Abstract
Pulmonary pleomorphic carcinoma is an uncommon malignant lesion of the lung. A chest radiograph of 53-year-old man who was suffering from a cough revealed a well-defined mass-like opacity with a broad base on the pleura at the apico-posterior segment of the right upper lobe of the lung. The subsequent chest computed tomography (CT) scan demonstrated an inhomogeneous enhancing mass with central low-attenuation in the right upper lobe. A lobectomy was performed and the mass was determined to be a pleomorphic carcinoma with visceral pleura invasion. Forty days after the operation, the patient complained of melena and an abdominal CT revealed an intraluminal and extraluminal protruding mass around the prepyloric antrum and duodenal bulb. The mass was removed by en-block surgery and diagnosed as metastatic pleomorphic carcinoma from the lung. Previous articles reported a median survival time of 3–10 months for pleomorphic carcinoma, but in this case, the patient has continued to survive, 11 years after surgery. Chest and abdominal CTs have revealed no evidence of tumor recurrence or metastasis.
Pleomorphic carcinomas of the lung form a subgroup of general carcinomas exhibiting pleomorphic, sarcomatoid, or sarcomatous elements. The World Health Organization defines pleomorphic carcinoma of the lung as non-small cell lung cancer (with a carcinomatous or epithelial component) combined with neoplastic spindle or giant cells (with a sarcomatous or mesenchymal component) or as a carcinoma consisting only of spindle and giant cells (1).
Pulmonary pleomorphic carcinoma associated with intraperitoneal metastasis is extremely rare. We report an instance of the duodenal metastasis of a pulmonary pleomorphic carcinoma, in addition to providing a review of the literature.
A 53-year-old male was referred from another hospital to our department of respiratory medicine due to persistent coughing. A chest radiograph revealed a well-defined mass-like opacity, with a broad base on the pleura at the apico-posterior segment of the right upper lung lobe (Fig. 1A). Laboratory data revealed low hemoglobin (8.6 g/dL) and hematocrit levels (28%). The serum carcinoembryonic antigen and carbohydrate antigen 19-9 levels were normal. The erythrocyte sedimentation rate was 120 mm/h (normal, 0–30 mm/h) and the white blood cell count was slightly elevated (11.1 × 103/µL).
Three days later, a chest computed tomography (CT) scan (HiSpeed Advantage Scanner; GE Medical Systems, Waukesha, WI, USA) revealed a 5.7 × 5.6 cm-sized inhomogeneous enhancing mass, with a central low-attenuation region, in the peripheral area of the right upper lung lobe; the mass abutted the adjacent visceral pleura (Fig. 1B). The lesion exhibited slight wash-out in the delay enhancement phase. In addition, a 10-mm diameter oval lymph node was noted at the right lower paratracheal nodal station. Two weeks after the CT, a right upper lobectomy was performed. The mass was determined to be a pleomorphic carcinoma that had invaded the visceral pleura. Also, metastasis to the mediastinal lymph nodes was confirmed in the surgical specimens.
Upon gross pathological examination of the resected specimen, the relatively well-defined, grayish-yellow solid mass was 5.0 × 4.7 cm and exhibited focal inner necrosis. The tumor mass involved the visceral pleura. Microscopically, the tumor was a mixed spindle cell (Fig. 1C) and giant cell (Fig. 1D) carcinoma. Immunohistochemically, the tumor was positive for pan-cytokeratin and vimentin.
The region of well enhancing area on contrast-enhanced CT corresponded to the cellular/collagenous tissue of the tumor on pathology; the region exhibiting myxoid degeneration and hemorrhagic foci corresponded to that area exhibiting low attenuation on contrast-enhanced CT scans.
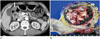
Forty days after the operation, the patient complained of melena, and a gastrofiberoscopy was conducted. An ulcerating mass was evident at the duodenal bulb, and a biopsy was performed. An abdominal CT revealed a mass protruding intra- and extraluminally around the prepyloric antrum and duodenal bulb (Fig. 2A).
The mass was removed by en-block surgery. Histologically, the duodenal mass was a metastatic pleomorphic carcinoma from the lung. The resected duodenal specimen was a serosal protruding mass, 5.5 × 5.6 in size and exhibited mucosal ulceration. On sectioning, the tumor was a well-defined gray-yellowish solid mass exhibiting extensive hemorrhage and necrosis (Fig. 2B). Microscopically, the tumor was similar, both histologically and immunohistochemically, to the lung tumor.
Pleomorphic carcinoma is diagnosed when non-small cell lung carcinoma is associated with neoplastic spindle and/or giant cells, or when the carcinoma contains only spindle and giant cells (2). Kim et al. (3) found that the most frequent epithelial component was large cells, followed by squamous cells. Immunohistochemical staining may aid in the diagnosis of lung pleomorphic carcinoma when the extent of carcinomatous differentiation is difficult to discern by light microscopy (45). Several antibodies can be used to differentiate the components of a pleomorphic carcinoma (456). Anti-vimentin and anti-cytokeratin antibodies are commonly used for the immunohistochemical staining of spindle cells and epithelial cells, respectively (456).
Such tumors account for only 0.1–0.4% of all lung malignancies (4) and occur principally in males who smoke heavily. The average age at diagnosis is 60 years (467).
Rossi et al. (6) reported that pleomorphic carcinomas present as large, frequently peripheral necrotic masses involving the upper lobes principally (48% of all cases). Of all cases, 33% were peripheral tumors.
Such tumors are associated with poor prognoses (24). Six of 10 patients were reported to have died within 5 months of surgery (2). Chang et al. (4) found that the median survival time was 3 months. An earlier report found that the median survival time was 10 months (7). Raveglia et al. (8) reported that 16 of 20 patients with pleomorphic carcinomas died from early distant metastases. In that series, the median disease-free survival was 5 months and the median overall survival was 8 months. The causes of death were local recurrence and distant metastasis, and the prognosis seemed to depend on the extent of the sarcomatous tumor component. The most frequent sites of metastasis were the lymph nodes, but metastases also developed in many other organs, most commonly the kidney, bone, liver, lung, spleen, and gastrointestinal tract.
In several cases, distant metastases were not found on preoperative systemic examination, but rather during surgery or postoperatively. Segawa et al. (9) reported that multiple metastases of a pleomorphic carcinoma of the lung developed rapidly after surgery in a 73-year-old male; the patient was diagnosed with pleomorphic carcinoma of the lung, pT2N0M0, stage IB during a preoperative systemic examination. However, by postoperative day 30, new metastatic lesions had developed in the thoracic skin, liver, diaphragm, bilateral adrenal glands, and retroperitoneal space. The patient died of peritonitis and pleuritis only 60 days after surgery.
Aketa et al. (10) reported two cases of younger male patients with rapidly progressing pulmonary pleomorphic carcinoma; metastases were found during surgery. Chest radiographs and CT revealed huge lung tumors but no distant metastases. The cited authors attempted pneumonectomies but found that the tumors had invaded the aorta, the pulmonary artery, the pericardium, and the pleura. One patient underwent a pneumonectomy followed by systemic chemotherapy including cisplatin and irinotecan. The other patient underwent a segmentectomy and radiation therapy. Both exhibited rapidly growing neoplasms that were only marginally sensitive to chemotherapy or radiotherapy. Pulmonary pleomorphic carcinoma is thus a form of lung cancer with a poor prognosis if the tumor is not resected at an early stage.
Our patient had a mass in the right upper lobe, with invasion of the visceral pleura, and a lobectomy was performed. Fortythree days after surgery, duodenal metastasis was evident on an abdominal CT, and further surgery was performed. The patient remains alive today (11 years after surgery), and neither chest nor abdominal CT have yielded any evidence of tumor recurrence or metastasis. It is very rare to have such a case of pulmonary plomorphic carcinoma with distant metastasis that shows long-term disease-free survival.
Figures and Tables
Fig. 1
Pleomorphic carcinoma of the lung in a 53-year-old man.
A. A chest postero-anterior radiograph reveals a well-defined mass with a maximum diameter of 8.2 cm (arrows) in the right upper lobe.
B. A transverse contrast-enhanced CT scan shows a 5.7 cm sized, inhomogeneously enhancing mass lesion with inner low attenuated area (star) in the peripheral lung area of the right upper lobe. The mass abutted the adjacent visceral pleura (arrow).
C, D. Photomicrographs of histopathologic specimens (hematoxylin and eosin staining, × 200) show a mixed composition of spindle cell carcinoma (C) and giant cell carcinoma (D).
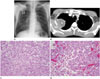
Fig. 2
Duodenal metastasis of pulmonary pleomorphic carcinoma.
A. A transverse contrast-enhanced abdominal CT scan shows an intraluminal (arrow) and extraluminal (star) protruding mass around prepyloric antrum and duodenal bulb.
B. A photograph of gross specimen of duodenum reveals well-defined serosal mass with extensive hemorrhagic necrosis and mucosal ulceration.
References
1. Brambilla E, Travis WD, Colby TV, Corrin B, Shimosato Y. The new World Health Organization classification of lung tumours. Eur Respir J. 2001; 18:1059–1068.
2. Kim TH, Kim SJ, Ryu YH, Lee HJ, Goo JM, Im JG, et al. Pleomorphic carcinoma of lung: comparison of CT features and pathologic findings. Radiology. 2004; 232:554–559.
3. Kim TS, Han J, Lee KS, Jeong YJ, Kwak SH, Byun HS, et al. CT findings of surgically resected pleomorphic carcinoma of the lung in 30 patients. AJR Am J Roentgenol. 2005; 185:120–125.
4. Chang YL, Lee YC, Shih JY, Wu CT. Pulmonary pleomorphic (spindle) cell carcinoma: peculiar clinicopathologic manifestations different from ordinary non-small cell carcinoma. Lung Cancer. 2001; 34:91–97.
5. Yoo SH, Han J, Kim TJ, Chung DH. Expression of CD99 in pleomorphic carcinomas of the lung. J Korean Med Sci. 2005; 20:50–55.
6. Rossi G, Cavazza A, Sturm N, Migaldi M, Facciolongo N, Longo L, et al. Pulmonary carcinomas with pleomorphic, sarcomatoid, or sarcomatous elements: a clinicopathologic and immunohistochemical study of 75 cases. Am J Surg Pathol. 2003; 27:311–324.
7. Fishback NF, Travis WD, Moran CA, Guinee DG Jr, McCarthy WF, Koss MN. Pleomorphic (spindle/giant cell) carcinoma of the lung. A clinicopathologic correlation of 78 cases. Cancer. 1994; 73:2936–2945.
8. Raveglia F, Mezzetti M, Panigalli T, Furia S, Giuliani L, Conforti S, et al. Personal experience in surgical management of pulmonary pleomorphic carcinoma. Ann Thorac Surg. 2004; 78:1742–1747.
9. Segawa M, Kusajima Y, Saito K. [Pleomorphic carcinoma of the lung rapidly developed multiple metastases after surgery]. Kyobu Geka. 2006; 59:387–391.
10. Aketa A, Yamada G, Aketa K, Ohnishi T, Takahashi Y, Kudoh K, et al. [Two younger male patients with rapidly progressing pulmonary pleomorphic carcinoma]. Nihon Kokyuki Gakkai Zasshi. 2004; 42:164–169.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download