Abstract
Breast metastases from extramammary malignancies are uncommon. Although metastatic lesions show variable radiologic features, there have been few reports of metastatic breast cancer with negative sonographic findings. Furthermore, the results of several studies have indicated a high negative predictive value when ultrasonographic and mammographic findings were normal in the setting of a palpable lump, and follow-up is recommended when the physical examination is not highly suspicious. Herein, we report a case of a 26-year-old woman with breast metastasis from a known gastric adenocarcinoma, which had negative findings without any evidence of suspicious features for malignancy on the initial mammogram and ultrasound.
Metastases to the breast from extramammary malignancies are uncommon (1). When such metastases do occur, lymphomas/leukemias and melanomas are the most common, while some of the less common sources include carcinomas of the lung, ovary, and stomach (12). Although breast metastases show va-riable sonographic features (2), reports of metastatic breast cancer with negative mammographic and ultrasonographic (US) findings have been rare (345). Although the false-negative rate of mammography in the detection of breast cancer has been consistently reported as approximately 10%, US is considered to be an adequate method for guiding the effective evaluation of women with palpable breast lesions. We describe a case of a delayed diagnosis of metastatic breast cancer originating from the stomach, which presented as a palpable breast lump with negative imaging findings initially.
A 26-year-old woman with a history of stomach cancer was referred to the breast center of our hospital for the evaluation of a palpable lump in the left upper-inner breast. The patient had been treated with chemotherapy for gastric adenocarcinoma and peritoneal seeding metastasis for the past year. There was no family history of any breast or gynecological malignancy, and no prior breast imaging had been conducted. A physical examination revealed an irregular, lumpy growth with tenderness at the 10 o'clock position. No axillary or supraclavicular lymph nodes were palpable. Due to the youth of the patient, ultrasound examinations (US) were taken first. The US showed normal fibroglandular tissue with heterogeneous echotexture and no evidence of an abnormal mass lesion (Fig. 1A). Additionally, the US findings were symmetric with the corresponding area of the contralateral breast (Fig. 1B). Because there were negative imaging findings in the patient despite a palpable breast lump, digital mammograms were next performed. The breast tissue was extremely dense, and no definite areas of mass lesions or microcalcifications were noted (Fig. 1C, D). One month later, the patient revisited the hospital due to the enlargement of the palpable br-east lump with pain and a local heating sensation. A targeted US taken at that time showed a more heterogeneous echotexture characterized by large areas of markedly decreased echogenecity without a discrete mass lesion. Skin thickening was also noted (Fig. 1E). A power Doppler US showed no vascularity in the lesion. The ipsilateral axillary lymph node showed eccentric cortical thickening (Fig. 1F). A US-guided core needle biopsy was performed at the hypoechoic area of the palpable lesion. The biopsy specimen was pathologically confirmed to be adenocarcinoma, consistent with metastasis from the stomach (Fig. 2). Although the patient underwent several cycles of chemotherapy with paclitaxel and cisplatin, she expired from the disease one year later.
Metastasis to the breast from extramammary malignancies is considered to be an uncommon occurrence, accounting for 0.5-1.3% of all breast malignancies. Most metastatic lesions are the result of metastasis from the contralateral breast; however, rare occurrences of metastasis from a primary malignancy have been reported (1267). Such cases of metastases to the breast are marked by the presence of large areas of fibrous tissue with a relatively poor blood supply (7).
Breast metastases from extramammary malignancies can occur through either the hematogenous or lymphatic routes. Common radiologic features of metastatic disease of the breast have been associated with the route of metastasis; however, these features are not specific (7). Typical features of hematogenous metastases include one or more well circumscribed hypoechoic mass without spiculations, calcification, and a superficial location. Typical US features of lymphatic breast metastases include diffusely and heterogeneously increased echogenicities in subcutaneous fat and glandular tissue, as well as a thick trabecular pattern with secondary skin thickening, lymphedema, and lym-ph node enlargement. The results of one study suggested that carcinomas of the stomach more frequently caused diffuse architectural distortions, whereas other malignancies tended to present as intramammary masses (7). In this case, the follow-up breast US revealed markedly decreased echogenecity and diffuse skin thickening without a discrete mass lesion, combined with ipsilateral lymph node enlargement. Therefore, these imaging findings implied a strong probability of lymphatic metastasis.
Breast metastasis from stomach cancer that mimics normal breast parenchyma is regarded as even more infrequent (89). One report described breast metastasis from rhabdomyosarcoma (8), and other reports have detailed lymphoma involving the breast, which was detected only through the use of fluorodeoxyglucose positron emission tomography, despite negative findings on mammography, sonography, and in the physical examination (9). Patients with palpable breast masses commonly present for imaging evaluations. The results of several studies have revealed a high negative predictive value of combined negative sonographic and mammographic findings in patients with a palpable abnormality in the breast, ranging from 96.5% to 100% (345). However, prompt tissue sampling has been recommended in cases with suspicious findings from the physical examination. According to the 5th edition of Breast Imaging Reporting and Data System (BI-RADS) (10), the assessment-management mismatch is permitted for several specific clinical scenarios. In the case of negative image findings in patients with palpable breast lumps (BI-RADS category 1), the interpreting physician may want to suggest surgical consultation or tissue diagnosis to cover the possibility that the palpable breast cancer might not be visible with breast imaging, as in the present case.
In summation, breast metastasis from stomach cancer may mimic prominent fibroglandular tissue on breast sonography. Therefore, the possibility of metastasis should be considered in patients who have a primary malignancy in other organs and a palpable breast lesion. In such cases, tissue sampling should not be delayed if the results of the physical examination raise suspicions, regardless of negative sonographic and mammographic findings.
Figures and Tables
Fig. 1
A 26-year-old female with a palpable lump in the left breast.
A. Initial ultrasonographic (US) of the palpable area at the left 10-o'clock position shows heterogeneous fibroglandular tissue without a discrete mass lesion.
B. Symmetric parenchymal echotexture is noted in the corresponding area of the contralateral breast (right 2-o'clock).
C, D. Left craniocaudal (C) and mediolateral oblique (D) mammograms show extremely dense parenchyma and no abnormal findings at the palpable radiopaque BB marker area (black arrows) of the left-upper inner breast.
E. Follow-up US after 1 month was conducted due to an enlargement of the palpable breast lump. Targeted US shows a further heterogeneous echotexture characterized by large areas of decreased echogenecity without a discrete mass lesion. Skin thickening is also observed.
F. US of the ipsilateral axillary lymph node shows eccentric cortical thickening (white arrow).

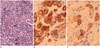
Fig. 2
Histopathology of the breast biopsy specimen.
A. The tumor cells seem to be signet ring cells with abundant intracytoplasmic mucin (arrows), and poorly differentiated small pleomorphic features are frequently recognized as well (hematoxylin and eosin, × 200).
B, C. Cytokeratin (CK) 20 (B) and CK7 (C) staining are both positive (× 400).
References
1. Wood B, Sterrett G, Frost F, Swarbrick N. Diagnosis of extramammary malignancy metastatic to the breast by fine needle biopsy. Pathology. 2008; 40:345–351.
2. Surov A, Fiedler E, Holzhausen HJ, Ruschke K, Schmoll HJ, Spielmann RP. Metastases to the breast from non-mammary malignancies: primary tumors, prevalence, clinical signs, and radiological features. Acad Radiol. 2011; 18:565–574.
3. Shetty MK, Shah YP. Prospective evaluation of the value of negative sonographic and mammographic findings in patients with palpable abnormalities of the breast. J Ultrasound Med. 2002; 21:1211–1216. quiz 1217-1219
4. Dennis MA, Parker SH, Klaus AJ, Stavros AT, Kaske TI, Clark SB. Breast biopsy avoidance: the value of normal mammograms and normal sonograms in the setting of a palpable lump. Radiology. 2001; 219:186–191.
5. Lee JH, Kim EK, Yoon SK, Choi S, Nam KJ, Cho SH, et al. The Clinical Significance of Normal Mammograms and Normal Sonograms in Patients with Palpable Abnormalities of the Breast. J Korean Radiol Soc. 2006; 55:299–304.
6. Mun SH, Ko EY, Han BK, Shin JH, Kim SJ, Cho EY. Breast metastases from extramammary malignancies: typical and atypical ultrasound features. Korean J Radiol. 2014; 15:20–28.
7. Abbas J, Wienke A, Spielmann RP, Bach AG, Surov A. Intramammary metastases: comparison of mammographic and ultrasound features. Eur J Radiol. 2013; 82:1423–1430.
8. Ahn SJ, Kim SK, Kim EK. Metastatic breast cancer from rhabdomyosarcoma mimicking normal breast parenchyma on sonography. J Ultrasound Med. 2010; 29:489–492.
9. Kyoung Jung H, Kim EK, Yun M, Jung Kim M, Young Kwak J. Bilateral breasts involvement in Burkitt's lymphoma detected only by FDG-PET. Clin Imaging. 2006; 30:57–59.
10. American College of Radiology. ACR BI-RADS Mammography. In : Sickles EA, D'Orsi CJ, Bassett LW, Appleton CM, Berg WA, Burnside ES, editors. ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System. Reston, VA: American College of Radiology;2013.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download