Abstract
This study estimates the treated prevalence of schizophrenia and the annual costs associated with the illness in Korea in 2005, from a societal perspective. Annual direct healthcare costs associated with schizophrenia were estimated from National Health Insurance and Medical Aid records. Annual direct non-healthcare costs were estimated for incarceration, transport, community mental health centers, and institutions related to schizophrenia. Annual indirect costs were estimated for the following components of productivity loss due to illness: unemployment, reduced productivity, premature mortality, and caregivers' productivity loss using a human capital approach based on market wages. All costs were adjusted to 2005 levels using the healthcare component of the Consumer Price Index. The treated prevalence of schizophrenia in 2005 was 0.4% of the Korean population. The overall cost of schizophrenia was estimated to be $ 3,174.8 million (3,251.0 billion Won), which included a direct healthcare cost of $ 418.7 million (428.6 billion Won). Total direct non-healthcare costs were estimated to be $ 121 million (123.9 billion Won), and total indirect costs were estimated at $ 2,635.1 million (2,698.3 billion Won). Unemployment was identified as the largest component of overall cost. These findings demonstrate that schizophrenia is not rare, and that represents a substantial economic burden.
Schizophrenia is not an uncommon disease. According to World Health Organization (WHO), approximately 29 million people suffer from the disease worldwide (1). Moreover, it has been reported that schizophrenia affects 0.7% of the U.S. population (2), and that the lifetime prevalence of schizophrenia in Korea is 0.28% (3).
Schizophrenia is a chronic, debilitating condition with a lower mortality than many other chronic illnesses. However, it has been reported that schizophrenia is a costly disease (4, 5), and that costs associated with productivity losses are probably the largest component of the overall societal cost of schizophrenia (4). Therefore, the adequate distribution of medical resources and the establishment of proper healthcare policies are crucially required to effectively manage this illness. For this reason, it is critical that the economic burden of schizophrenia can be measured from a societal perspective.
Only one Korean study has reported that schizophrenia is a relatively costly illness, as compared with coronary heart disease, but this study was limited to outpatients at one hospital (6). The costs of schizophrenia have never been estimated in Korea from a societal perspective, and therefore, a comprehensive estimate of the costs associated with this disease was required to ensure the efficient and systematic delivery of an appropriate mental health service.
The aims of this study were to estimate the prevalence of treated schizophrenia in Korea in 2005 and to determine the direct and indirect costs associated with the disease.
Estimates of total societal costs were based on treated prevalence. Initially, the treated prevalence rate of schizophrenia in 2005 was estimated based on information from the "Statistical Information System of National Health Insurance" (7), the "National Health Insurance Statistical Yearbook" (8), and the "Medical Aid Statistical Yearbook" (9). Information on the 2005 general population was obtained from the Korean National Statistical Office (10). The Korean Medical Security system consists of National Health Insurance and Medical Aid. The majority of Koreans are beneficiaries of National Health Insurance, and people at the lowest income level are provided with free Medical Aid. Thus, we were able to analyze every case of schizophrenia treated in Korea.
Estimations of the costs of schizophrenia vary between countries due to different healthcare systems, but the commonly accepted definitions of costs related to illness are as follows. Cost-of-illness (COI) studies identify two main categories of cost: 1) direct costs, for which payments are made, and 2) indirect costs, for which resources are lost (5).
In the present study, we used various data sources, including published scientific literature and government reports and documents to estimate the economic burden of schizophrenia. The focus of our literature review was on Korean data sources, especially on government reports. When Korean data sources were not available, data from COI studies on schizophrenia in other countries were used. However, this was limited to data about the prevalence rate of schizophrenia among all suicide victims.
Where possible, all resource utilization estimates were obtained for 2005, and these were expressed in 2005 U.S. dollars (average exchange rate 1 U.S. Dollar=1,024 Korean Won as of 2005, Korean Exchanging Bank). When costs were unavailable for 2005, the healthcare component of the Korean Consumer Price Index (CPI) was used to adjust costs to 2005 values (10).
Costs included in this analysis were; direct healthcare costs, direct non-healthcare costs, and the indirect costs associated with productivity losses. The methods used to determine costs in each category are described below.
Patients included in our analyses were defined as those with an F20 diagnosis (ICD-10 diagnosis code). We obtained details on overall healthcare utilization in Korea from the previously mentioned database and Yearbooks (7-9), which also contained information on total numbers of outpatients and inpatients, and the cost of total visits and total admissions. Total outpatient cost-National Health Insurance and Medical Aid-was divided by the number of patients to determine per-person outpatient cost, and the same procedure was followed for inpatients.
We defined direct non-healthcare costs as costs related to patient management, excluding medical care costs. Direct non-healthcare costs were estimated for the criminal justice system, community mental healthcare centers, sanatoria, rehabilitation facilities, homeless shelters, and transport costs related to schizophrenia.
The crime rate among persons with severe mental illness is higher than in the general population (11). Cost estimates relating to the criminal justice system were mainly incarceration costs related to schizophrenia. Costs associated with crime are debatable, because policing, investigations, legal defense, and prosecution costs could all arguably be included in calculations of the economic burden of schizophrenia. However, there were no data on these detailed contents. In the present analysis, we focused on areas with available definitive data, such as the cost of incarceration. The Korean government has operated a cure-custody system since 1980, and the Institute of Forensic Psychiatry Ministry of Justice is responsible for providing mentally disordered offenders with treatment in custody. We calculated incarceration costs associated with schizophrenia using estimates supplied by the annual budget of the Institute of Forensic Psychiatry Ministry of Justice (12) and the incarceration rate. A recent study by the Institute of Forensic Psychiatry Ministry of Justice reported that persons with schizophrenia accounted for 55% of incarcerated offenders (13).
In 2005, there were 127 community mental health centers, which provided mentally ill patients in communities with mental health programs. Annual budgets, operating programs, and schizophrenia registration rates were available from the government report, "2005 The Central Mental Health Supporting Committee Report" (14). This report also contains comprehensive information about sanatoria and rehabilitation facilities. Annual operating cost and percentage of schizophrenia according to institution type were also obtained from this report.
In 2005, there were 38 homeless shelters nationwide that admitted mentally ill patients. Nine thousands and fifty five persons were registered at homeless shelters in 2005 (15), and of these 62% were diagnosed as having schizophrenia (3). The majority of these homeless shelters were administered by the private sector. Thus, we were unable to obtain the total annual operation costs associated with schizophrenia at homeless shelters due to limited accessibility to private data. Therefore, to estimate the cost related to schizophrenia in homeless shelters, we use the standardized operation fee model proposed by the Korean Institute of Health and Social Affairs (KIHASA) (16), which suggested that an average of $3,500 per person per annum is required to maintain a homeless shelter.
Transport costs were estimated by multiplying the number of total visits to outpatient clinics by the mean return fare, and it has been reported that the mean return fare per visit is $5.5 (6).
Productivity losses caused by schizophrenia can be divided into productivity losses associated with morbidity and those associated with premature mortality. Schizophrenia morbidity increases unemployment and reduces productivity. Morbidity costs also include productivity losses by patients and their caregivers due to illness. Mortality costs were defined as the product of the number of deaths due to schizophrenia and the discounted value of average expected future earnings.
Thus, indirect annual costs resulting from schizophrenia were estimated separately for four distinct components of productivity loss: 1) increased unemployment; 2) reduced workplace productivity due to morbidity; 3) premature mortality resulting from schizophrenia; and 4) care-giving time required of family member. Indirect costs due to schizophrenia were estimated using a human capital method, i.e., by multiplying the expected mean earnings of an individual without illness by time lost at work. The equations used to estimate indirect costs are presented in Appendix 1.
First, a review of published studies determined that the estimated employment-to-population rate of schizophrenia was 18.8% (from 15.9% to 21.7%) in Korea (6, 17, 18). This rate was lower than the employment-to-population rate for the general population in 2005 (59.7%) (10). The resultant productivity loss due to unemployment was estimated as lost earnings due to morbidity in the schizophrenia population using the mean annual wage for 2005, as reported by the Korean Ministry of Labor for the employed population (19).
Second, employed persons with schizophrenia have reduced productivity resulting from disability due to illness. Productivity reductions were estimated from average earnings in the general population and productivity reduction ratios. Productivity reduction ratios were calculated by subtracting population-to-patient earning ratios from '1'. The average income of employed persons with schizophrenia is about 40% (range from 30% to 50%) of that of the general population in Korea (6, 18).
Third, the present value of lost earnings due to premature mortality (20) was calculated from deaths attributable to schizophrenia and annual earnings, data for these calculations were obtained from the National Mortality Statistics (10) and the Ministry of Labor (19). Only persons with schizophrenia who died when less than 65 yr old were included in this analysis, although this figure is lower than the recognized retirement age in South Korea, it was intentionally adopted in order to ensure that the study results were conservative. The average retirement age was 68.2 for men and 66.9 for women in 2004 (Korea Labor Institute). Expected future earnings lost due to premature mortality among persons with schizophrenia were adjusted to 2005 values using a 3% discount rate. Information on numbers of deaths due to schizophrenia or suicides per year in Korea was obtained from National Mortality Statistics. However, suicide is the most common cause of premature deaths in schizophrenia (17). Therefore, the cause of death from schizophrenia in National Mortality Statistics can underestimate the total number of deaths from schizophrenia, because a proportion of deaths coded as 'suicide' can result from schizophrenia. A review of the literature suggested that the prevalence of schizophrenia among suicide victims ranged from 2% to 12% (21). For this study, we assumed that 7% of all Korean suicides were attributable to schizophrenia. To estimate productivity losses associated with premature mortality, we combined estimates of mortality due to schizophrenia by age and gender with estimates of labor force income data for those employed.
Finally, the costs of caregiver productivity losses were estimated using family member's productivity loss and the mean monthly wages of employed individuals in 2005 (19). It was reported that 24.9% of schizophrenia patients with disability (estimated as 24,015 in 2005) interfere with the earning capacity of caregivers on a daily basis (18), and therefore estimated that the number of such schizophrenia patients was 5,980/day in 2005.
In the present study, a human capital method was used to estimate indirect societal costs associated with unemployment and reduced productivity. Some patients with schizophrenia are provided with disability payments and other forms of governmental support, and although these payments are made as a result of schizophrenia morbidity, they do not reflect true societal costs because these resources simply represent transfers from some members of society to others (i.e., transfer payments) (4, 22). In the present study, indirect schizophrenia costs were estimated based on the standpoint 'of likely earnings in the absence of illness'. Thus, governmental support costs were excluded from our indirect cost calculations.
Although resource utilizations and unit cost information were obtained directly from National Health Insurance records, direct healthcare costs are also influenced by self-payments made due to Health Insurance exclusions, and average exclusion payments ranged from 11% to 20% (23). To assess the robustness of cost estimates made during this analysis, sensitivity analyses were conducted. Cost estimates were set at the lowest and highest levels reported in the literature, respectively, whilst other parameters were held constant. Productivity loss estimates were based upon literature estimates, and these rates and costs were also subjected to sensitivity analysis. More specifically, we evaluated the sensitivity of schizophrenia total cost estimates with respect to exclusion payment rates (11% and 20%), alternative discount rates (0% and 5%) of expected future earning, schizophrenia employment rates (15% and 22%), productivity reduction ratios (0.5 and 0.7), and prevalence of schizophrenia among all suicides (2% and 12%).
Most of COI studies associated with schizophrenia were based on human capital approach (5). A different perspective on mortality cost estimates is offered by Goeree et al. (20), who used the friction cost method instead of using human capital approach. We also estimated the productivity costs associated with schizophrenia premature mortality by using the friction cost method. Sensitivity analysis was conducted on friction periods required for worker replacement.
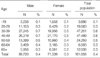
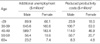
The treated prevalence rate of schizophrenia in the Korean population in 2005 was 0.4% (Table 1). The number of persons treated with schizophrenia in 2005 was 161,058 (89,720 men and 71,339 women). Table 1 also shows treated prevalence rates of schizophrenia among the total population in 2005 by gender and age group.
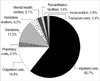
Fig. 1 presents individual direct costs as a percentage of total direct cost.
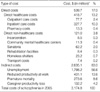
The total direct health care cost for individuals with schizophrenia in 2005 was estimated to be $418.7 million (428.7 billion Won), or 13.2% of the total costs associated with schizophrenia. Table 3 shows the proportions of direct health care costs attributable to inpatient and outpatient care based on information provided by Medical Security Systems. Patient-level costs for individuals that received National Health Insurance and Medical Aid are also presented in Table 3.
The average length of stay for patients with schizophrenia enrolled with National Health Insurance was 99 days and for Medical Aid patients this was 234 days. In terms of all inpatients regardless of disease entity in 2005, average length of stay was 14 days (Health Insurance) and 71 days (Medical Aid). Total annual national health care expenditure on medical care in Korea in 2005 was U.S. $25.8 billion (43.0% on outpatient care, and 30.4% on inpatient care). The direct health care costs of schizophrenia accounted for 1.6% of national health care expenditure in 2005, and the inpatient care cost of schizophrenia contributed 78.3% to the direct health care costs of schizophrenia.
Direct non-healthcare costs were estimated to be $121.0 million (123.9 billion Won) in 2005 for schizophrenia-related incarceration, community mental health centers, institutions, and transport (Table 2). These costs represent 3.8% of the total costs associated with schizophrenia. Schizophrenia-related incarceration contributed $8.5 million (8.7 billion Won) to the total annual cost of schizophrenia. The institutions that deal with schizophrenics, i.e., sanatoria, rehabilitation facilities and homeless shelters, contributed $93.8 million (96.0 billion Won) to the annual cost imposed by the disease. Transport cost for visits to outpatient departments contributed $7.4 million (7.6 billion Won) to the annual cost of schizophrenia.
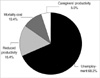
Fig. 2 shows individual indirect costs as a percentage of total indirect costs.
Assuming a mean employment rate of persons with schizophrenia of 18.8%, additional productivity losses due to unemployment were calculated and results are presented in Table 4. Overall increased unemployment due to schizophrenia resulted in a cost of $1,798.2 million (1,841.4 billion Won), and this was the largest contributor to total indirect costs. In terms of employed schizophrenia, the productivity reduction ratio was calculated to be '0.6', and thus, reduced productivity at work cost $431.1 million (441.4 billion Won) (Table 4).
The number of deaths in 2005 listed as being due to schizophrenia and the numbers of suicides attributed to schizophrenia are presented in Table 5. The 138 deaths were listed as being due to schizophrenia (78 males and 60 females), and 840 suicides were attributed to schizophrenia (562 males and 278 females). Thus, the total estimated number of deaths due to schizophrenia in 2005 was 978, of which 640 were males and 338 were females. Additionally costs due to premature mortality were estimated at $273.6 million (280.2 billion Won) (estimated by applying a 3% discount rate).
Concerning schizophrenia patients with disabilities, average 5,980 schizophrenics per day required cares from their family members to the extent that these interfered with caregivers' earnings. Patients admitted by institutions were not included in this estimate. The total cost associated with caregiver productivity losses was $132.2 million (135.4 billion Won).
Base case COI estimates and the results of selected sensitivity analyses are presented in Table 6. Assuming that additional self-payments due to exclusion from National Health Insurance contribute to direct health care costs, total cost estimates, including self-payment rates, were $3,370.3 and 3,386.1 million when additional self-payment rates were assumed to be 11% and 20%, respectively. The results according to varying unemployment rate assumptions for schizophrenia showed that the results were $3,309.8 million (employment rate 15%) and $3,061.8 million (employment rate 22%). The use of a 0% discount rate increased total schizophrenia cost to $3,290.8 million, and a 5% discount rate reduced this to $3,126.8 million. When a 0.5 productivity reduction ratio was used, total schizophrenia cost reduced to $3,101.8 million, and for a ratio of 0.7 total cost increased to $3,248.8 million. We varied the schizophrenia prevalence rate in all suicides using the range from 2% to 12%. Application of the lower (2%) and upper bound (12%) values in this analysis resulted in total schizophrenia cost of $3,001.1 million and $3,348.8 million, respectively. Finally, assuming a 1- or 6-month friction period for worker replacement, the productivity costs associated with premature death were estimated at $0.8 million and $4.7 million, respectively. Therefore, the total schizophrenia cost was estimated at $2,902.0 (1-month friction period) and $2,905.9 million (6-month friction period).
Schizophrenia follows a chronic debilitating course, and thus, its costs tend to persist. Estimated prevalences of schizophrenia vary by country and time, and it has been estimated that the lifetime prevalence rate of schizophrenia lies between 0.4% and 0.7% (2, 24). According to the 2001 Korean Epidemiologic Catchment Area (KECA) Study, the one year prevalence rate of schizophrenia among community resident adults aged 18-64 yr is 0.16% (25), and when persons living in institutions were included, the one year prevalence rate increased to 0.28% (3). In the present study, the treated prevalence rate of schizophrenia was 0.4%, which was found to be higher than the prevalence rates in the previous epidemiologic studies in Korea. Our estimation of the prevalence of schizophrenia was based on claims data (7-9), which are supported by diagnoses made by psychiatrists. This observed difference in the prevalence of schizophrenia supports the notion that clinical interviews by clinicians are more useful than structured interviews by trained laymen (2, 24). It also indicates that the Composite International Diagnostic Interview (CIDI) is not sensitive enough to estimate the prevalence of psychotic disorders (25), and that a clinical reinterview is required for all epidemiologic survey respondents suspected of having psychotic symptoms (26).
The costs of schizophrenia have been estimated in a number of countries (27), e.g., Australia, Belgium, Canada, Denmark, France, Germany, Italy, Norway, Puerto Rico, Spain, Sweden, Taiwan, the United Kingdom, and the United States. However, no previous study has estimated the economic burden of schizophrenia in Korea. Therefore, we compared out results with those published in other countries. Despite differences in data sources and costing methodologies, the impact of schizophrenia on health care expenditure is universally substantial. Moreover, direct cost estimates of schizophrenia across countries are remarkably similar, and range from 1.5% to 3% of national healthcare expenditure (5, 22). Our study shows that direct healthcare costs accounted for around 1.6% of total health care expenditure in Korea, which compares favorably to cost estimates made in other countries.
Inpatient care is the single largest contributor to the direct healthcare costs of schizophrenia. In terms of cross-national comparisons, inpatient care costs account for the largest proportion of direct healthcare costs in most countries. The proportion of cost attributed to inpatient care varies between countries, as it is a function of individual mental health delivery systems. Generally between 33% and 66% of total healthcare costs for schizophrenia are for inpatient care, even in countries that have already substantially reduced their inpatient provisions (5). In the present study, it was found that inpatient care costs associated with schizophrenia accounted for 78.3% of the total health care costs for schizophrenia in Korea, which is higher than has been reported in other countries. This level of inpatient care cost is also higher than the 30.4% of total national healthcare costs spent on inpatients in Korea.
Average length of stay of schizophrenia was longer than other diseases. In Korea the number of psychiatric beds has continuously increased from the 1980's; in fact this rate of increase is higher than in any other OECD member nation (14). It is problematic that schizophrenia patients are still predominantly treated by hospitalization in Korea, and that mean length of stay is greater than in other countries (14, 28-30).
The costs associated with psychosocial rehabilitation like community mental healthcare centers and rehabilitation facilities are 0.7%, which was much lower than the other costs of schizophrenia.
These findings - inpatient oriented treatment, long length of stay, poor psychosocial treatment - indicate that more attention should be paid to activities like de-institutionalization, community-based mental healthcare, and psychosocial rehabilitation. Moreover, psychosocial rehabilitation in community will decrease the productivity loss due to schizophrenia.
Studies on schizophrenia costs vary considerably in terms of productivity cost estimates, especially with respect to indirect costs (4, 5, 22). These differences are largely due to the inclusion, or not, of premature mortality and morbidity productivity estimates in cost calculations, and whether productivity was determined using the human capital approach or the friction cost method (20), the latter of which allows for the possibility of worker replacement (the number of days necessary to fill the vacant position).
The majority of studies that have addressed the costs associated with productivity losses and indirect costs have reported that productivity losses outweigh direct healthcare costs (4, 5, 22), whereas a smaller number of studies have concluded to the contrary (5). However, most studies have found that productivity losses are 2.0 times higher (ranging from one to seven times higher) than direct health care costs. According to our cost estimates, indirect costs are 4.8 times larger than direct costs. Unemployment was found to be the largest contributor to the costs related to schizophrenia, which is a reflection of the fact that schizophrenia morbidity is associated with a continued inability to work. Caregivers' productivity losses contributed least to indirect costs in the present study, which is unlike that found by other studies (4, 5). Schizophrenia patients under inpatient care were excluded from the caregivers' productivity loss estimate. Therefore, our findings suggest that the relatively low number of caregivers were interfered with their productivity losses due to high proportion of inpatient care in Korea.
Some factors may have resulted in under-estimations during our analysis of COI. First, we did not include costs associated with distress, pain, and an impoverished quality of life, which are not measurable. Second, we did not include cost estimates for over-the-counter or herbal medications. Third, we did not include cost estimates for outpatient waiting time, and time spent visiting hospitals.
In summary, the treated prevalence rate of schizophrenia in Korea in 2005 was 0.4%. Using this prevalence-based COI estimate, the cost of schizophrenia in Korea in 2005 was estimated to be $3,174.8 million, and of this, $539.7 million was accounted for by healthcare and non-healthcare costs, and $2,635.1 million by productivity losses related to morbidity, premature mortality, and caregivers' productivity losses. Inpatient care was found to be the single largest contributor to direct healthcare costs, whereas psychosocial rehabilitation costs were found to be too low. The greatest contributor to the cost of schizophrenia in Korea was identified as a high level of unemployment. These findings indicate that more action must be taken to de-institutionalize mental healthcare, and that programs should be targeted at improving psychosocial rehabilitation.
Figures and Tables
References
1. Mental and neurological disorders. Fact sheet no. 265. 199. World Health Organization;Available from:
http://www.who.int/whr/2001/media_centre/en/whr01_fact_sheet1_en.pdf.
2. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994. 51:8–19.
3. Cho SJ, Cho MJ, Suh T, Hahm BJ, Hong JP, Bae JN, Lee JY, Lee DW, Park JI, Jeon HJ, Kim SJ, Kim YI. Prevalence rates of major mental disorders in mental health related facilities: nationwide 20 institutions study. J Korean Neuropsychiatr Assoc. 2004. 43:749–759.
4. Wu EQ, Birnbaum HG, Shi L, Ball DE, Kessler RC, Moulis M, Aggarwal J. The economic burden of schizophrenia in the United States in 2002. J Clin Psychiatry. 2005. 66:1122–1129.
5. Knapp M, Mangalore R, Simon J. The global costs of schizophrenia. Schizophr Bull. 2004. 30:279–293.

6. Park JI, Song SH, Suh Tw, Jang HJ, Lee JG, Chang AK, Kim Y, Lee C, Hong JP. Direct and indirect cost of treating out-patients with schizophrenia in Korea. J Korean Neuropsychiatr Assoc. 2000. 39:580–588.

7. Statistical Information System. National Health Insurance Corporation 2007 April cited. National Health Insurance Corporation;Available from:
http://www.nhic.or.kr/wbm/wbmb/wbmb_1000_f.jsp
.
8. Health Insurance Review Agency, National Health Insurance Corporation. 2005 National Health Insurance Statistical Yearbook. Seoul, Korea: Health Insurance Review Agency and National Health Insurance Corporation 2006.
9. Ministry of Health and Welfare, National Health Insurance Corporation. 2005 Medical Aid statistical Yearbook. Seoul Korea: Ministry of Health and welfare and National Health Insurance Corporation 2006.
10. Korean Statistical Information System. Korean National Stastical Office 2007 April cited. Korean National Statistical Office;Available from:
http://kosis.nso.go.kr/
.
11. Bonta J, Law M, Hanson K. The prediction of criminal and violent recidivism among mentally disordered offenders: a meta-analysis. Psychol Bull. 1998. 123:123–142.
12. National Budget and Settlement of Accounts Information System. The National Assembly of the Republic of Korea 2007 April cited. The National Assembly of the Republic of Korea;Available from:
http://nafs.assembly.go.kr:83/
.

13. Jeong PJ. A study on the cure-custody system for mentally disordered offenders. 2004. Kongju: Kongju National University.
14. Suh TW, Cho MJ, Kim JH, Kwak YS, Kim KK, Bae A, Kim DH. 2005 The Central Mental Health Supporting Committee Report. Ministry of Health and Welfare, Korean Institute for Health and Social Affairs, Central Mental Health Supporting Committee 2006.
15. Statistical Data; statistics of homeless shelter Ministry of Health and Welfare. 2007 April cited. Ministry of Health and Welfare;Available from:
http://www.mohw.go.kr/
.
16. Kim MS. Development of a standardized operation fee model for social welfare facilities. Health and welfare policy forum. 2003. 84:88–101.
17. Hong JP, Kim CY. Course and Outcome of Schizophrenia. Korean J Psychopathol. 1999. 8:140–150.
18. Ministry of Health and Welfare, Korea Institute for Health and Social Affairs. 2005 Survey report on the disabled. 2006. Ministry of Health and Welfare, Korea Institute for Health and Social Affairs.
19. 2005 Survey Report on Wage Structure. Ministry of Labor 2007 April cited. Labor Statistics of Korea;Available from:
http://laborstat.molab.go.kr
.
20. Goeree R, O'Brien BJ, Blackhouse G, Agro K, Goering P. The valuation of productivity costs due to premature mortality: a comparison of the human-capital and friction-cost methods for schizophrenia. Can J Psychiatry. 1999. 44:455–63.
21. Goeree R, Farahati F, Burke N, Blackhouse G, O'Reilly D, Pyne J, Tarride JE. The Economic Burden of Schizophrenia in Canada in 2004. Curr Med Res Opin. 2005. 21:2017–2028.

21. Murray RM, Jones PB, Susser E, Van Os J, Cannon M. The epidemiology of schizophrenia. 2003. New York: Cambridge University Press.

22. Goeree R, Farahati F, Burke N, Blackhouse G, O'Reilly D, Pyne J, Tarride JE. The economic burden of schizophrenia in Canada in 2004. Curr Med Res Opin. 2005. 21:2017–28.

23. Jeong HS. Public financing in total health expenditure and coverage by National Health Insurance in Korea: including comparison with other OECD countries. Korean J Health Economics Policy. 2004. 10:95.
24. Bijl RV, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS). Soc Psychiatry Psychiatr Epidemiol. 1998. 33:587–595.

25. Cho MJ, Kim JK, Jeon HJ, Suh T, Chung IW, Hong JP, Bae JN, Lee DW, Park JI, Cho SJ, Lee CK, Hahm BJ. Lifetime and 12-month prevalence of DSM-IV psychiatric disorders among Korean adults. J Nerv Ment Dis. 2007. 195:203–210.

27. Knapp M, Chisholm D, Leese M, Amaddeo F, Tansella M, Schene A, Thornicroft G, Vazquez-Barquero JL, Knudsen HC, Becker T. Comparing patterns and costs of schizophrenia care in five European countries: the EPSILON study. European Psychiatric Services: Inputs Linked to Outcome Domains and Needs. Acta Psychiatr Scand. 2002. 105:42–54.
28. DeFrances CJ, Hall MJ, Podgornik MN. Advance data from vital and health statistics; no 359. 2005, 2003. Hyattsville, MD: National Center for Health Statistics.
29. Australian Institute of Health and Welfare (AIHW). Australian hospital statistics 2001-02. 2003. Canberra: AIHW;Health Services Series no. 20. AIHW cat. no. HSE 25.
30. Department of Health. Hospital Episode Statistics, Department of Health, England, 2002-03.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download