Abstract
To determine the effects of excessive drinking and alcohol dependency on mortality and chronic health problems in a rural community in South Korea, this study represents a nested case-control study. In 1998, we conducted the Alcohol Dependence Survey (ADS), a population survey of a village in Korea. To measure the effects of alcohol on chronic health conditions and mortality over time, in 2004, we identified 290 adults from the ADS sample (N=1,058) for follow-up. Of those selected, 145 were adults who had alcohol problems, either alcohol dependence as assessed in the ADS by the Severity of Alcohol Dependence Questionnaire (N=59), or excessive drinking without dependency (N=86). Further 145 nondrinkers were identified, matching those with alcohol problems in age and sex. We revisited the village in 2004 and completed personal interviews with them. In multivariate logistic regressions, the rates of mortality and morbidity of chronic health conditions were three times greater for alcohol dependents compared with the rate for nondrinkers. Importantly, however, excessive drinking without dependency was not associated with the rates of either mortality or morbidity. Future investigations would benefit by attending more specifically to measures for alcohol dependence as well as measures for alcohol consumption.
Health consequences of alcohol dependence are substantial and unambiguous. Foremost, by contributing adversely to heart diseases, cancer, accidents, and suicide, alcohol dependence shortens life expectancy by 10 to 15 yr. Alcohol dependence is also linked to such severe health conditions as fatty liver, hepatitis, cirrhosis, pancreatitis, gastritis, ulcers, fractures, and peripheral neuropathy (1). Alcohol-related health conditions may be classified into several clusters of cancer, neuropsychiatric conditions, cardiovascular conditions, gastrointestinal conditions, maternal and perinatal conditions, acute toxic effects, accidents, self-inflicted injuries, and violent deaths (2).
Despite the knowledge of the numerous chronic health effects of alcohol use and abuse, research to date is largely limited to studies of mortality. The impact on morbidity is examined less frequently. This trend is related to the accessibility of death certificates and availability of data on the cause of death. Research on morbidity is more difficult to conduct and requires more resources than research on death (3). Unlike the registration of deaths, routine registrations of physical health problems or disabilities are not generally available for analysis. Current understanding of the effects of alcohol dependence on physical health is further limited because most research employs various measures of alcohol consumption as continuous variables, instead of binomial variables of alcohol dependence or excessive alcohol use. Moreover, most research findings are from Euro-American countries, including Canada and the United States (4-6), Britain (7), Sweden (8), and Norway (9). Very limited data are available on Asian populations (10, 11). The present study attempts to fill these research gaps.
Alcohol drinking is popular in the Republic of Korea (Korea). A psychiatric epidemiologic survey conducted in Korea (12, 13) revealed that while prevalence rates of most psychiatric disorders were significantly lower compared with those found in the US, the alcohol dependence rate was substantially higher in Korea than in the US. Moreover, the rates of alcohol drinking in men and women have been increasing in Korea during the last several decades, especially among women. According to 1986 statistics, 41% of adults in Korea (14 yr or older) were drinkers. The figure was substantially higher for men (68%) than for women (17%). The rates of "daily drinkers" in men and women were 9% and 0.8%, respectively. By 1995, one-month prevalence of alcohol drinking was 63.1% for the national population of adults 20 yr or older; 83% for men and 44.6% for women. Rates of daily drinking had risen to 12% for men and 2% for women. Estimated per capita (adults) consumption of alcohol in Korea in 1996 was 13.1 L of pure alcohol (14). In 1995, 20% of all deaths in Korea were attributable to alcohol use, which findings are based on death certificates (14). There has been no epidemiologic investigation to link physical health problems and mortality directly with alcohol dependence or excessive alcohol consumption.
In this study, we compared a sample of "alcoholics," who were screened for excessive drinking or alcohol dependence, with a control sample of "non-drinkers," comprised of abstainers and minimal drinkers. Health outcomes considered in the analyses were 6-yr prevalence of mortality and point prevalence of chronic health conditions. Analyses also examined the role of smoking in exacerbating the effects of alcohol on mortality and morbidity.
Data for the present study were derived from a survey of adult residents of a rural community, Guyrae-myon, in the Republic of Korea. To date, health and addiction research has failed to address adequately the special needs of rural populations, thus making the choice of this village well-justified. Furthermore, the current study is the only epidemiological study that provides empirical data connecting alcohol abuse, mortality, and health conditions in a rural population of Korea. Guyrae-myon is a small farming village surrounded by mountains that limit social and economic interactions with even nearby cities and towns. There is no direct access by train, and bus services are restricted to only a few times a week. Most residents of the village visit nearby cities or towns several times a month. They are almost exclusively farmers of very small pieces of land, who have little education and income, and who maintain their traditional way of life.
In 1998, we contacted and interviewed all adults 18 yr and older who were living in Guyrae-myon during the 3-month period of fieldwork from April to June 1998. A total of 1,058 adults completed interviews in their homes providing information related to alcohol behaviours and health behaviours as well their basic demographic characteristics (15). Guyrae-myon was instrumental for the survey research because residents were approachable and cooperative. Whereas participation rates often fall below 30% in surveys of urban residents of Korea, we were able to complete initial interviews with 100% of adults who were actually residing in Guyrae-myon and were not traveling or visiting elsewhere during the surveys. The purpose of the initial 1998 survey was to estimate rates of alcohol consumption, abuse, and dependence, and related health behaviors such as eating breakfast (many heavy drinkers skip breakfast and instead have a drink in the morning), smoking, and exercise (e.g., walking and jogging). Unfortunately, we did not plan a follow-up at the time of the 1998 survey. We designed the follow-up study six years later, which we conducted in 2004. Given limited financial resources, we could not follow-up with all 1,058 subjects. To maximize the statistical power, we employed the nested case-control design, contrasting the alcohol "abuse" cases with abstinent or nearly abstinent "control" subjects.
In 2004, using the methods described below, we reviewed the 1998 survey data and identified 145 subjects (117 men and 28 women) who showed alcohol dependence or excessive drinking. A control sample of 145 subjects was also selected from the 1998 sample. The control sample consisted of abstinent adults or those with minimal consumption. Of all abstinent female subjects, we selected 28 women to best match the age distribution of the women in the "alcoholic" sample. There were few non-drinkers among male subjects. Age-matched control cases were selected from those whose 1998 data indicated minimal alcohol consumption (less than 12 gm per day) and a score of zero on the Severity of Alcohol Dependence Questionnaire (SADQ).
Upon arriving in Guyrae-myon we found that during the six years following the 1998 survey, 20 (13.8%) of the 145 subjects of the "alcoholic" sample and 14 (9.7%) of the control sample had died. There were 72 cases lost through survey attrition, 30 (41.7%) from the alcoholic sample, and 42 (58.3%) from the control sample. Thus, we were able to complete follow-up interviews with 95 subjects (65.5%) from the alcoholic sample and 89 (61.4%) from the control sample. Missing case analysis revealed that the attrition cases were significantly younger in age (m=47.17; sd=16.94) compared with those who completed interviews (m=59.91; sd=13.88). Distributions of sex, marital status, education, alcohol dependence, excessive drinking, and the rate of smoking were not different between participants and lost cases.
Health care professionals at a teaching hospital (6 physicians, 2 nurses, and 2 social workers) conducted follow-up interviews at the homes of the respondents in the summer of 2004. To minimize the potential for interviewer (professional) bias, all attended training sessions for interview procedures and skills. In addition, the interviews followed a structured protocol, which consisted of close-end questions. We believe that the training and the adoption of structured interviews consisting of closed-end question items minimized the effects of interviewer bias on survey responses. However, we applied statistical control of the interviewer effect where deemed relevant.
In the 1998 survey, we used the SADQ to identify cases of alcohol dependence (16, 17). This 20-item scale obtains information on physical and affective withdrawal symptoms, withdrawal relief drinking, consumption patterns, and rapidity of reinstatement of dependence during a heavy drinking period. Subjects were asked to answer on a 4-point Likert scale ranging from "almost never (=0)" to "nearly always (=3)". In this study, we applied sex-specific cutoffs of SADQ≥16 for men and SADQ≥10 for women. These criteria tend to screen male cases of "severe alcohol dependence." The cutoff for females (SADQ≥10) was used to increase representation of female subjects in the sample. SADQ has been demonstrated as a reliable and valid instrument (16, 17). In this survey, we found strong reliability of the scale based on Cronbach's alpha coefficients (0.86). Because data supporting the validity of the translated Korean version of SADQ is limited, in our 2004 follow-up survey we repeated the SADQ and also included the Alcohol Dependence Scale (ADS), another popular measure of alcohol dependence. The ADS Korean version was validated recently (18). We found that the SADQ was strongly correlated with the ADS (r=.89, p<.001), providing preliminary evidence for the validity of the SADQ.
To identify excessive alcohol users, we used responses to questions of daily alcohol consumption from the original 1998 survey. Although different aspects of alcohol consumption have been related to mortality or morbidity, overall volume or average volume consumption have been used most commonly as indicators of excessive drinking in epidemiological research (19). In this study, male subjects were classified as excessive drinkers if the average volume of daily consumption was 90 gm or greater of pure alcohol. For female subjects, we used a 45 gm cutoff.
All mortality cases were identified through interviews with family members, neighbors, and the population registry office of Guyrae-myon. The presence of chronic health problems was assessed during the 2004 follow-up interviews. Respondents were provided with a list of chronic health conditions and asked to report those they currently suffered from. The list included hepatic disorders, neuritis, gastric disorders, enteric disorders, pancreatic disorders, insomnia, depression, and cerebrovascular disorders. Interviewers were trained to use standardized methods of probing and providing feedback to assist respondents who did not understand the health conditions. Subjects were classified as either having one or more chronic health conditions (=1) or being free of chronic health conditions (=0).
Information on smoking status was collected during the 1998 survey. During the interviews, subjects were asked whether they had ever smoked. The responses were coded as nonsmokers (never smoked), former smokers, and current smokers.
Age, sex, marital status, education, and religion were measured at the 1998 survey. Chronological age was categorized. Marital status (=1) was contrasted with currently not married (=0). Subjects were also classified into two levels of education: less than ninth grade and ninth grade or beyond. Religious affiliation was coded as Christianity (Protestant and Catholic), Buddhism, and no religion or other religion.
Data were analyzed with SPSS 12.0. Type I error of 5% was used for statistical significance. A multivariate binary logistic regression procedure was used to estimate odds ratios and 95% confidence intervals (CI). To assess the "net" effects of alcohol dependence and excessive drinking, we took age, sex, marital status, education, religion, and smoking into account in the models. To further specify the effects of alcohol, the analyses of mortality and morbidity included comparisons of the control sample with cases of "alcohol dependence only," "excessive drinking only," and "all alcoholic." We also examined the hypothesis that the health effects of alcohol may be exacerbated for smokers. To test this hypothesis we included multiplicative interaction terms, alcohol dependence, and excessive drinking by smoking status in all models.
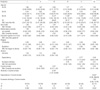
Descriptive statistics of the samples are shown in Table 1. As reported in the first column of the table, the total sample was over-represented by males (79.8%). This uneven gender distribution is due to the higher rate of alcohol problems in men. The mean ages at the 1998 survey were 57 and 59 yr for men and women, respectively. Because we tried to matchage and sex in the samples, there were few sample differenceson these variables. Compared with women in the samples, men were more likely to be married; 87.4% of men compared with 68.2% of females were currently married. The sex difference in marital status in the alcoholic sample (89.1% vs. 56.5% for men and women, respectively) was statistically significant (p<0.05). In the control sample, the sex difference (85.4% and 81.0%) was not significant.
Less than 40% of men and 12% of women had completed middle school (ninth grade), suggesting an educational level that is substantially lower than the national average (15). Regarding self-identified religious affiliation, nearly 60% of male and 50% of female subjects indicated no religious affiliation. About 14% were identified as Christians, whereas over one-quarter of male and over one-third of female subjects were identified as Buddhists. The representation of Christian affiliation was significantly stronger in the control sample than in the alcoholic sample (p<0.01).
With respect to alcohol drinking, at the time of 1998 survey, 22.1% of the sample was drinking almost every day. The average daily alcohol consumption was 59.6 gm (sd=81.83 gm) in men and 11.1 gm (sd=22.97 gm) in women. One in every 5 men consumed more than 90 gm of alcohol daily, and 2.5% of women consumed more than 45 gm daily. On the SADQ, 20.2% of men and 2.9% of women scored 10 or greater.
Among all subjects, 55.5% were current smokers at the time of 1998 survey, and 72.0% had ever smoked. Almost one-third of male subjects were current smokers and over 80% of them were either current or previous smokers. The figures were significantly lower among women. Less than 30% of all female subjects ever smoked. No female subjects in the control sample ever smoked. However, in the alcoholic sample, the sex difference in smoking rates was substantially reduced. Nearly 55% of the female alcoholics were either current or previous smokers. Thus, the current data suggest a significant co-morbidity of alcohol drinking and smoking in both men and women.
Results of logistic regressions on mortality are summarized in Table 2. The figures reported in the tables are odds ratios and 95% confidence limits of the estimated odds. All models include the demographic controls and smoking status. The first three models (I to III) in Table 2 examine the difference between the two samples. Model I shows the main effects of alcohol, whereas Model II examines the main effects of alcohol and smoking. Model III tests the joint effects of alcohol and smoking. The results from the first two models (I and II) were negative. Neither alcohol nor smoking independently was associated with the 6-yr mortality, but alcohol and smoking jointly increased the risk of 6-yr mortality.
The next three models (IV to VI) disaggregate the effects of alcohol dependence and excessive drinking. In model IV, taking into account the effects of control variables, we found that the 6-yr mortality rate was 2.77 times greater in adults with alcohol dependence, compared with the rate in the control sample. The odds were statistically significant (p<0.05). Controlling for the effects of alcohol dependence, neither excessive drinking nor smoking was significantly related to mortality. As reported in Model VI, the adverse effects of alcohol dependence were dramatically increased among those who were smoking at the time of the 1998 survey, showing an odds ratio greater than 24 (p<0.05). For nonsmokers, the odds (0.26) were not significantly different from 1.0.
Among the 184 subjects interviewed in the 2004 follow-up survey, 43 men (29.5%) and 10 women (26.3%) reported having at least one of the chronic health conditions enlisted. Table 3 shows logistic models of morbidity. In Model I, we note increasing risks in the elderly (p<0.05). Taking into account the sample variations in age and other factors shown in Model I, the estimated morbidity rate for the alcoholic sample was 2.64 times higher than for the control sample (p<0.05). In Models II and III, the results show no effects of smoking on morbidity.
In Models IV and VI, we showed the main effects and interactive effects of alcohol dependence and excessive drinking on morbidity. As shown in Model V, the prevalence of a chronic health condition was about three times greater for adults with alcohol dependence compared with nondrinkers or minimal drinkers (p<0.01). Smoking did not show significant impact. The multiplicative term of dependence by smoking (in Model VI) was statistically significant. The odds ratio of the term (0.11) was considerably smaller than 1, suggesting a significantly moderated effect of alcohol dependence on morbidity among current smokers. This result was contrary to our expectation and the results noted with regard to mortality in Table 2.
The objective of this study was to examine the effects of alcohol dependence and excessive drinking on mortality and the morbidity of chronic health conditions in a rural population of lower socio-economic (SES) status in Korea. The results of multivariate analyses showed substantial and significant adverse effects of alcohol dependence on both mortality and chronic health conditions. Controlling the variances in age and sex as well as other control variables, the rates of 6-yr mortality and morbidity were about three times higher among the subjects with alcohol dependence compared with the rates for the nondrinking sample. Excessive drinking alone was not related to the health outcomes. Results also confirmed moderating effects of smoking. With reference to mortality, the significant effect of alcohol dependence appeared to be large and significant only for smokers. For morbidity of chronic conditions, the effect of alcohol dependence was much greater among nonsmokers. It seems that those who developed chronic health problems might have stopped smoking prior to the survey.
With regard to excessive drinking, our findings are inconsistent with previous research showing significant associations between the volume of alcohol consumption and health outcomes (2, 3, 5-9, 20). It is possible that the inconsistency may be due to the fact that the present study examined the effects of alcohol dependence and excessive drinking in the same models, whereas previous research tends to have relied only on the level of alcohol consumption (19) or on one categorical measure (e.g., alcohol abuse, dependence, binge drinking, etc.) alone. More recently, patterns of drinking have gained increasing attention. In particular, heavy drinking occasions (21), drinking with meals (22), and beverage type (23, 24) have been measured frequently. In general, Graduated Frequency (GF) measures are preferred to the Quantity and Frequency (QF) measures (19, 25). In addition to the alcohol consumption and drinking patterns, researchers have used the CAGE questionnaire for problem drinking history (26) and DSM-IV criteria of alcohol dependence (27). It is difficult to determine how well the methods used in the present study for classifying alcohol dependence and excessive drinking correspond to these other measures.
The literature also suggests that the type of beverage may be related to health consequences. Although controversial (28), several prospective population studies reported reduced risk of mortality among wine drinkers of any type compared with consumers of beer or liquor (24, 29, 30). In our sample of low SES, rural Korean farmers, we found little variation in the type of beverage. Almost all drinkers in our sample of small farmers were soju drinkers, soju being the most widely consumed and affordable alcoholic beverage in Korea. When we analyzed with regard to the beverage type, exercise, breakfast, SES insomnia, etc., those variables did not influence either mortality or morbidity.
As noted, most previous studies concentrate on mortality due to the methodological challenges associated with assessing health problems (3). The present study reports adverse impacts of alcohol dependence on both mortality and morbidity. While the findings contribute to the literature, the findings on mortality need to be considered with some stipulations. The assessment of chronic health conditions was limited to the respondents' self-reports on selected health conditions, and because of the small sample size, our analyses employed a binary measure and classified subjects either as having or not having at least one chronic condition. Neither were we able to distinguish conditions diagnosed recently from health problems that subjects had had for years. We also excluded hypertension and cardiovascular disorders because the risk for cardiac failure was not related in a linear manner to the level of consumption, or moderate consumption appeared to protect against congestive heart (31), stroke, and peripheral arterial disease (32). We cannot be definite, however, about the extent to which the omissions of hypertension and cardiovascular disorders might have influenced the unexpected moderation by smoking status on the impact of alcohol dependence.
The current samples were relatively small to test the hypotheses with confidence. Although findings of this study may be generalized to rural populations of Korea, the extent to which the results are applicable to the general population of Korea is difficult to determine. For example, the age of onset of alcohol drinking in Korea is significantly younger than the current age of our participants. Readers are also reminded that the effects of alcohol as reported in this study were estimated based on the comparisons of persons with severe alcohol problems with a control sample of nondrinkers. Thus, we could not investigate health effects of moderate alcohol consumption.
A considerable number of subjects were lost to attrition, and the rate was higher for younger adults and among non-alcoholic controls than for the older and alcoholic subjects. The differential attrition rates might have influenced the findings of the study. However, at least two observations suggest minimal influence of the study attrition. First, younger age was the only variable that distinguished the lost cases from the participants. However, results showed that older age was associated significantly with mortality and morbidity. Had we been able to complete our follow-up survey with all 290 cases of the alcoholic and control samples, we would have found even greater differences in health between the two samples compared to the effects found in the currently reported analyses. Second, the interaction of alcohol by age was not significant in analyses shown in Tables 2 and 3, indicating that the differential rates of attrition in the alcoholic and control samples would not have biased the results shown in the respective tables.
Cohort data analysis is always challenging because of modeling predictors or risk factors. However, there are at least three reasons for supporting our approach in data analysis. First, in examining the impact of risk factors, it is not entirely clear whether current status is the best option to use; we may be placing the cart in front of horse. Second, ideally, analyses would include both the baseline status and the changes in the predictors. However, given the limited sample and the changes only in a small number of cases, we restricted the analyses with the status of predictors in the baseline survey. Finally, the approach allows us to assess the health consequences of alcohol abuse regardless of the changes in social status or behavioral modification made in due course (of 6 yr), some of which may be motivated by the onset of health conditions. While these issues are a subject to debate, in our view, the findings of the current study are unlikely to alter due to the use (or omissions) of the changes in risk factors.
Diverse forms of self-reported chronic health conditions are available and used quite regularly in epidemiological surveys. Most of these self-reported health measures, including the scale used in the current study, are vulnerable to the potential measurement bias due to subjectivity and accuracy. Our measure is also vulnerable to the inability of capturing changes in health status over the follow-up period (6 yr). Clearly, the unknown validity of the morbidity measure is a flaw of this study. However, the reported associations of the mortality with older age and the unmarried provide partial support for the validity of the measure. It is also important to interpret the results on morbidity in combination with the results on mortality. That alcohol dependence and excessive drinking are related to both mortality and morbidity in similar ways adds to the evidence supporting the adverse health effects of alcohol abuse. Overall, despite the measurement flaw, the inclusion of the morbidity enhances the conclusion on noxious effects of excessive alcohol use and abuse.
In conclusion, health effects of alcohol dependence were confirmed in a rural population in Korea. Given, however, that alcohol dependence, and not excessive drinking per se, was associated with a multifold increase of risk for mortality and chronic health problems, future investigations on the use and effects of alcohol among different global populations would benefit by including measures of alcohol dependence along with measures of alcohol consumption and patterns of drinking. Findings of the present study also emphasize the importance of conducting prospective studies and incorporating measures of a wide range of health outcomes. Empirical data on the factors and processes that discriminate between cases of alcohol dependence and cases of excessive drinking (without dependence) may offer intervention strategies to prevent alcohol-related health conditions and deaths.
Figures and Tables
Table 1
Descriptive statistics of the study variables for alcoholic and non-alcoholic samples by sex

ACKNOWLEDGMENTS
This study was supported by the Gangwon Alcohol Counseling Center in Wonju. The authors than Dr. Min-Hyuk Kim, Dr. You-Ra Lee, the rural community, Guyrae-myon, and participants.
References
1. Schuckit MA. Sadock BJ, Sadock VA, Kaplan HI, editors. Alcohol-Related Disorders. Kaplan & Sadock's comprehensive textbook of psychiatry. 2004. 8th ed. Philadelphia: Lippincott Williams & Wilkins;1168–1188.
2. Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, Grube J, Gruenewald P, Hill L, Holder H, Homel R, Osterberg E, Rehm J, Room R, Rossow I. Babor T, editor. The global burden of alcohol consumption. Alcohol: no ordinary commodity: research and public policy. 2003. New York: Oxford University Press;57–92.

3. Rehm J, Gmel G, Sempos CT, Trevisan M. Alcohol-Related Morbidity and Mortality. Alcohol Res Health. 2003. 27:39–51.
4. Rehm JT, Bondy SJ, Sempos CT, Vuong CV. Alcohol consumption and coronary heart disease morbidity and mortality. Am J Epidemiol. 1997. 146:495–501.

5. Thun MJ, Peto R, Lopez AD, Monaco JH, Henley SJ, Heath CW Jr, Doll R. Alcohol consumption and mortality among middle-aged and elderly U.S. adults. N Engl J Med. 1997. 337:1705–1714.

6. Single E, Robson L, Rehm J, Xi X. Morbidity and mortality attributable to alcohol, tobacco, and illicit drug use in Canada. Am J Public Health. 1999. 89:385–390.

7. Doll R, Peto R, Hall E, Wheatley K, Gray R. Mortality in relation to consumption of alcohol: 13 years' observations on male British doctors. BMJ. 1994. 309:911–918.

8. Romelsjo A, Leifman A. Association between alcohol consumption and mortality myocardial infarction, and stroke in 25 year follow up of 49,618 young Swedish men. BMJ. 1999. 319:821–822.
9. Rossow I, Amundsen A. Alcohol abuse and mortality: a 40-year prospective study of Norwegian conscripts. Soc Sci Med. 1997. 44:261–267.

10. Yuan JM, Ross RK, Gao YT, Henderson BE, Yu MC. Follow up study of moderate alcohol intake and mortality among middle aged men in Shanghai, China. BMJ. 1997. 314:18–23.

11. Tsugane S, Fahey MT, Sasaki S, Baba S. Alcohol consumption and all-cause and cancer mortality among middle-aged Japanese men: Seven-year follow-up of the JPHC study cohort I. Am J Epidemiol. 1999. 150:1201–1207.

12. Lee CK, Kwak YS, Yamamoto J, Rhee H, Kim YS, Han JH, Choi JO, Lee YH. Psychiatric epidemiology in Korea. Part I: Gender and age differences in Seoul. J Nerv Ment Dis. 1990. 178:242–246.
13. Lee CK, Kwak YS, Yamamoto J, Rhee H, Kim YS, Han JH, Choi JO, Lee YH. Psychiatric epidemiology in Korea. Part II: Urban and rural differences. J Nerv Ment Dis. 1990. 178:247–252.
14. World Health Organization. Dept. of Mental Health and Substance Abuse. Global status report on alcohol. 1999. Geneva: World Health Organization. Dept. of Mental Health and Substance Abuse.
15. Shin J, Min S, Park K, Lee J, Pyo J. An epidemiologic study on alcoholism and alcohol abuse in an isolated mountainous rural community. J Korean Acad Addict Psychiatry. 1999. 3:99–106.
16. Stockwell T, Murphy D, Hodgson R. The severity of alcohol dependence questionnaire: Its use, reliability and validity. Br J Addict. 1983. 78:145–155.

17. Potamianos G, Gorman DM, Duffy SW, Peters TJ. The use of the severity of alcohol dependence questionnaire (SADQ) on a sample of problem drinkers presenting at a district general hospital. Alcohol. 1984. 1:441–445.

18. Lee D, Shin J, Yun S, Byun W. A reliability and validity study of the Korean version of the alcohol dependence scale in alcoholics. J Korean Acad Addict Psychiatry. 2000. 4:30–37.
19. Rehm J, Gmel G. Alcohol consumption and total mortality/morbidity-Definitions ane methodological implications. Best Pract Res Clin Gastroenterol. 2003. 17:497–505.
20. Schuckit MA, Tapert S. Galanter M, Kleber HD, editors. Alcohol. The American Psychiatric Publishing textbook of substance abuse treatment. 2004. 3rd ed. Washington, DC: American Psychiatric Pub;156–158.
21. Rehm J, Greenfield TK, Rogers JD. Average volume of alcohol consumption, patterns of drinking, and all-cause mortality: Results from the US national alcohol survey. Am J Epidemiol. 2001. 153:64–71.

22. Trevisan M, Schisterman E, Mennotti A, Farchi G, Conti S. Drinking pattern and mortality: The Italian Risk Factor and Life Expectancy Pooling Project. Ann Epidemiol. 2001. 11:312–319.
23. Rimm EB, Klatsky A, Grobbee D, Stampfer MJ. Review of moderate alcohol consumption and reduced risk of coronary heart disease: Is the effect due to beer, wine, or spirits? BMJ. 1996. 312:731–736.

24. Klatsky AL, Friedman GD, Armstrong MA, Kipp H. Wine, liquor, beer, and mortality. Am J Epidemiol. 2003. 158:585–595.

25. Greenfield TK. Ways of measuring drinking patterns and the difference they make: Experience with graduated frequencies. J Subst Abuse. 2000. 12:33–49.

26. Perreira KM, Sloan FA. Excess alcohol consumption and health outcomes: A 6-year follow-up of men over age 50 from the health and retirement study. Addiction. 2002. 97:301–310.

27. Dawson DA. Alcohol consumption, alcohol dependence, and all-cause mortality. Alcohol Clin Exp Res. 2000. 24:72–81.

28. Grønbæk M. Factors influencing the relation between alcohol and mortality - With focus on wine. J Intern Med. 2001. 250:291–308.

29. Grønbæk M, Becker U, Johansen D, Gottschau A, Schnohr P, Hein HO, Jensen G, Sorensen TI. Type of alcohol consumed and mortality from all causes, coronary heart disease, and cancer. Ann Intern Med. 2000. 133:411–419.

30. Theobald H, Bygren LO, Carstensen J, Engfeldt P. A moderate intake of wine is associated with reduced total mortality and reduced mortality from cardiovascular disease. J Stud Alcohol. 2000. 61:652–656.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download