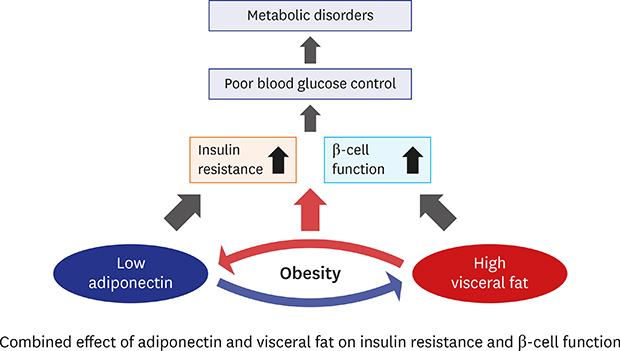
1. Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006; 444(7121):840–846.


2. Ibrahim MM. Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev. 2010; 11(1):11–18.


3. Balsan GA, Vieira JL, Oliveira AM, Portal VL. Relationship between adiponectin, obesity and insulin resistance. Rev Assoc Med Bras (1992). 2015; 61(1):72–80.


5. Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun. 1999; 257(1):79–83.


8. Patané G, Caporarello N, Marchetti P, Parrino C, Sudano D, Marselli L, et al. Adiponectin increases glucose-induced insulin secretion through the activation of lipid oxidation. Acta Diabetol. 2013; 50(6):851–857.


9. Matsushita Y, Nakagawa T, Yamamoto S, Kato T, Ouchi T, Kikuchi N, et al. Adiponectin and visceral fat associate with cardiovascular risk factors. Obesity (Silver Spring). 2014; 22(1):287–291.


10. Cho SA, Joo HJ, Cho JY, Lee SH, Park JH, Hong SJ, et al. Visceral fat area and serum adiponectin level predict the development of metabolic syndrome in a community-based asymptomatic population. PLoS One. 2017; 12(1):e0169289.

11. Okauchi Y, Nishizawa H, Funahashi T, Ogawa T, Noguchi M, Ryo M, et al. Reduction of visceral fat is associated with decrease in the number of metabolic risk factors in Japanese men. Diabetes Care. 2007; 30(9):2392–2394.


12. Bi X, Seabolt L, Shibao C, Buchowski M, Kang H, Keil CD, et al. DXA-measured visceral adipose tissue predicts impaired glucose tolerance and metabolic syndrome in obese Caucasian and African-American women. Eur J Clin Nutr. 2015; 69(3):329–336.


13. Inoue M, Maehata E, Yano M, Taniyama M, Suzuki S. Correlation between the adiponectin-leptin ratio and parameters of insulin resistance in patients with type 2 diabetes. Metabolism. 2005; 54(3):281–286.


14. Weber KS, Strassburger K, Pacini G, Nowotny B, Müssig K, Szendroedi J, et al. Circulating adiponectin concentration is inversely associated with glucose tolerance and insulin secretion in people with newly diagnosed diabetes. Diabet Med. 2017; 34(2):239–244.


16. Oka R, Yagi K, Sakurai M, Nakamura K, Nagasawa SY, Miyamoto S, et al. Impact of visceral adipose tissue and subcutaneous adipose tissue on insulin resistance in middle-aged Japanese. J Atheroscler Thromb. 2012; 19(9):814–822.


17. Scheuer SH, Færch K, Philipsen A, Jørgensen ME, Johansen NB, Carstensen B, et al. Abdominal fat distribution and cardiovascular risk in men and women with different levels of glucose tolerance. J Clin Endocrinol Metab. 2015; 100(9):3340–3347.


18. Shim JS, Song BM, Lee JH, Lee SW, Park JH, Choi DP, et al. Cardiovascular and Metabolic Diseases Etiology Research Center (CMERC) cohort: study protocol and results of the first 3 years of enrollment. Epidemiol Health. 2017; 39:e2017016.

20. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28(7):412–419.

21. Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999; 22(9):1462–1470.


22. Bergman RN, Belfiore F, Molinatti GM. Current topics in diabetes research. In : Turner R, Levy J, Rudenski A, Hammersley M, Page R, editors. Measurement of Insulin Resistance and Beta-cell Function: the HOMA and CIGMA Approach. Berlin: Karger Publishers;1993. p. 66–75.
23. Goedecke JH, Dave JA, Faulenbach MV, Utzschneider KM, Lambert EV, West S, et al. Insulin response in relation to insulin sensitivity: an appropriate beta-cell response in black South African women. Diabetes Care. 2009; 32(5):860–865.


26. Utzschneider KM, Carr DB, Hull RL, Kodama K, Shofer JB, Retzlaff BM, et al. Impact of intra-abdominal fat and age on insulin sensitivity and beta-cell function. Diabetes. 2004; 53(11):2867–2872.

27. Wagenknecht LE, Langefeld CD, Scherzinger AL, Norris JM, Haffner SM, Saad MF, et al. Insulin sensitivity, insulin secretion, and abdominal fat: the Insulin Resistance Atherosclerosis Study (IRAS) Family Study. Diabetes. 2003; 52(10):2490–2496.


28. Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. 1999. Biochem Biophys Res Commun. 2012; 425(3):560–564.

29. Halleux CM, Takahashi M, Delporte ML, Detry R, Funahashi T, Matsuzawa Y, et al. Secretion of adiponectin and regulation of apM1 gene expression in human visceral adipose tissue. Biochem Biophys Res Commun. 2001; 288(5):1102–1107.


30. Maeda N, Takahashi M, Funahashi T, Kihara S, Nishizawa H, Kishida K, et al. PPARgamma ligands increase expression and plasma concentrations of adiponectin, an adipose-derived protein. Diabetes. 2001; 50(9):2094–2099.

32. Winzell MS, Nogueiras R, Dieguez C, Ahrén B. Dual action of adiponectin on insulin secretion in insulin-resistant mice. Biochem Biophys Res Commun. 2004; 321(1):154–160.


33. Staiger K, Stefan N, Staiger H, Brendel MD, Brandhorst D, Bretzel RG, et al. Adiponectin is functionally active in human islets but does not affect insulin secretory function or beta-cell lipoapoptosis. J Clin Endocrinol Metab. 2005; 90(12):6707–6713.

34. Okamoto M, Ohara-Imaizumi M, Kubota N, Hashimoto S, Eto K, Kanno T, et al. Adiponectin induces insulin secretion in vitro and in vivo at a low glucose concentration. Diabetologia. 2008; 51(5):827–835.


35. Roh E, Kim KM, Park KS, Kim YJ, Chun EJ, Choi SH, et al. Comparison of pancreatic volume and fat amount linked with glucose homeostasis between healthy Caucasians and Koreans. Diabetes Obes Metab. 2018; 20(11):2642–2652.


36. Basu R, Dalla Man C, Campioni M, Basu A, Klee G, Toffolo G, et al. Effects of age and sex on postprandial glucose metabolism: differences in glucose turnover, insulin secretion, insulin action, and hepatic insulin extraction. Diabetes. 2006; 55(7):2001–2014.


39. Rössner S, Bo WJ, Hiltbrandt E, Hinson W, Karstaedt N, Santago P, et al. Adipose tissue determinations in cadavers--a comparison between cross-sectional planimetry and computed tomography. Int J Obes. 1990; 14(10):893–902.

41. Snijder MB, Visser M, Dekker JM, Seidell JC, Fuerst T, Tylavsky F, et al. The prediction of visceral fat by dual-energy X-ray absorptiometry in the elderly: a comparison with computed tomography and anthropometry. Int J Obes Relat Metab Disord. 2002; 26(7):984–993.









 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download