closure devices: a review of their use after invasive procedures. Am J Cardiovasc Drugs. 2005; 5:185–200.
9. Wong SC, Bachinsky W, Cambier P, Stoler R, Aji J, Rogers JH, et al. A randomized comparison of a novel bioabsorbable vascular closure device versus manual compression in the achievement of hemostasis after percutaneous femoral procedures: the ECLIPSE (Ensure's Vascular Closure Device Speeds Hemostasis Trial). JACC Cardiovasc Interv. 2009; 2:785–793.
10. Chung J, Lee DW, Kwon OS, Kim BS, Shin YS. Angio-Seal™ Evolution™ versus manual compression for common femoral artery puncture in neurovascular diagnostic angiography: a prospective, non-randomized study. J Korean Neurosurg Soc. 2011; 49:153–156.
11. Upponi SS, Ganeshan AG, Warakaulle DR, Phillips-Hughes J, Boardman P, Uberoi R. Angioseal versus manual compression for haemostasis following peripheral vascular diagnostic and interventional procedures--a randomized controlled trial. Eur J Radiol. 2007; 61:332–334.
12. Hieb RA, Neisen MJ, Hohenwalter EJ, Molnar JA, Rilling WS. Safety and effectiveness of repeat arterial closure using the AngioSeal device in patients with hepatic malignancy. J Vasc Interv Radiol. 2008; 19:1704–1708.
13. McEvoy SH, McCarthy CJ, Lavelle LP, Moran DE, Cantwell CP, Skehan SJ, et al. Hepatocellular carcinoma: illustrated guide to systematic radiologic diagnosis and staging according to guidelines of the American Association for the Study of Liver Diseases. Radiographics. 2013; 33:1653–1668.
14. Boschewitz JM, Andersson M, Naehle CP, Schild HH, Wilhelm K, Meyer C. Retrospective evaluation of safety and effectiveness of the EXOSEAL vascular closure device for single vascular closure and closure after repeat puncture in diagnostic and interventional radiology: single-center experience. J Vasc Interv Radiol. 2013; 24:698–702.
15. Choo HJ, Jeong HW, Park JY, Jin SC, Kim ST, Seo JH, et al. Ultrasonographic features of vascular closure devices: initial and 6-month follow-up results. Ultrasonography. 2014; 33:283–290.
16. Biancari F, D'Andrea V, Di Marco C, Savino G, Tiozzo V, Catania A. Meta-analysis of randomized trials on the efficacy of vascular closure devices after diagnostic angiography and angioplasty. Am Heart J. 2010; 159:518–531.
17. Eggebrecht H, Haude M, Woertgen U, Schmermund A, von Birgelen C, Naber C, et al. Systematic use of a collagen-based vascular closure device immediately after cardiac catheterization procedures in 1,317 consecutive patients. Catheter Cardiovasc Interv. 2002; 57:486–495.
18. Krishnasamy VP, Hagar MJ, Scher DJ, Sanogo ML, Gabriel GE, Sarin SN. Vascular closure devices: technical tips, complications, and management. Tech Vasc Interv Radiol. 2015; 18:100–112.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download