1. Dhanwal DK, Cooper C, Dennison EM. Geographic variation in osteoporotic hip fracture incidence: the growing importance of Asian influences in coming decades. J Osteoporos. 2010; 2010:757102.

4. Wade SW, Strader C, Fitzpatrick LA, Anthony MS, O'Malley CD. Estimating prevalence of osteoporosis: examples from industrialized countries. Arch Osteoporos. 2014; 9(1):182.

5. Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ 3rd, Khaltaev N. A reference standard for the description of osteoporosis. Bone. 2008; 42(3):467–475.

6. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, et al. Proximal femur bone mineral levels of US adults. Osteoporos Int. 1995; 5(5):389–409.

7. Tenenhouse A, Joseph L, Kreiger N, Poliquin S, Murray TM, Blondeau L, et al. Estimation of the prevalence of low bone density in Canadian women and men using a population-specific DXA reference standard: the Canadian Multicentre Osteoporosis Study (CaMos). Osteoporos Int. 2000; 11(10):897–904.

8. Emaus N, Omsland TK, Ahmed LA, Grimnes G, Sneve M, Berntsen GK. Bone mineral density at the hip in Norwegian women and men--prevalence of osteoporosis depends on chosen references: the Tromsø Study. Eur J Epidemiol. 2009; 24(6):321–328.

9. Barrett-Connor E, Siris ES, Wehren LE, Miller PD, Abbott TA, Berger ML, et al. Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res. 2005; 20(2):185–194.

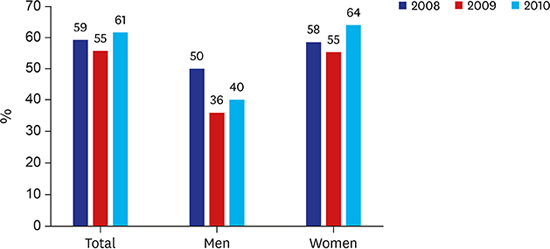
10. Choi YJ, Oh HJ, Kim DJ, Lee Y, Chung YS. The prevalence of osteoporosis in Korean adults aged 50 years or older and the higher diagnosis rates in women who were beneficiaries of a national screening program: the Korea National Health and Nutrition Examination Survey 2008–2009. J Bone Miner Res. 2012; 27(9):1879–1886.

11. Kim TY, Jang S, Park CM, Lee A, Lee YK, Kim HY, et al. Trends of incidence, mortality, and future projection of spinal fractures in Korea using nationwide claims data. J Korean Med Sci. 2016; 31(5):801–805.

12. Ha YC, Kim TY, Lee A, Lee YK, Kim HY, Kim JH, et al. Current trends and future projections of hip fracture in South Korea using nationwide claims data. Osteoporos Int. 2016; 27(8):2603–2609.

13. Kwon GD, Jang S, Lee A, Park CM, Lee YK, Kim TY, et al. Incidence and mortality after distal radius fractures in adults aged 50 years and older in Korea. J Korean Med Sci. 2016; 31(4):630–634.

14. Jang S, Park C, Jang S, Yoon HK, Shin CS, Kim DY, et al. Medical service utilization with osteoporosis. Endocrinol Metab (Seoul). 2010; 25(4):326–339.

15. Korean National Health and Nutrition Examination Survey in 2008–2010 results presentation. Updated 2011. Accessed Apr 1, 2017.
http://knhanes.cdc.go.kr.
16. McCombs JS, Thiebaud P, McLaughlin-Miley C, Shi J. Compliance with drug therapies for the treatment and prevention of osteoporosis. Maturitas. 2004; 48(3):271–287.

17. Abramowicz S, Kim S, Prahalad S, Chouinard AF, Kaban LB. Juvenile arthritis: current concepts in terminology, etiopathogenesis, diagnosis, and management. Int J Oral Maxillofac Surg. 2016; 45(7):801–812.

19. Lee J, Lee S, Jang S, Ryu OH. Age-related changes in the prevalence of osteoporosis according to gender and skeletal site: the Korea National Health and Nutrition Examination Survey 2008–2010. Endocrinol Metab. 2013; 28(3):180–191.

20. Lim Y, Jo K, Ha HS, Yim HW, Yoon KH, Lee WC, et al. The prevalence of osteoporosis and the rate of bone loss in Korean adults: the Chungju metabolic disease cohort (CMC) study. Osteoporos Int. 2017; 28(4):1453–1459.

21. Choi HJ, Shin CS, Ha YC, Jang S, Jang S, Park C, et al. Burden of osteoporosis in adults in Korea: a national health insurance database study. J Bone Miner Metab. 2012; 30(1):54–58.

22. Gillespie CW, Morin PE. Osteoporosis-related health services utilization following first hip fracture among a cohort of privately-insured women in the United States, 2008–2014: an Observational Study. J Bone Miner Res. 2017; 32(5):1052–1061.

23. Kim HS, Shin DW, Lee WC, Kim YT, Cho B. National screening program for transitional ages in Korea: a new screening for strengthening primary prevention and follow-up care. J Korean Med Sci. 2012; 27:Suppl. S70–S75.

24. Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013; 8:136.

25. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998–2005. Diabetes Care. 2009; 32(11):2016–2020.

26. Kim KI, Chang HJ, Cho YS, Youn TJ, Chung WY, Chae IH, et al. Current status and characteristics of hypertension control in community resident elderly Korean people: data from a Korean longitudinal study on health and aging (KLoSHa study). Hypertens Res. 2008; 31(1):97–105.









 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download