Abstract
Tumor necrosis factor (TNF) is essential for host defense against Mycobacterium tuberculosis, and the risk of reactivation of latent tuberculosis infection (LTBI) increases with anti-TNF therapy. This study estimated the prevalence of LTBI and evaluated the safety and completion rate of short-course therapy with isoniazid plus rifampin for 3 months to treat LTBI in a cohort of Korean arthritis patients before initiating anti-TNF therapy. We retrospectively studied the files of 112 consecutive patients to evaluate LTBI before starting anti-TNF drugs. Screening tests were performed, including a tuberculin skin test and chest radiography. LTBI treatment was indicated in 41 patients (37%). Of these, three patients refused the LTBI treatment. Of the 38 patients who underwent LTBI treatment, 36 (95%) took isoniazid plus rifampin for 3 months. Six patients (16%) showed transient elevations of liver enzymes during the LTBI treatment. Overall, 35 patients (92%) completed the LTBI treatment as planned. In conclusion, LTBI was diagnosed in one-third of Korean arthritis patients before initiating anti-TNF therapy. A high percentage of these patients completed 3 months of LTBI treatment with isoniazid plus rifampin without serious complications.
The introduction of biological agents that counter tumor necrosis factor (TNF)-α represents a major advance in the treatment of rheumatoid arthritis (RA) and other systemic inflammatory diseases, including ankylosing spondylitis (AS) (1-4). However, the association with increased occurrence of tuberculosis is a major concern (5, 6). TNF-α is an essential cytokine that plays an important role in the immune response against Mycobacterium tuberculosis (7), and the reemergence of active tuberculosis has been reported soon after patients began taking TNF-α antagonists (8). Therefore, it is critical to diagnose and treat latent tuberculosis infection (LTBI) before commencing treatment with TNF-α antagonists in these patients.
Isoniazid has been the mainstay of LTBI treatment for over 40 yr worldwide. Unfortunately, the recommended lengthy treatment (9 months) with isoniazid has compromised this regimen as an effective tool, as only 50-60% complete the regimen (9). In the United States, 6 months of isoniazid (6H), 4 months of rifampin (4R), and 2 months of rifampin and pyrazinamide (2RZ) are recommended as acceptable alternatives to the preferred 9 months of isoniazid (9H) (9). After these recommendations were published in 2000, they were revised to indicate that 2RZ should not be generally offered because it caused severe hepatotoxicity and mortality (10). In the United Kingdom, 6H and 3 months of isoniazid and rifampin (3HR) are recommended (11).
In December 2004, the Korea Food and Drug Administration strongly recommended treating LTBI in patients before starting TNF-α antagonist therapy using one of the recommended regimens: 6H (or 9H), 4R, 3HR, or 2RZ (12). In addition to the low completion rate due to the lengthy treatment, the 6H and 9H regimens have limitations in countries with high isoniazid resistance rates. A recent national survey found that 9.9% of new tuberculosis cases in Korea involved isoniazid-resistant strains (13). Although the regimen of 3HR or 4R has some merits in this situation, the efficacy of each regimen for treating LTBI has never been evaluated in Korea.
Therefore, this study estimated the prevalence of LTBI and evaluated the safety and completion rate of the 3HR regimen for treating LTBI in a cohort of Korean arthritis patients before commencing anti-TNF agents.
We retrospectively studied the files of 112 consecutive patients with RA or AS who visited our facility to evaluate LTBI before starting anti-TNF drugs during a 22-month period (December 2004-September 2006) at the Samsung Medical Center, Seoul, Korea. Diagnosis of RA or AS was defined according to the proposed criteria (14, 15). All the patients were diagnosed, treated, and followed in the same rheumatology center. Approval from the institutional review board was obtained to review the patient records retrospectively and to publish the results.
The diagnosis of LTBI was made from the medical history and screening tests. The evaluation of the medical history included current symptoms, a prior history of treatment for tuberculosis, and a recent contact history of patient with active pulmonary tuberculosis. All the patients had a tuberculin skin test (TST) and posteroanterior chest radiography (CXR) taken before beginning the anti-TNF treatment. Patients with a history of adequate previous therapy for tuberculosis and no current evidence of active pulmonary tuberculosis on CXR were not given the TST.
The TST was performed on the volar side of the forearm according to the Mantoux method (9) using a 2-TU dose of purified protein derivative RT23 (Statens Serum Institute, Copenhagen, Denmark). The TST was considered positive when the transverse diameter of the induration exceeded 10 mm after 48-72 hr using the ball-point method (16). A positive TST result without an active tuberculosis lesion on CXR was considered an indication for LTBI treatment.
In addition, a recent contact with patients having active pulmonary tuberculosis, an abnormal CXR suggesting latent tuberculosis without adequate prior treatment, or an inadequate treatment history of tuberculosis were indications for LTBI treatment regardless of the TST results (12). When LTBI treatment was indicated, the anti-TNF treatment was started 1 month later. All the patients received etanercept.
All patients who were diagnosed with LTBI had their liver chemistry, hepatitis B virus surface antigen, and hepatitis C virus antibody assessed before commencing LTBI treatment, and none of these patients had abnormal liver chemistry or were positive for hepatitis B virus surface antigen or hepatitis C virus antibody. In the LTBI treatment, most of the patients were placed on the 3HR regimen (isoniazid 300 mg/day plus rifampin 600 mg/day, if the body weight was <50 kg, rifampin 450 mg/day for 3 months). A few patients were placed on the 4R regimen (rifampin, dose as above for 4 months).
The attending physician assessed adherence and adverse reactions using the clinical signs, symptoms, and liver chemistry at 4-week intervals. The serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels were monitored monthly. The following criteria were used to define transient transaminase elevation and drug-induced hepatotoxicity (17). Transient transaminase elevation was diagnosed if the AST/ALT levels increased, but were still less than three times the upper normal limit (120 IU/L), and resolved spontaneously despite continued medication. Drug-induced hepatotoxicity was diagnosed when liver transaminase levels exceeded 120 IU/L.
Numerical variables were given as the mean±standard deviation (SD). Categorical variables were presented as numbers and percentages. Variables were compared between patients with AS and RA using the Fisher's exact test, chisquare test, and Student's t-test, as appropriate. A p<0.05 was considered statistically significant.
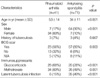
The study identified 112 consecutive patients referred for the evaluation of LTBI before starting anti-TNF therapy (71 men and 41 women; mean age±SD, 41±15 yr). The diagnosis of RA was established in 41 patients (37%) and AS in 71 (63%). The patient characteristics are summarized in Table 1.
No patient had signs, symptoms, or CXR findings suggestive of current active pulmonary tuberculosis. The TST was performed in 106 patients, excluding the six patients who had received adequate therapy for previous tuberculosis. Forty-one patients had a positive TST. Of the patients with a negative TST, none had recent contact with patients with active pulmonary tuberculosis, an abnormal CXR suggesting latent tuberculosis, or inadequately treated prior tuberculosis. Therefore, LTBI treatment was indicated in 41 arthritis patients (37%) scheduled to receive anti-TNF agents.
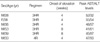
The prevalence of LTBI and the clinical characteristics of the patients with RA and AS differed. LTBI was diagnosed in more patients with AS (35/71, 49%) than with RA (6/41, 15%; p<0.001). Most of the patients with AS were men (64 [90%] of 71), while few men had RA (7 [17%] of 41; p<0.001]. The patients with AS were younger (mean age 34 yr) than those with RA (mean age 53 yr; p<0.001). Patients with AS were more likely to have a Bacillus Calmette-Guérin (BCG) scar (57 [80%] of 71) compared to those with RA (23 [56%] of 41; p=0.003). The percentage of patients receiving immunosuppressants, including systemic glucocorticoids or methotrexate, was higher in patients with RA compared to those with AS (p<0.001; Table 2).
Three of the 41 patients who were diagnosed with LTBI
refused both LTBI treatment and anti-TNF drug therapy.
Therefore, 38 patients received LTBI treatment; 3HR in 36
patients (95%) and 4R in two patients (5%).
Six patients (16%, 6/38) showed a transient elevation of AST or ALT during the LTBI treatment, which normalized spontaneously without discontinuing the treatment. The AST and ALT levels in these patients are shown in Table 3. Three patients (8%, 3/38) were switched to another regimen because of adverse reactions, such as a skin rash or gastrointestinal disturbance. Two patients starting the 3HR regimen were switched to the 4R regimen and one patient starting with the 4R regimen was switched to the 6H regimen. Thirty-five patients (92%, 35/38) completed the LTBI treatment as planned, while three were nonadherent.
The main objectives of this study were to estimate the prevalence of LTBI and to evaluate the completion rate and safety of the 3HR regimen for treating LTBI in Korean patients with RA or AS before starting anti-TNF agents. Using the TST, LTBI was diagnosed in more than one-third in these patients and the treatment of LTBI with the 3HR regimen had a high completion rate with few complications.
Since TNF-α plays a central role in mycobacterial infection, it is not surprising that anti-TNF therapy is associated with the progression of recently acquired tuberculosis or the reactivation of LTBI. Currently, three anti-TNF agents are in clinical use: etanercept, infliximab, and adalimumab. As of June 2002, 295 cases of tuberculosis among patients receiving infliximab and 36 cases among those receiving etanercept had been reported to the US Food and Drug Administration (18). Adalimumab was also associated with tuberculosis during clinical trials (6). Most patients were thought to have a reactivation of LTBI. Tuberculosis associated with anti-TNF agent therapy has an unusual presentation, as more than half of the cases have extrapulmonary disease, while one-fourth have disseminated disease (8). Therefore, all candidates for anti-TNF therapy should undergo screening for LTBI before initiating these drugs. In December 2004, the Korea Food and Drug Administration strongly recommended that LTBI be diagnosed and treated in patients before starting TNF antagonists.
The prevalence of LTBI in arthritis patients before initiating anti-TNF therapy has never been reported in Korea. In this study, 37% (41/112) of the patients who were scheduled to receive anti-TNF agents had a positive TST, and LTBI treatment was indicated.
We used the TST for the diagnosis of LTBI, but the TST has several limitations. The interpretation of negative tests is complicated by the effect of immunosuppressants precluding effective testing. Moreover, patients with RA might not produce an adequate delayed type hypersensitivity reaction to tuberculin because of their deficient cell-mediated immunity (19, 20). Therefore, a false negative TST makes it unreliable for determining the risk of tuberculosis (21). In addition, it is still uncertain whether prior BCG vaccination affects the interpretation of a TST. Individuals vaccinated with BCG are more likely to have a positive TST; however, the size of the reaction almost never exceeds 15 mm (22). In this study, the prevalence of LTBI differed in patients with RA (15%) and AS (49%). These results may have been influenced by confounding factors such as age, BCG vaccination status, and the use of immunosuppressant agents, including systemic glucocorticoids.
New blood tests, based on the detection of interferon-γ produced by T cells in response to antigens specific to M. tuberculosis, have recently been developed and are available commercially (QuantiFERON-TB Gold; Cellestis Ltd; Victoria, Australia and T-SPOT.TB assay; Oxford Immunotec; Oxford, United Kingdom). These tests might be more accurate than the tuberculin skin test (23, 24), but the number of studies in immunosuppressed patients is limited. Therefore, until other more accurate diagnostic tests are available for identifying LTBI in routine clinical practice, the TST should continue to be used.
Four potential treatment regimens are used for LTBI: 6H, 4R, 3HR, or 2RZ (9, 11, 12). Rifampin and pyrazinamide for 2 months (2RZ) had a very high rate of hepatitis with several fatalities reported. Accordingly, the choice of regimen is between 6H (or 9H), which has a lower hepatitis rate, and 3HR (or 4R), which may have advantages in terms of shorter duration and possibly better adherence, and less risk of drug resistance developing if active disease is present (11). In particular, poor patient adherence to the 6H or 9H regimen due to the long course and a high prevalence of isoniazid-resistant tuberculosis in Korea make the 6H or 9H regimens less advantageous for LTBI treatment.
A recent meta-analysis demonstrated that short-course therapy with isoniazid plus rifampin for 3 months was equivalent to standard therapy with isoniazid for 6-12 months in terms of efficacy, the proportion of severe side effects, and mortality (25). With due regard to these results, 3HR was the main regimen used to treat LTBI in our institution, shortly after the recommendation for the diagnosis, and treatment of LTBI was released by Korea Food and Drug Administration.
In this study, most (95%, 36/38) of the patients in whom LTBI treatment was indicated received daily short-course therapy with isoniazid plus rifampin for 3 months. Only two patients receiving the 3HR regimen were switched to the 4R regimen due to drug side effects, including skin rash or gastrointestinal disturbance. Five patients (14%, 5/36) receiving 3HR experienced transient elevation of AST or ALT during the LTBI treatment, which normalized spontaneously without discontinuing the treatment. Moreover, the completion rate was relatively high in this study (92%, 35/38), although our study population was small.
In conclusion, the diagnosis of LTBI was made in slightly more than one-third of Korean arthritis patients before instituting anti-TNF therapy. In these patients, 3 months with isoniazid plus rifampin for LTBI treatment showed had a high completion rate without serious complications.
Figures and Tables
Table 1
The characteristics of the 112 patients with rheumatoid arthritis or ankylosing spondylitis before initiating anti-TNF therapy

ACKNOWLEDGMENTS
The authors would like to thank Soo Young Yeom, RN and Jung Sun Kwon, RN for their help in management of patients and the collection of clinical data.
References
1. Lipsky PE, van der Heijde DM, St Clair EW, Furst DE, Breedveld FC, Kalden JR, Smolen JS, Weisman M, Emery P, Feldmann M, Harriman GR, Maini RN. Infliximab and methotrexate in the treatment of rheumatoid arthritis. Anti-Tumor Necrosis Factor Trial in Rheumatoid Arthritis with Concomitant Therapy Study Group. N Engl J Med. 2000. 343:1594–1602.
2. Ledingham J, Deighton C. Update on the British Society for Rheumatology guidelines for prescribing TNFα blockers in adults with rheumatoid arthritis (update of previous guidelines of April 2001). Rheumatology (Oxford). 2005. 44:157–163.

3. Keat A, Barkham N, Bhalla A, Gaffney K, Marzo-Ortega H, Paul S, Rogers F, Somerville M, Sturrock R, Wordsworth P. BSR guidelines for prescribing TNF-α blockers in adults with ankylosing spondylitis. Report of a working party of the British Society for Rheumatology. Rheumatology (Oxford). 2005. 44:939–947.

4. Braun J, Davis J, Dougados M, Sieper J, van der Linden S, van der Heijde D. First update of the international ASAS consensus statement for the use of anti-TNF agents in patients with ankylosing spondylitis. Ann Rheum Dis. 2006. 65:316–320.

5. Hochberg MC, Lebwohl MG, Plevy SE, Hobbs KF, Yocum DE. The benefit/risk profile of TNF-blocking agents: findings of a consensus panel. Semin Arthritis Rheum. 2005. 34:819–836.

6. Mutlu GM, Mutlu EA, Bellmeyer A, Rubinstein I. Pulmonary adverse events of anti-tumor necrosis factor-alpha antibody therapy. Am J Med. 2006. 119:639–646.
7. Gardam MA, Keystone EC, Menzies R, Manners S, Skamene E, Long R, Vinh DC. Anti-tumour necrosis factor agents and tuberculosis risk: mechanisms of action and clinical management. Lancet Infect Dis. 2003. 3:148–155.

8. Keane J, Gershon S, Wise RP, Mirabile-Levens E, Kasznica J, Schwieterman WD, Siegel JN, Braun MM. Tuberculosis associated with infliximab, a tumor necrosis factor alpha-neutralizing agent. N Engl J Med. 2001. 345:1098–1104.
9. American Thoracic Society. Diagnostic standards and classification of tuberculosis in adults and children. Am J Respir Crit Care Med. 2000. 161:1376–1395.
10. Centers for Disease Control and Prevention (CDC); American Thoracic Society. Update: adverse event data and revised American Thoracic Society/CDC recommendations against the use of rifampin and pyrazinamide for treatment of latent tuberculosis infection--United States, 2003. MMWR Morb Mortal Wkly Rep. 2003. 52:735–739.
11. British Thoracic Society Standards of Care Committee. BTS recommendations for assessing risk and for managing Mycobacterium tuberculosis infection and disease in patients due to start anti-TNF-alpha treatment. Thorax. 2005. 60:800–805.
12. Korea Food and Drug Administration. Guideline for diagnosis and treatment of latent tuberculosis infection in patients treated with TNF blockers. 2004.
13. Bai GH, Park YK, Choi YW, Bai JI, Kim HJ, Chang CL, Lee JK, Kim SJ. Trend of anti-tuberculosis drug resistance in Korea, 1994-2004. Int J Tuberc Lung Dis. 2007. 11:571–576.
14. Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS, Medsger TA Jr, Mitchell DM, Neustadt DH, Pinals RS, Schaller JG, Sharp JT, Wilder RL, Hunder GG. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988. 31:315–324.

15. van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984. 27:361–368.
17. Lee BH, Koh WJ, Choi MS, Suh GY, Chung MP, Kim H, Kwon OJ. Inactive hepatitis B surface antigen carrier state and hepatotoxicity during antituberculosis chemotherapy. Chest. 2005. 127:1304–1311.

18. Sichletidis L, Settas L, Spyratos D, Chloros D, Patakas D. Tuberculosis in patients receiving anti-TNF agents despite chemoprophylaxis. Int J Tuberc Lung Dis. 2006. 10:1127–1132.
19. Nizam S, Emery P. Attenuated response to purified protein derivative in patients with rheumatoid arthritis. Ann Rheum Dis. 2006. 65:980.

20. Emery P, Panayi G, Symmons D, Brown G. Mechanisms of depressed delayed-type hypersensitivity in rheumatoid arthritis: the role of protein energy malnutrition. Ann Rheum Dis. 1984. 43:430–434.

21. Ponce de Leon D, Acevedo-Vasquez E, Sanchez-Torres A, Cucho M, Alfaro J, Perich R, Pastor C, Harrison J, Sanchez-Schwartz C. Attenuated response to purified protein derivative in patients with rheumatoid arthritis: study in a population with a high prevalence of tuberculosis. Ann Rheum Dis. 2005. 64:1360–1361.

22. Wang L, Turner MO, Elwood RK, Schulzer M, FitzGerald JM. A meta-analysis of the effect of Bacille Calmette Guerin vaccination on tuberculin skin test measurements. Thorax. 2002. 57:804–809.

23. Kang YA, Lee HW, Yoon HI, Cho B, Han SK, Shim YS, Yim JJ. Discrepancy between the tuberculin skin test and the whole-blood interferon γ assay for the diagnosis of latent tuberculosis infection in an intermediate tuberculosis-burden country. JAMA. 2005. 293:2756–2761.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download