This article has been
cited by other articles in ScienceCentral.
To the Editor:
We read with interest the article by Chan Hong Jeon in the November 2016 issue of the
Journal of Korean Medical Science regarding 3 cases of central nervous system involvement in relapsing polychondritis (RP) (
1). Neurological involvement is indeed a rare but serious condition in RP, and raises difficulties in diagnosis.
We report another case which illustrates the most important differential diagnosis to rule out in the presence of neurological involvement in patient with RP. A 34-years-old Turkish woman, with bilateral auricular, nasal chondritis and laryngeal involvement, was diagnosed with RP, according to McAdam's criteria in February 2013 (
2). She was initially treated by corticosteroids and intravenous cyclophosphamide (6 pulses), followed by mycophenolate mofetil (2 g/day). Subcutaneous methotrexate was initiated in June 2014 because of recurrent exacerbations. In October 2014, she presented with fever at 40°C and high elevation of inflammation biomarkers without bacteriological documentation
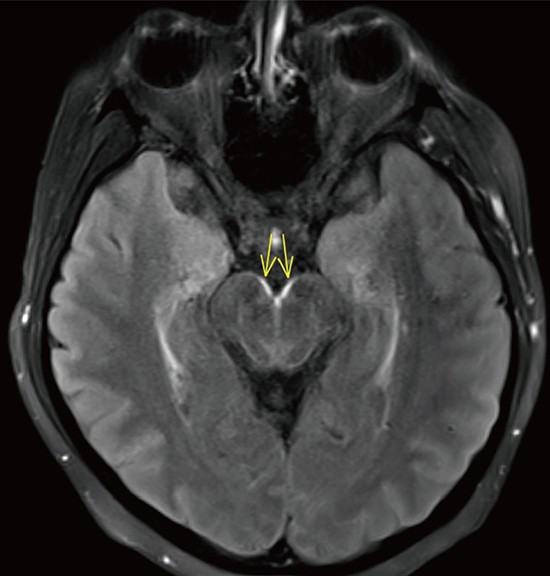
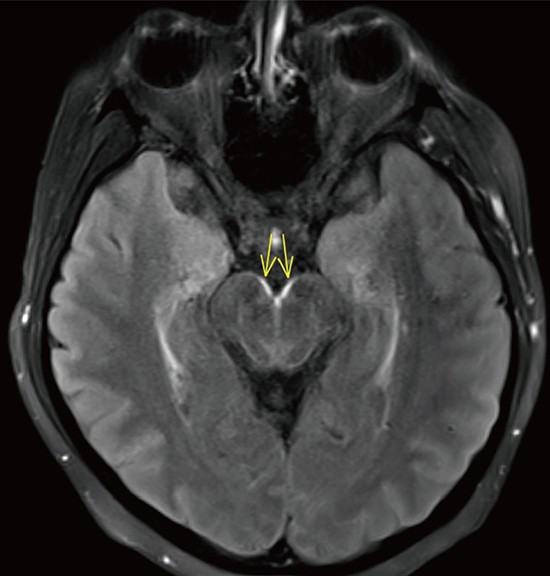
, leading to the withdrawal of methotrexate. Seven days later, appeared headaches, neck stiffness and urine retention. The cerebrospinal fluid (CSF) showed aseptic lymphocytic meningitis (protein 1.19 g/L, glucose 2.20 mM, lactate 2.24 mM, lymphocytes 150 /µL). Complete microbiological investigations in the blood and CSF, including quantiferon, herpes simplex, cytomegalovirus (CMV), Epstein-Barr virus (EBV), toxoplasma, borrelia, search for malignant cells, and lymphocytic count were negative. Implication of methotrexate was initially suspected, though recently stopped. An empirical treatment by doxycycline was initiated. Her condition worsened with the appearance of dizziness and rhombencephalitis with diplopia and bilateral palsy of the abducens nerve. Brain magnetic resonance imaging (MRI) was performed and showed an aspect of leptomeningitis surrounding the brainstem and the occipital lobes (
Fig. 1). In the presence of severe rhombencephalitis in a Turkish woman, in France for 4 years, tuberculous meningoencephalitis was suspected and a quadritherapy was started without waiting for the results of CSF mycobacterial culture. Despite this treatment, her neurological condition worsened, fever and biological inflammation persisted and inflammatory joint pain reappeared 2 weeks later. Behçet disease and mouth and genital ulcers with inflamed cartilage (MAGIC) syndrome were hypothesized but ruled out. Neurological involvement of RP with meningo-encephalitis was at that moment presumed, infliximab was initiated in association with methotrexate, with clinic and biological remission within 2 weeks. Control of the CSF fluid at one month was normal. To date, the disease is perfectly controlled.
This observation, even if the neurological manifestations were not present at diagnosis of RP as in the 2 cases reported in the article, shows the difficulties of differential diagnosis of meningoencephalitis in patients with RP. It demonstrates the importance to rule out at first all infectious causes (viral, bacterial, fungal, and parasitic) and eventual drugs adverse events. In our clinical case, Methotrexate toxicity, although rarely described in its sub cutaneous form was initially presumed responsible but rapidly eliminated (
3). After elimination of other infectious causes, in this immunodepression context tuberculosis was the most likely hypothesis to raise in the presence of a lymphocytic meningo-encephalitis in a Turkish woman and she indeed received a complete anti-tuberculosis therapy (
4). This treatment inefficiency, the exclusion of drug toxicity and the reoccurrence of articular inflammation strongly suggested to role of RP. Central nervous system (CNS) involvement in RP is a rare complication and treatment empirical. The effectiveness of anti-tumor necrosis factor (TNF) agents in these clinical presentation, such as infliximab in our case report, have been related in a few reports (
5).