Abstract
Vaccination against hepatitis A virus (HAV) is recommended for patients with chronic liver disease (CLD), but this has been deemed unnecessary in Korea since the immunity against HAV was almost universal in adults. However, this practice has never been reevaluated with respect to the changing incidence of adult acute hepatitis A. We retrospectively reviewed the medical records of 278 patients with acute hepatitis A diagnosed from January 1995 to November 2005 and prospectively tested 419 consecutive CLD patients from July to December 2005 for the presence of IgG anti-HAV. The number of patients with acute hepatitis A has markedly increased recently, and the proportion of adult patients older than 30 yr has been growing from 15.2% during 1995-1999, to 28.4% during 2000-2005 (p=0.019). Among 419 CLD patients, the seroprevalences of IgG anti-HAV were 23.1% for those between 26 and 30 yr, 64% between 31 and 35 yr, and 85.0% between 36 and 40 yr. These data demonstrate that immunity against HAV is no more universal in adult and substantial proportion of adult CLD patients are now at risk of HAV infection in Korea. Therefore, further study on seeking proper strategy of active immunization against HAV is warranted in these populations.
Acute hepatitis A is one of the well known vaccine preventable diseases (1) and active hepatitis A virus (HAV) vaccination is recommended in high risk populations (2). These include the two major high risk groups for fatal fulminant hepatic failure, those aged over 40 and patients with chronic liver disease (CLD) (3-6). Mortality among patients with HBsAg was found to be significantly higher than among those without HBsAg in an outbreak of HAV infection in Shanghai (7), and an analysis of HAV associated death in the United States revealed higher case fatality rate among chronic hepatitis B virus (HBV) carriers than among patients without HBV (5). Moreover, patients with hepatitis C virus (HCV) infection were reported to experience HAV associated fulminant hepatic failure more often than those without CLD (8). Given the highly effective and safe vaccines now available and a low rate of inherent immunity, the active immunization of CLD patients is emphasized in countries with a low seroprevalence of anti-HAV (9).
In Korea, where HBV is highly prevalent, age-specific immunity against HAV in the adult population older than 30 yr was reported to be 100% in the early 1980s (10) and more than 97% in 1999 (11). Therefore, the clinical significance of acute HAV infection in adults was thought to be negligible, and it has been considered unnecessary, until recently, to test for the presence of anti-HAV antibody in adults, even in high risk groups. However, as environmental conditions have improved, the seroprevalence of anti-HAV has been steadily decreasing in childhood (12), whereas the incidence of overt acute hepatitis A has recently been increasing in adults (13-15). These changes imply that more people reached adulthood without being exposed to HAV in childhood, and therefore, are at risk of developing symptomatic acute hepatitis A. However, the consequences of these changes have not been evaluated in CLD patients in Korea.
In this study, we restrospectively analyzed the changes of age distributions of acute hepatitis A patients during the last decade and prospectively investigated age-specific seroprevalences of anti-HAV in CLD patients in a 3rd referral center in Korea.
We retrospectively reviewed the medical records of patients with acute hepatitis A, who were identified by the presence of serum IgM antibody against HAV (Electrochemiluminescence, Roche Diagnostics Korea, Seoul) along with appropriate clinical manifestations from January 1995 to November 2005 at Ewha Womans University Mokdong Hospital. Annual numbers of acute hepatitis A patients were plotted, and the age distributions of patients were compared for the periods 1995-1999 and 2000-2005.
We prospectively tested the sera of consecutive chronic liver disease patients who visited the outpatient department or who were admitted to our hospital between July and December 2005, for the presence of IgG antibody against HAV using a radioimmunoassay kit (Beijing North Institute of Biological Technology, Beijing, China). Patients with chronic hepatitis B, chronic hepatitis C, alcoholic liver disease, liver cirrhosis, and hepatocellular carcinoma were included. Age-specific seroprevalences were analysed.
A total of 278 patients with acute hepatitis A were selected. The case number of acute hepatitis A was found to have steadily increased during the last decade with an extraordinarily high eruption in 1998 (Fig. 1). The majority of patients were in their twenties (21-30 yr, 49.6%) with a mean age of 24.9 yr, and 24.8% of the patients were adults older than 30 yr (Table 1).
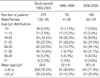
We arbitrarily divided the study period into before and after the year 2000 to determine whether the numbers of adult acute hepatitis A patients have increased recently. The age distribution of the 79 patients in pre-2000 period (1995-1999) was compared with that of the 199 patients in post-2000 period. Mean age of the post-2000 patients was significantly higher than that of the pre-2000 patients (26 vs. 22 yr, p<0.001) and the proportion of patients older than 30 yr was almost doubled between pre and post-2000 periods (15.2% vs. 28.6%, p<0.001) (Table 1). Although the most prevalent age interval was unchanged (21-25 yr), the number of patients older than 21 yr was markedly increased between the two periods and that contributes to the most of recent increase in the overall occurrence of acute hepatitis A (Fig. 2).
Four hundred and nineteen chronic liver disease patients were tested for serum IgG antibody against HAV from July to December 2005. The mean age of patients was 52 yr and 67.5% were male. Most of the patients were >40 yr old (79%) and 15% were in their thirties. HBV was associated in more than 65% and alcohol in 17.7%, followed by HCV in 12.9%. Other causes of chronic liver disease included primary biliary cirrhosis (1 case), autoimmune hepatitis (10 cases), Budd-Chiari syndrome (1 case), and cryptogenic liver cirrhosis (8 cases) (Table 2).
The overall seroprevalence of anti-HAV in CLD patients was 89.3% (374/419). As shown by Fig. 3, age-specific seroprevalences increased with age (p<0.001); 0% in patients ≤25 yr old, 23.1% in those between 26 and 30 yr, 64% between 31 and 35 yr, 85.0% between 36 and 40 yr, 94% between 41 and 45 yr, 100% between 46 and 55 yr, and 98% in patients ≥56 yr old. According to these data, the seroprevalence of anti-HAV in adults between 31 and 40 yr, which had been reported to be more than 97% before 2000 (10, 11) was substantially decreased, and about 25% of these patients were at the risk of HAV infection.
In Korea, acute symptomatic hepatitis A, which has been steadily increased since the 1980s, has become one of the most common causes of acute viral hepatitis (14). In the meantime, childhood incidence has decreased (12) while its incidence in adults has increased (13-15), as evidenced by the present study (Fig. 1, 2). In 1998 an outbreak of acute hepatitis A was recorded in several regions in Korea (11, 16). To characterize chronological changes in the ages of affected patients, we compared the age distributions of patients diagnosed in the pre-2000 and post-2000 periods. The mean age of patients was significantly higher in post-2000 and the relative proportions of adult and elderly patients were significantly increased (Table 1, Fig. 2). These results are in accordance with epidemiologic changes in HAV infection reported in other Asian populations (17), and reflect reduced immunity against HAV in adult Koreans, (11, 12, 15) including those with chronic liver disease for whom WHO recommends active vaccination.
As was anticipated, the seroprevalence of anti-HAV in middle aged adult CLD patients between the ages of 31 and 35 yr was only 64% in the present study, which was markedly lower than the 100% that reported in 1982 (10), and even 15% of patients between the ages of 36 and 40 yr were found to be at risk of HAV infection (Fig. 3). These data indicate that a substantial proportion of CLD patients younger than 40 yr are now at the risk of acute HAV infection, more specifically, 77% of patients aged 26 to 30 yr, 36% of those aged 31 to 35 yr, and 15% of those aged 36 to 40 yr. Accordingly, active immunization against HAV is demanded for these populations.
Patients older than 40 yr comprised 79% of 419 CLD patients (Table 2), and more than 94% of these had already acquired immunity against HAV, and thus, the majority of CLD patients were free of HAV infection. However, if the decreasing anti-HAV seroprevalence trend in adult continues, more CLD patients will be at risk of HAV infection in the near future (18, 19). Cases of symptomatic HAV superinfection in hepatitis virus carriers, which were very rare in the 1980s, are being reported recently in Korea. In an analysis of clinical features of 177 acute hepatitis A patients, 12 patients with serologic evidences of hepatitis virus infection; 10 HBsAg positive and 2 anti-HCV positive, were identified and mild clinical courses of these patients were described (15). On the other hand, one case of fulminant acute hepatitis A in an HBV carrier was reported in 2002, who suffered from encephalopathy, azotemia and marked prolongation of prothrombin time (20). In the present study, we identified two cases of acute HAV superinfection in chronic viral hepatitis patients, a 17-yr old female with chronic hepatitis C and a 35-yr old male with chronic hepatitis B. Both eventually recovered from symptomatic acute hepatitis A with maximum serum aminotransferase levels of 937 and 2,976 IU/mL, respectively. The 35-yr old male patient experienced more severe hepatitis with a mild prolongation of prothrombin time (70%, Internatinal Normalized Ratio 1.21).
In terms of active immunization modalities, different immunization strategies can be implemented, depending on the underlying anti-HAV seroprevalence rates (21, 22); when anti-HAV seroprevalence rate is high, selective vaccination according to anti-HAV serostatus is more cost-effective than universal vaccination. In an analysis of the cost-effectiveness of different vaccination strategies in CLD patients, Saab et al. found that screening for anti-HAV became less costly than vaccination without checking HAV serology when anti-HAV prevalence exceeded 35% and the cost of serologic testing was less than US$25 (23). Anti-HAV seroprevalence rates by age, as determined by the present study, may provide principal data for adjusting adequate vaccination strategy in CLD patients. For example, instituting selective vaccination for 31-40 yr old CLD patients (anti-HAV rate of 64-85%) and universal vaccination for patients younger than 31 yr (anti-HAV rate of 0-34%).
In addition to seroprevalence data, the cost of serologic testing, the cost of vaccination, patient compliance, and the likelihood of the occurrence of a clinically significant fatal HAV superinfection should also be determined to facilitate the identification of the most efficient vaccination strategy. In young or childhood CLD patients, the serum anti-HAV rate is very low and the risk of infection is high, but the symptomatic infection rate and the risk of severe hepatic failure are minimal and natural life long immunity is frequently attained after a mild or asymptomatic infection. Therefore, the selective HAV vaccination of middle aged adult CLD patients appears more urgent than the universal vaccination for younger CLD patients (24). Further nationwide large scale studies, including the active evaluation of the clinical significance of acute HAV infection and cost-benefit analyses of different vaccination strategies in different age groups of CLD patients will provide firmer data for designing an optimal vaccination strategy.
This single center study demonstrates that adult patients with acute hepatitis A are more frequently encountered recently and that a substantial proportion of adult patients with CLD are now susceptible to HAV infection. Although the occurrence of acute hepatitis A was analyzed retrospectively and this study was conducted in a third referral center hospital, the observed increase of acute hepatitis A patients in the adult population is concordant with previously reported data (11, 13, 15) and, to our knowledge, no prospective analysis of the age-specific seroprevalences of anti-HAV antibody in CLD patients has been conducted before in this HBV endemic area. The results of this study provide an evidence of emerging needs for HAV vaccination in adult CLD patients in Korea and for large scale investigations to find out proper vaccination strategy in these patients.
Figures and Tables
Fig. 1
Annual case numbers of acute hepatitis A from 1995 to 2005 in our hospital. The number of acute hepatitis A patients have markedly increased in recent years with an eruption in 1998.
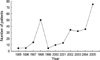
Fig. 2
Age distributions of acute hepatitis A patients during 1995-1999 and 2000-2005, demonstrating recent increasing trends among adult patients.

References
1. Craig AS, Schaffner W. Prevention of hepatitis A with hepatitis A vaccine. N Engl J Med. 2004. 350:476–481.
2. Centers for Disease Control and Prevention. Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1999. 48(RR-12):1–37.
3. Willner IR, Uhl MD, Howard SC, Williams EQ, Riely CA, Waters B. Serious hepatitis A: an analysis of patients hospitalized during an urban epidemic in the United States. Ann Intern Med. 1998. 128:111–114.

4. Wise ME, Sorvillo F. Hepatitis A-related mortality in California, 1989-2000: analysis of multiple cause-coded death data. Am J Public Health. 2005. 95:900–905.

5. Keeffe EB. Is hepatitis A more severe in patients with chronic hepatitis B and other chronic liver disease? Am J Gastroenterol. 1995. 90:201–205.
6. Lefilliatre P, Villeneuve JP. Fulminant hepatitis A in patients with chronic liver disease. Can J Public Health. 2000. 91:168–170.

7. Yao G. Hollinger FB, Lemon SM, Margolis H, editors. Clinical spectrum and natural history of viral hepatitis A in a 1988 Shanghai epidemic. Viral Hepatitis and Liver Disease. 1991. Baltimore: Williams & Wilkins;76–78.
8. Vento S, Garofano T, Renzini C, Cainelli F, Casali F, Ghironzi G, Ferraro T, Concia E. Fulminant hepatitis associated with hepatitis A virus superinfection in patients with chronic hepatitis C. N Engl J Med. 1998. 338:286–290.

9. Keeffe EB. Acute hepatitis A and B in patients with chronic liver disease: prevention through vaccination. Am J Med. 2005. 118:Supple 10A. 21S–27S.

10. Kim CY, Hong WS. Seroepidemiology of type A and type B hepatitis in Seoul area. Korean J Intern Med. 1982. 25:19–26.
11. Choi W, Eom HS, Kim IH, Lee DH, Kim PS, Kim HG, Kwon KS, Cho HG, Shin YW, Kim YS. Patterns of acute hepatitis A and anti-HAV seroprevalence of Kyungin province. Korean J Gastroenterol. 1999. 34:69–75.
12. Sohn YM, Rho HO, Park MS. The changing epidemiology and hepatitis A in children and the consideration of active immunization in Korea. Yonsei Med J. 2000. 41:34–39.
13. Kang JH, Lee KY, Kim CH, Sim D. Changing hepatitis A epidemiology and the need for vaccination in Korea. Asian Pac J Allergy Immunol. 2004. 22:237–242.
14. Song MH, Lim YS, Song TJ, Choi JM, Kim JI, Jun JB, Kim MY, Pyun DK, Lee HC, Jung YH, Lee YS. The etiology of acute viral hepatitis for the last 3 years. Korean J Med. 2005. 68:256–260.
15. Lee TH, Kim SM, Lee GS, Im EH, Huh KC, Choi YW, Kang YW. Clinical features of acute hepatitis A in the western part of Daejeon and Chungnam province: single center experience. Korean J Gastroenterol. 2006. 47:136–143.
16. Han SH, Lee SH, Roh BJ, Shim SC, Cho SC, Sohn JH, Lee DH, Kee CS. An outbreak of hepatitis A in south Korean military personnel: a clinical and epidemiologic study. Korean J Hepatol. 2001. 7:392–400.
17. Lee SD. Asian perspectives on viral hepatitis A. J Gastroenterol Hepatol. 2000. 15:Suppl. 94–99.

18. Saab S, Lee C, Shapaner A, Ibrahim AB. Seroepidemiology of hepatitis A in patients with chronic liver disease. J Viral Hepat. 2005. 12:101–105.

19. Cooksley G. The importance and benefits of hepatitis A prevention in chronic liver disease patients. J Gastroenterol Hepatol. 2004. 19:Suppl. S17–S20.

20. Woo YS, Chung SH, Kim SK, Jang UI, Chung WC, Lee KM, Yang JM, Han JY, Lee YS, Chung KW, Seon HS. Fulminant hepatitis A associated with hepatorenal syndrome in asymptomatic chronic hepatitis B virus carrier. Korean J Hepatol. 2002. 8:Suppl 3. 120.
21. Reiss G, Keeffe EB. Review article: Hepatitis vaccination in patients with chronic liver disease. Aliment Pharmacol Ther. 2004. 19:715–727.
22. Lau DT, Hewlett AT. Screening for hepatitis A and B antibodies in patients with chronic liver disease. Am J Med. 2005. 118:Suppl 10. 28–33.

23. Saab S, Martin P, Yee HF Jr. A simple cost-decision analysis model comparing two strategies for hepatitis A vaccination. Am J Med. 2000. 109:241–244.

24. Lemon SM, Shapiro CN. The value of immunization against hepatitis A. Infect Agents Dis. 1994. 3:38–49.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download