Abstract
Gestational diabetes mellitus (GDM) is a strong predictor of postpartum prediabetes and transition to overt type 2 diabetes (T2DM). Although many reports indicate that low magnesium is correlated with deteriorated glucose tolerance, the association between postpartum serum magnesium level and the risk for T2DM in women with a history of GDM has not been evaluated. We analyzed postpartum serum magnesium levels and development of prediabetes and T2DM in women with prior GDM according to American Diabetes Association (ADA) criteria using the Korean National Diabetes Program (KNDP) GDM cohort. During a mean follow-up of 15.6±2.0 months after screening, 116 women were divided into three groups according to glucose tolerance status. Ultimately, eight patients (6.9%) were diagnosed with T2DM, 59 patients (50.9%) with prediabetes, and 49 patients (42.2%) with normal glucose tolerance (NGT) after follow-up. The T2DM group had the lowest serum magnesium level (0.65 [0.63-0.68] mM/L) in the postpartum period, but there was no significant difference between the prediabetes group (0.70 [0.65-0.70] mM/L) and the NGT group (0.70 [0.65-0.70] mM/L) (P=0.073) Multiple logistic regression analysis showed that postpartum HOMA-IR was a significant predictor of both prediabetes and T2DM. Moreover, we found that postpartum serum magnesium level was also a possible predictor for T2DM development. Serum magnesium level in the postpartum period may be a possible predictor for T2DM development in women with a history of GDM.
Gestational diabetes mellitus (GDM), defined as glucose intolerance during pregnancy, is a risk factor not only for adverse perinatal outcome, but also for postpartum prediabetes and development of type 2 diabetes mellitus (T2DM). The Diabetes Prevention Program study results showed that women with self-reported GDM and impaired glucose tolerance (IGT) had a 74% increased risk of developing T2DM compared to women with no GDM history and normal glucose tolerance (1).
GDM is similar to T2DM in terms of pathophysiology in that insulin resistance is a cardinal factor. Therefore, the pathophysiology of GDM plays an important role in the understanding of T2DM and the assessment of its risk factors. Until recently, obesity, sedentary life style and genetics were known risk factors for the development of type 2 diabetes. However, recent reports have revealed that there are many other possible risk factors, such as magnesium deficiency.
Magnesium is the fourth most abundant cation in the body and plays an important physiological role. It is a cofactor in enzymatic reactions involving energy metabolism and carbohydrate oxidation, as well as insulin secretion, receptor binding, and physiologic activity. Decreased blood and tissue levels of magnesium are related to the incidence of high blood pressure, kidney stones, heart disease, coronary artery spasms, systemic inflammation, insulin resistance, and T2DM (2-5).
Moreover, a previous report showed that a low serum magnesium level was a strong, independent predictor of incident type 2 diabetes in a cohort of non-diabetic middle-aged adults (6), and the Health Professionals Follow-up Study and the Nurses' Health Study also demonstrated that subjects in the highest quintile of oral magnesium intake had a lower risk of developing type 2 diabetes than those in the lowest quintile of magnesium intake (7).
Furthermore, a-10 yr follow-up study in Mexico also showed hypomagnesemia was independently associated with the development of abnormal glucose tolerance status including type 2 diabetes (8). And recently, Song et al. reported that magnesium intake from the diet is modestly and inversely associated with some, but not all, markers of systematic inflammation and endothelial dysfunction in apparently healthy women (9). Moreover, Federici et al. reported that not only the presence of type 2 diabetes, but also the degree of metabolic control in obese individuals who had undergone bariatric surgery were essential in accounting for the lower levels of serum magnesium (10). However, there is some controversy regarding whether magnesium supplementation could improve insulin sensitivity and metabolic control (11-13).
On this basis, we conducted a prospective cohort study to investigate postpartum serum magnesium level and the development of T2DM in women with a history of GDM.
The Korean National Diabetes Program (KNDP) study is an ongoing, multicenter, prospective cohort study investigating the course of T2DM and diabetic risk in patients who have been previously diagnosed with gestational diabetes mellitus (GDM) using the Carpenter and Coustan criteria. This cohort is composed of 13 KNDP-affiliated hospitals, as described previously (14).
Our study population was derived from the KNDP GDM cohort, which is followed annually at the Endocrinology Department of Cheil General Hospital after having been diagnosed by a universal two-step GDM screening program at 24-28 weeks of gestation. The first step was a 50-g glucose challenge test, and women with a positive result underwent a 3-hr 100-g oral glucose tolerance test (OGTT).
Women with GDM were advised to return to the hospital for a postpartum 75-g OGTT at 6-12 weeks after delivery. Routine annual follow-up was conducted with a 75-g OGTT and a metabolic assessment, including measurements of blood pressure, waist and hip circumferences, and biochemical assessments according to the KNDP GDM cohort protocol. The postpartum and follow-up 75-g OGTT results were interpreted using ADA criteria. We excluded patients with history of overt diabetes or type 1 diabetes. No participants had history of cardiovascular disease, stage 2 hypertension, malignancy, or severe renal or hepatic disease. As the exact time of diabetes onset was not ascertainable due to the irregularity of follow-up, the date of diagnosis was estimated as the date of the 75-g OGTT test.
Baseline anthropometric measurements, including pre-pregnancy weight and anthropometric measurements were recorded at the postpartum visit and every follow-up visit. The body mass index (BMI) of each study subject after pregnancy was calculated as weight/height2 (kg/m2), and waist circumference was also measured at the postpartum visit and follow-up visit using the midpoint between the lower border of the rib cage and the iliac crest.
All blood samples were drawn after a 12-hr overnight fast and were stored at -80℃ until analysis. The glucose oxidase method (YSI 2300-STAT; Yellow Springs Instrument Co., Yellow Springs, OH, USA) was used to determine plasma glucose, and a radioimmunoassay kit (Linco Research Inc, St. Louis, MO, USA) was used to measure insulin level. Insulin resistance was determined by HOMA-IR (Homeostasis model assessment=serum insulin [mU/L]×serum glucose [mM/L]/22.5]. Serum magnesium level was measured using the ADVIA 1650 chemistry system (Siemens, Tarrytown, NY, USA). The mean intra- and interassay coefficients of variation for serum magnesium were 2.8% and 4.2%, respectively.
Data are expressed as mean±SD, median (inter-quartile ranges), or percentage (%). Differences between groups were assessed using a one-way analysis of variance or the Kruskal-Wallis test for continuous variables. Tukey's multiple comparison test and the Wilcoxon rank-sum test were used for multiple comparisons. Bonferroni's correction was used to adjust for multiple comparisons.
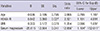
We used multiple logistic regression analysis to investigate the risk factors for T2DM and prediabetes. Variables with a P value<0.2 in the univariate analysis were selected for multiple logistic analysis. We estimated the odds ratio and 95% confidence interval when serum magnesium level was 0.1 mM/L decreased, because serum magnesium level was relatively small and very narrow range. We also excluded variables that correlated too highly with the other covariates. Data were analyzed using SPSS for Windows version 12.0 (SPSS Inc, Chicago, IL, USA). A P value<0.05 was considered statistically significant.
A total of 451 patients were enrolled in the KNDP gestational diabetes cohort between August 2005 and March 2010. Among these patients, 180 women were followed for more than one year. However, we regrettably did not have follow-up serum magnesium data for 62 women. Ultimately, 116 women had their serum magnesium status assessed in the postpartum period, and the prospective analysis was based on information from the first year after delivery.
Retrospectively, mean age at delivery was 33.9 yr, and the mean follow-up duration was 15.6±2.0 months. The mean postpartum serum magnesium level was 0.69 mM/L (reference range: 0.7-1.05 mM/L).
Table 1 shows that after follow-up, eight patients (6.9%) were diagnosed with T2DM; 59 patients (50.9%) with prediabetes, including impaired fasting glucose, impaired glucose tolerance, or both; and 49 patients (42.2%) with NGT using the ADA criteria (15). The T2DM group had the lowest serum magnesium level (0.65 [0.63-0.68] mM/L) at the postpartum visit, whereas the prediabetes group (0.70 [0.65-0.70] mM/L) and NGT group (0.70 [0.65-0.70] mM/L) were not significantly different (Fig. 1).
Multiple logistic regression analysis showed that postpartum HOMA-IR was a significant predictor of both prediabetes and T2DM (prediabetes, odds ratio [OR] 2.367, 95% confidence interval [CI] 1.348-4.155 (data not shown); T2DM, OR 2.321; 95% CI 1.101-4.891, Table 2). Moreover, we also founded that postpartum hypomagnesemia is a possible risk factor for T2DM since the corresponding odds ratio for a 0.1 mM/L decrease in the serum magnesium level was 12.956 (95% CI, 1.104-152.011).
This is the first study to demonstrate an association between postpartum serum magnesium level and development of T2DM. The results suggest that low postpartum serum magnesium is a potent risk factor for future T2DM.
Magnesium plays a key role in carbohydrate metabolism. Magnesium may influence the release and activity of hormones that help control blood glucose level via tyrosine kinase. Additionally, insulin partially regulates intracellular magnesium accumulation (16, 17). In humans, nearly all magnesium is supplied from vegetables, seafood, nuts, or seeds. However, meals high in protein or fat, a diet high in phosphorus or calcium or alcohol use may decrease magnesium absorption. In fact, the magnesium level in the human body is tightly regulated and depends on the balance between intestinal absorption and renal excretion. Therefore, in most normal adults, serum magnesium ranges from 0.70 to 1.10 mM/L. In Korea, there was a few report about magnesium status of normal population or pregnant women, Song et al. reported that the magnesium levels of these subjects including type 2 diabetes patients are 0.85±0.07 mM/L, respectively (18). However, the National Academy of Science and the Institute of Medicine have reported that an estimated 50%-85% of the US population has subclinical or severe magnesium deficiency (19).
Although extracellular magnesium accounts for 1% of total body magnesium, serum magnesium is considered a good indicator of magnesium deficiency. Therefore, most studies have analyzed magnesium status by magnesium intake until recently. Magnesium intake assessed by a food diary is associated with various disorders, such as insulin resistance, T2DM, atherosclerosis, hypertension, osteoporosis, and cancer (2, 20-22).
However, Lopez-Ridaura et al. (7) found that low blood level of magnesium is frequently observed in patients with T2DM and is associated with increased insulin resistance. In addition, serum magnesium is regarded as an additional risk factor for cardiovascular disease in type 2 diabetes and is also associated with both increased diabetic complications and all-cause mortality in type 2 diabetic patients (23, 24). Previous studies have reported that the first change appearing during experimentally-induced magnesium deficiency in humans and experimental animals is a decrease in serum magnesium concentration (25). Moreover, other researchers have reported that the serum magnesium concentration is sufficient to confirm a deficient status in the body (26, 27).
However, there are ongoing debates about whether magnesium supplementation has beneficial effects on metabolic parameters. Recent reports have shown that oral magnesium supplementation reduces insulin resistance even in non-diabetics (28), and improves borderline hypertension (29). Randomized controlled trials are warranted to provide additional evidence to settle this debate.
Gestational diabetes is a precursor of T2DM and prediabetes. Although magnesium deficiency in pregnant women is frequently observed due to inadequate or low magnesium intake, there are some disagreements about magnesium depletion in patients with gestational diabetes. Decreased serum magnesium is a known risk factor for intrauterine growth restriction (30), but no significant differences were observed in the fetal weights in our study. Meanwhile, our study showed that 1-min Apgar scores decreased slightly in the T2DM group (the lowest magnesium status group), but no significant relationship was observed between serum magnesium level and 1-min Apgar score by simple correlation analysis (r=0.101, P=0.328). In our study, serum magnesium level was obtained after delivery, and we did not observe a clear relationship between fetal weight and serum magnesium in this report.
This study showed that postpartum serum magnesium level influenced postpartum glucose tolerance and also demonstrated that the T2DM group with previous gestational diabetes had the lowest serum magnesium level in the postpartum period.
However, our study had some limitations. First, serum magnesium is influenced by creatinine clearance, but we could not estimate creatinine clearance because we did not measure serum creatinine during the postpartum period. Second, although this study was planned as a prospective design, the follow-up duration was relatively short, and the number of subjects was small. Third, dietary magnesium intake and supplementation of multi-vitamins and minerals were also important, but we did not include a food intake diary in this report. Fourth, it is not serum magnesium but intracellular magnesium that is an appropriate marker of magnesium status, and we could not evaluate intracellular magnesium status in this study. However, serum magnesium has been shown to be proportional to intracellular magnesium in many previous reports, and serum magnesium is an easily measured potential marker of intracellular magnesium status. Fifth, there were no data about preterm serum magnesium level. Maybe it brings about many confounding factor to our result, but lower serum magnesium level in preterm gestational women is known risk factor of preterm delivery. Our cohort data showed that birth weight of baby was within normal range, and serum magnesium level after delivery is within lower normal range.
In conclusion, low serum magnesium level was shown to be a potent risk factor for T2DM in patients with a history of gestational diabetes. This result is in agreement with those of several previous reports showing a relationship between serum magnesium level or magnesium intake and various inflammatory disorders, such as T2DM. The role of serum magnesium in the pathophysiology of T2DM and other chronic inflammatory disorders warrants further investigation.
Figures and Tables
Fig. 1
Postpartum serum magnesium level according to glucose tolerance statusduring the follow-up period (NGT, normal glucose tolerance; T2DM, type 2 diabetes mellitus).

Table 1
Clinical and laboratory characteristics of the study subjects after follow-up glucose tolerance status.

Data are presented as mean±SD or median (inter-quartile range). P values represent overall differences across groups as determined by one-way analysis of variance (ANOVA) or Kruskal-Wallis' H-test* for continuous variables. a,b,cSame letters indicate no statistical significance based on Tukey's post-hoc analysis or Wilcoxon's rank-sum test. SBP, systolic blood pressure; DBP, diastolic blood pressure; HOMA-IR, homeostasis model assessment insulin resistance.
Notes
References
1. Ratner RE, Christophi CA, Metzger BE, Dabelea D, Bennett PH, Pi-Sunyer X, Fowler S, Kahn SE. Diabetes Prevention Program Research Group. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab. 2008; 93:4774–4779.
2. Kim DJ, Xun P, Liu K, Loria C, Yokota K, Jacobs DR Jr, He K. Magnesium intake in relation to systemic inflammation, insulin resistance, and the incidence of diabetes. Diabetes Care. 2010; 33:2604–2610.
3. Song Y, Li TY, van Dam RM, Manson JE, Hu FB. Magnesium intake and plasma concentrations of markers of systemic inflammation and endothelial dysfunction in women. Am J Clin Nutr. 2007; 85:1068–1074.
4. He K, Liu K, Daviglus ML, Morris SJ, Loria CM, Van Horn L, Jacobs DR Jr, Savage PJ. Magnesium intake and incidence of metabolic syndrome among young adults. Circulation. 2006; 113:1675–1682.
5. Jaipakdee S, Prasongwatana V, Premgamone A, Reungjui S, Tosukhowong P, Tungsanga K, Suwantrai S, Noppawinyoowong C, Maskasame S, Sriboonlue P. The effects of potassium and magnesium supplementations on urinary risk factors of renal stone patients. J Med Assoc Thai. 2004; 87:255–263.
6. Kao WH, Folsom AR, Nieto FJ, Mo JP, Watson RL, Brancati FL. Serum and dietary magnesium and the risk for type 2 diabetes mellitus: the Atherosclerosis Risk in Communities Study. Arch Intern Med. 1999; 159:2151–2159.
7. Lopez-Ridaura R, Willett WC, Rimm EB, Liu S, Stampfer MJ, Manson JE, Hu FB. Magnesium intake and risk of type 2 diabetes in men and women. Diabetes Care. 2004; 27:134–140.
8. Guerrero-Romero F, Rascón-Pacheco RA, Rodríguez-Morán M, de la Peña JE, Wacher N. Hypomagnesaemia and risk for metabolic glucose disorders: a 10-year follow-up study. Eur J Clin Invest. 2008; 38:389–396.
9. Song Y, Manson JE, Buring JE, Liu S. Dietary magnesium intake in relation to plasma insulin levels and risk of type 2 diabetes in women. Diabetes Care. 2004; 27:59–65.
10. Lecube A, Baena-Fustegueras JA, Fort JM, Pelegrí D, Hernández C, Simó R. Diabetes is the main factor accounting for hypomagnesemia in obese subjects. PLoS One. 2012; 7:e30599.
11. Rodríguez-Morán M, Guerrero-Romero F. Oral magnesium supplementation improves insulin sensitivity and metabolic control in type 2 diabetic subjects: a randomized double-blind controlled trial. Diabetes Care. 2003; 26:1147–1152.
12. Eibl NL, Kopp HP, Nowak HR, Schnack CJ, Hopmeier PG, Schernthaner G. Hypomagnesemia in type II diabetes: effect of a 3-month replacement therapy. Diabetes Care. 1995; 18:188–192.
13. Paolisso G, Sgambato S, Gambardella A, Pizza G, Tesauro P, Varricchio M, D'Onofrio F. Daily magnesium supplements improve glucose handling in elderly subjects. Am J Clin Nutr. 1992; 55:1161–1167.
14. Rhee SY, Chon S, Kwon MK, Park IeB, Ahn KJ, Kim IJ, Kim SH, Lee HW, Koh KS, Kim DM, et al. Prevalence of chronic complications in Korean patients with type 2 diabetes mellitus based on the Korean national diabetes program. Diabetes Metab J. 2011; 35:504–512.
15. American Diabetes Association. Standards of medical care in diabetes: 2011. Diabetes Care. 2011; 34:S11–S61.
16. Paolisso G, Scheen A, D'Onofrio F, Lefèbvre P. Magnesium and glucose homeostasis. Diabetologia. 1990; 33:511–514.
17. Takaya J, Higashino H, Kobayashi Y. Intracellular magnesium and insulin resistance. Magnes Res. 2004; 17:126–136.
18. Song CH, Song IK, Ju SY, Ock SM. Serum magnesium level is negatively associated with fasting serum glucose level in Korean adults. Biol Trace Elem Res. 2011; 143:612–618.
19. Chaudhary DP, Sharma R, Bansal DD. Implications of magnesium deficiency in type 2 diabetes: a review. Biol Trace Elem Res. 2010; 134:119–129.
20. Weinert LS. International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy: comment to the International Association of Diabetes and Pregnancy Study Groups Consensus Panel. Diabetes Care. 2010; 33:e97.
21. Sales CH, Pedrosa LF, Lima JG, Lemos TM, Colli C. Influence of magnesium status and magnesium intake on the blood glucose control in patients with type 2 diabetes. Clin Nutr. 2011; 30:359–364.
22. Shils ME. Experimental human magnesium depletion. Medicine (Baltimore). 1969; 48:61–85.
23. Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR, Hadden DR, McCance DR, Hod M, McIntyre HD, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008; 358:1991–2002.
24. Pham PC, Pham PM, Pham PA, Pham SV, Pham HV, Miller JM, Yanagawa N, Pham PT. Lower serum magnesium levels are associated with more rapid decline of renal function in patients with diabetes mellitus type 2. Clin Nephrol. 2005; 63:429–436.
25. Håglin L, Törnkvist B, Bäckman L. Prediction of all-cause mortality in a patient population with hypertension and type 2 DM by using traditional risk factors and serum-phosphate,-calcium and-magnesium. Acta Diabetol. 2007; 44:138–143.
26. Dunn MJ, Walser M. Magnesium depletion in normal man. Metabolism. 1966; 15:884–895.
27. Alfrey AC, Miller NL, Butkus D. Evaluation of body magnesium stores. J Lab Clin Med. 1974; 84:153–162.
28. Pham PC, Pham PM, Pham SV, Miller JM, Pham PT. Hypomagnesemia in patients with type 2 diabetes. Clin J Am Soc Nephrol. 2007; 2:366–373.
29. Mooren FC, Krüger K, Völker K, Golf SW, Wadepuhl M, Kraus A. Oral magnesium supplementation reduces insulin resistance in non-diabetic subjects - a double-blind, placebo-controlled, randomized trial. Diabetes Obes Metab. 2011; 13:281–284.
30. Kisters K. Oral magnesium supplementation improves borderline hypertension. Magnes Res. 2011; 24:17.
31. Takaya J, Yamato F, Kaneko K. Possible relationship between low birth weight and magnesium status: from the standpoint of "fetal origin" hypothesis. Magnes Res. 2006; 19:63–69.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download